
Volume 9 | Issue 3 August 2023 www.delamed.org | www.delawarepha.org A publication of the Delaware Academy of Medicine / Delaware Public Health Association Public Health Delaware Journal of Neurological Impairment and Stroke
Delaware Academy of Medicine
OFFICERS
Lynn Jones, L.F.A.C.H.E. President
Stephen C. Eppes, M.D. President Elect
Ann Painter, M.S.N., R.N. Secretary
Jeffrey M. Cole, D.D.S., M.B.A. Treasurer
S. John Swanson, M.D.
Immediate Past President
Timothy E. Gibbs, M.P.H. Executive Director, ex officio DIRECTORS
David M. Bercaw, M.D.
Saundra DeLauder, Ph.D.
Lee P. Dresser, M.D.
Eric T. Johnson, M.D.
Erin M. Kavanaugh, M.D.
Joseph Kelly, D.D.S.
Omar A. Khan, M.D., M.H.S.
Brian W. Little, M.D., Ph.D.
Daniel J. Meara, M.D., D.M.D.
John P. Piper, D.O.
Megan L. Werner, M.D., M.P.H.
Charmaine Wright, M.D., M.S.H.P.
EMERITUS
Barry S. Kayne, D.D.S.
Joseph F. Kestner, Jr., M.D.
Delaware Public Health Association
ADVISORY COUNCIL
Omar Khan, M.D., M.H.S. Chair
Timothy E. Gibbs, M.P.H. Executive Director
COUNCIL MEMBERS
Louis E. Bartoshesky, M.D., M.P.H.
Gerard Gallucci, M.D., M.S.H.
Allison Karpyn, Ph.D.
Erin K. Knight, Ph.D., M.P.H.
Melissa K. Melby, Ph.D.
Mia A. Papas, Ph.D.
Karyl T. Rattay, M.D., M.S.
William Swiatek, MA, A.I.C.P.
Delaware Journal of Public Health
Timothy E. Gibbs, M.P.H.
Publisher
Omar Khan, M.D., M.H.S.
Editor-in-Chief
Lee P. Dresser, M.D.
Guest Editor
Kate Smith, M.D., M.P.H.
Copy Editor
Suzanne Fields
Image Director

ISSN 2639-6378
Public Health Delaware Journal of
A publication of the Delaware Academy of Medicine / Delaware Public Health Association
3 | In This Issue
Omar A. Khan, M.D., M.H.S.; Timothy E. Gibbs, M.P.H.
4 | Guest Editor
Lee P. Dresser, M.D.
6 | Stroke Prevention
Bruce Dopler, M.D.
12 | Atrial Fibrillation: A Common Cause of Stroke
Waimei Tai, M.D., F.A.A.N., F.A.H.A.
16 | Stroke Systems of Care: A Systematic Approach to Saving Neurons
Kim Gannon, M.D., Ph.D., F.A.H.A.
20 | Medical Management of Acute Cerebral Ischemia
Usman Shehzad, M.D.
30 | Update on Neurointerventional Therapy for the Treatment of Acute Cerebral Ischemia
Sudhakar Satti, M.D.
Thinesh Sivapatham, M.D.
34 | Nursing Care of Delaware’s Stroke Patients
Reina W. McAndrew M.S., A.P.R.N., F.N.P.-B.C., S.C.R.N.
Mary Ciechanowski M.S.N., A.P.R.N., A.C.N.S.-B.C., C.C.R.N.-K.
38 | The Social Worker in The Care of The Stroke Patient
Annamarie McDermott, L.M.S.W., A.C.M.-S.W.
44 | Lessons on Health Literacy and Communication in Post-Stroke Rehabilitation: A Primer and Proposal
Christine V. Cook, M.A., C.C.C.-S.L.P.
Rebecca Hunting Pompon, Ph.D.
50 | Global Health Matters May/June 2023
Fogarty International Center
62 | Evaluation & Treatment of Psychological Effects of Stroke
Nancy Devereux Ph.D.
Ashley M. Berns Psy.D.
70 | Cognitive Rehabilitation Interventions for Post-Stroke Populations
Meghan Mulhern, M.A., C.C.C.-S.L.P.
76 | The Effects of Stroke and Stroke Gait Rehabilitation on Behavioral and Neurophysiological Outcomes: Challenges and Opportunities for Future Research
Trisha Kesar, P.T., Ph.D.
82 | Artificial Intelligence and the Evaluation and Treatment of Stroke
Lee P. Dresser, M.D.
Michael Anders Kohn, M.D., M.P.P.
86 | Lexicon & Resources
90 | The Nation Needs to Invest in Public Health Now
Timothy E. Gibbs, M.P.H.
Katherine Smith, M.D., M.P.H.
91 | Index of Advertisers
The Delaware Journal of Public Health (DJPH), first published in 2015, is the official journal of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA).

Submissions: Contributions of original unpublished research, social science analysis, scholarly essays, critical commentaries, departments, and letters to the editor are welcome.
Questions?
Contact managingeditor@djph.org
Advertising: Please contact tgibbs@delamed.org for other advertising opportunities. Ask about special exhibit packages and sponsorships. Acceptance of advertising by the Journal does not imply endorsement of products.
Copyright © 2023 by the Delaware Academy of Medicine / Delaware Public Health Association. Opinions expressed by authors of articles summarized, quoted, or published in full in this journal represent only the opinions of the authors and do not necessarily reflect the official policy of the Delaware Public Health Association or the institution with which the author(s) is (are) affiliated, unless so specified.
Any report, article, or paper prepared by employees of the U.S. government as part of their official duties is, under Copyright Act, a “work of United States Government” for which copyright protection under Title 17 of the U.S. Code is not available. However, the journal format is copyrighted and pages June not be photocopied, except in limited quantities, or posted online, without permission of the Academy/DPHA.Copying done for other than personal or internal reference use-such as copying for general distribution, for advertising or promotional purposes, for creating new collective works, or for resale- without the expressed permission of the Academy/DPHA is prohibited. Requests for special permission should be sent to managingeditor@djph.org
August 2023 Volume 9 | Issue 3



IN THIS ISSUE
Timothy E. Gibbs, M.P.H Publisher, Delaware Journal of Public Health
Doi: 10.32481/djph.2023.08.001 3
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
Interview with Two Delaware Stroke Survivors
Lee P. Dresser, M.D. General Neurologist, Wilmington Neurology Consultants; Chair, Delaware Stroke Initiative
Stroke affects every victim somewhat differently. The effects of stroke can be subtle or dramatic. Some people have no noticeable symptoms at all, and at the other end of the spectrum of severity, stroke can lead to sudden death or disabling neurologic deficits in an instant. Stroke can rob a neurologically normal person of the use of their limbs, their speech or vision and forever change their life. How stroke affects a person depends on many factors, including the location in the brain where the stroke occurs, the size of the stroke, the age of the victim and whether they have any preexisting medical problems or have had prior strokes.
Stroke is a large public health problem and thus a very fitting topic for the Delaware Journal of Public Health. In this issue, experts in the field of stroke share their expertise on many important aspects of this serious disease. Because the best stroke is the one that never occurs, Dr. Bruce Dopler details important prevention measures. Dr. Amy Tai discusses atrial fibrillation and how it is involved with stroke. We learn from Dr. Kim Gannon how the Delaware Stroke System of Care is designed and operates to allow optimal treatment for stroke victims in our state. Dr. Usman Shehzad reviews the critical topic of the evaluation and treatment of acute cerebral ischemic stroke. An update on the rapidly developing and exciting treatment modality of neurointerventional surgery is provided by Drs. Sudhakar Satti and Thinesh Sivapatham. The important role of the nurse in every aspect of stroke care is discussed by Ms. Mary Ciechanowski and Ms. Reina McAndrew. Ms. Annamarie McDermott does an excellent job describing the many contributions social workers make to the care of stroke patients during and after their hospital treatment. A discussion of the important topics of health literacy and aphasia in stroke is presented by Christine Cook and Dr. Rebecca Pompon. It is not often realized how common depression and anxiety are after stroke and Drs. Nancy Devereux and Ashley Berns contribute an excellent review on this topic. Similarly, cognitive problems such as memory loss and reduced executive functions may not be typically considered as symptoms of stroke but are common and important and are expertly reviewed by Dr. Meghan Mulhern. Problems with balance and leg strength and coordination lead to disabling loss of normal ambulation for many stroke survivors. Dr. Trisha Kesar provides current research on rehabilitation therapy for gait problems after stroke. Artificial intelligence (AI) currently impacts all of our lives on a daily basis and Dr. Michael Kohn and I give a brief review of the role of AI in the evaluation, treatment and rehabilitation of stroke.
Following is an interview with two prominent Delaware residents who are stroke survivors and brothers. Their experiences illustrate many important aspects of this common and very serious disease. It is hoped by sharing their stories that medical professionals will better be able to help prevent stroke and care for stroke victims.
In order to put a more personal face on stroke, two prominent lifelong Delawareans were kind enough to share their own experiences with this disease. Vance and Bill Funk are brothers who have each survived strokes, and their stories personify the significant yet different ways this can manifest and affect people’s lives. They were kind enough to sit down with me and share their experiences.
VANCE FUNK
Vance Funk was born December 16, 1942, in Philadelphia, Pennsylvania. He is the oldest of four children. He graduated from Salesianum High School and then earned a bachelor’s degree in business administration from the University of Delaware in 1965. Vance received his law degree from the Washington and Lee University School of Law in 1968. He was a lieutenant in the U.S. Army and served a year in the 519th MP Battalion in Vietnam during the war. He has practiced real estate law in Newark, Delaware since 1973.
In 1993, Vance was working full time in his legal practice and under some stress helping to care for his mother, who was suffering from dementia. Four weeks before his stroke, while testifying in court, he had complete loss of his vision. This persisted long enough to gain the notice of others, but it then returned as quickly as it had left. A subsequent examination by an eye doctor was unremarkable. But he remembers no one checked his blood pressure and as a healthy, very busy 50-year-old man, Vance was not regularly seeing a physician. If it had been checked, it is likely his blood pressure would have been found to be dangerously high. Days later, while walking to his car, he found he could not lift his arm to reach the door handle. Moments later he collapsed onto the ground.
Vance was rushed to the Christiana Hospital in Newark where he was found to have markedly elevated blood pressure, right sided paralysis, and the inability to talk. A CT scan of his head showed a large left hemisphere hemorrhage. He does not recall (when interviewed 30 years later) that he had any headache and, in fact, had never experienced a headache at any time in his life.
Vance was admitted to the intensive care unit, where his mother was also a patient, being treated for severe pneumonia. He survived to recount his story many years later, but sadly, his mother died from complications of her pneumonia without ever leaving the hospital. Vance was able to visit her one last time at her bedside but was too ill at the time to attend her funeral.
During his first few days of hospitalization, Vance had severe aphasia and lethargy. He recalls a physician saying in his room that people with strokes as severe as his had an “87% chance of
4 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.002
dying.” Vance advises all medical personnel caring for stroke and other severely ill patients to assume they can hear what is being said in their presence, and thus choose their words carefully. Fortunately, he did not require surgery for his cerebral hemorrhage and was eventually transferred to Wilmington Hospital, the old Delaware Division hospital, for rehabilitation therapy. There, he survived the complication of a deep venous thrombosis requiring the placement of an inferior vena cava filter. He was not a good candidate for anticoagulation due to his cerebral hemorrhage. After many days of hard work, Vance was able to return home and continue rehabilitation as an outpatient. He quickly regained the ability to speak. After four months he was able to return to practicing law.
Despite being left with prominent weakness in his right arm, Vance has been able to walk and speak well. He recalled that the only cars he could find with enough foot room to allow him to use his left leg to operate the accelerator and brake pedals were Buicks, and this quickly became his car of choice. Vance was so successful in his rehabilitation from his life-threatening stroke that in 2004 he was elected mayor of the City of Newark. He was re-elected three times and in his time in office enacted many programs to improve the quality of life for city residents.
Since his stroke Vance has had his blood pressure closely monitored and controlled with medication. He wishes he had had done so in the past, which may well have prevented his stroke. He strongly advises that people have their blood pressure periodically measured and that they follow the advice of their medical providers.
BILL FUNK
Many years later, Vance’s younger brother Bill also suffered a stroke. Bill Funk was born on December 11, 1949 and, like his older brother, graduated from Salesianum High School and the University of Delaware. He subsequently earned his medical degree from the Thomas Jefferson Medical School. Bill completed his family practice residency in Wilmington, Delaware and is a two-time president of the Delaware Board of Family Physicians.
In contrast to his brother, Bill had no obvious risk factors for stroke. He was an active runner, belonging to the local Pike Creek Valley Running Club, regularly completed five-kilometer races, and also ran a number of marathons, including the Boston Marathon. One morning in 2017, upon awakening Bill walked to the kitchen to make some coffee. He noted he had a left limp, but initially attributed this to his chronic sciatica which he had managed for years. When he could not use his left hand to pick up a coffee cup, he knew something was more seriously wrong. He limped back to his bedroom and shared his concerns with his wife, Linda. Familiar with his good sense of humor, she initially thought he was joking, but then noted a mild left facial droop and some slurred speech.
Since they live only five minutes from the Christiana Hospital in Newark, Linda drove Bill there, calling the Emergency Department while en route to alert them of their arrival. There his symptoms temporarily improved immediately after a CT angiogram of his head, but quickly recurred. He had no noted occlusion of his carotid arteries or of the intracranial arteries, but the CT and MRI scans of his brain showed an area of
acute infarction in the right hemisphere. Because Bill had his neurological symptoms upon awakening in the morning, he was not a candidate in 2017 for thrombolytic therapy (today, patients with “wake up strokes” can be evaluated emergently employing cerebral perfusion scanning and, if there is significant brain tissue at risk, may be treated with enzyme lytic therapy or interventional therapy in the presence of a large vessel occlusion).
During his hospitalization, Bill reported there was no clear cause discovered for his stroke, despite extensive laboratory testing, and vascular and cardiac imaging. After several days in Christiana Hospital following his stroke, he was transferred to Wilmington Hospital for seven days of rehabilitation therapy. Because he had been working full time as a physician prior to his stroke and very much wanted to return to work, Bill requested thorough cognitive testing be done as part of his rehabilitation to make sure he had no problems that might interfere with his return to practicing medicine. Fortunately, no deficits were detected. Shortly after beginning physical and occupational therapy, Bill was walking multiple lengths of the hall on the rehab floor. Bill believes he was aided significantly in his recovery from his stroke because he was quite fit from being a regular runner. One week after returning home from the hospital, he began seeing patients again by telemedicine and shortly thereafter returned to treating patients in person. Bill has continued to practice medicine up until the time of the interview for this article. He has been able to resume his running, and going on long walks with Linda. He reports that he received excellent care at Christiana Hospital during his acute treatment for his stroke and at Wilmington Hospital during his rehabilitation therapy. Bill believes he is a good example of how important it is to recognize the first symptoms of stroke, and to immediately seek medical care at an appropriate hospital. He recommends anyone with stroke symptoms call 911, and notes that the only reason Linda drove him to the emergency department instead of calling for help is because they live literally five minutes from the hospital.
The stories of the strokes suffered by Bill and Vance Funk point out how important it is for everyone to monitor their risk factors for stroke, especially blood pressure. Vance’s experience reminds us as medical professionals how important it is to choose our words carefully anytime we are in the presence of our patients, even if a patient may outwardly not appear to be able to comprehend what is being said about them. Although Bill was a very experienced physician in 2017, and very familiar with what to do when he had acute neurological problems, his story shows how important it is for us to educate all of our patients to call 911 should they or others in their presence suffer signs or symptoms of stroke. Dr. Dresser may be contacted at lpdresser@gmail.com
5
Stroke Prevention
Bruce Dopler, M.D. Neurologist, Neurology Center of South Delaware; Tidal Health Nanticoke
ABSTRACT
Stroke has three main subtypes - ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage. The most common stroke subtype is ischemic stroke, making up about 88% of strokes. Many of these strokes may be prevented by lifestyle modifications. These lifestyle modifications include engaging in physical activity, dietary changes such as the Mediterranean diet, smoking cessation, and avoiding substance abuse. Addressing medical conditions such as diabetes, hypertension, lipid management, sleep apnea, and atrial fibrillation will also have a major impact on stroke prevention. In addition to stroke prevention, these strategies help with overall brain health, which may also have an impact on neurological degenerative diseases such as Alzheimer’s disease.
INTRODUCTION
Each year it is estimated that approximately 800,000 individuals in the United States suffer a stroke. Stroke has three main subtypes - ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage. The most common stroke subtype is ischemic, making up about 88% of strokes. Ischemic stroke occurs by acute interruption of blood flow resulting in brain tissue injury. This is best visualized acutely on MRI diffusion weighted image sequences. A transient ischemic attack (TIA) is the same process without resulting tissue injury; therefore, no abnormality is seen on an MRI diffusion weighted image. Intracerebral hemorrhage, at approximately 10%, is the next most common stroke followed by subarachnoid hemorrhage at about 2%. Prevention strategies discussed in this article are going to be confined to the ischemic stroke subtype; however, risk factor modification strategies are oftentimes applicable to the other two stroke subtypes.1,2
There has been a trend towards reduction of stroke incidence from 8.7% in the 1960s to 5.0% in the 2000s. This is thought to be secondary to improved blood pressure control and the use of antiplatelet medications.1 The optimal stroke prevention strategy for an individual depends on the underlying etiology of their stroke. In general, management of vascular risk factors, including management of diabetes, smoking cessation, lipid management, hypertension management, as well as lifestyle modification provide the foundation for prevention of stroke. Lifestyle factors such as low-sodium, Mediterranean diet and physical activity may provide the greatest benefit for primary and secondary prevention. Addressing these factors also helps maintain optimal brain health.
PRIMARY PREVENTION
Primary prevention of stroke involves identification of specific factors associated with vascular disease. These include the presence or absence of diabetes, hypertension, current smoking, cholesterol, race, and sex. Cardiovascular risk assessment scores have been shown to be very useful for targeting individuals that are at risk for a stroke. One such tool is the American Heart Association/American College of Cardiology Vascular Risk calculator (ASCVD Risk Estimator Plus). This calculator uses age, sex, race, systolic and diastolic blood pressure, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein
(LDL), histor y of diabetes, smoking history, hypertension treatment, statin usage, and aspirin treatment to give a 10-year atherosclerotic cardiovascular disease risk score.3 This tool is oftentimes used to start a conversation with a patient to help with motivation in controlling these risk factors.
Physical Activity
Physical inactivity has been a well-defined and modifiable risk factor for cardiac disease and stroke. In the Northern Manhattan Stroke Study, a dose response relationship showing more intensive physical activity had greater stroke reduction compared to light and moderate physical activity. It is felt that exercise itself plays a part through potential factors such as anti-inflammatory effects, but also the modification of other associated risk factors such as reduction in blood pressure, body mass index (BMI), lipid levels and better diabetic control.4
Diet
Diet and nutritional studies have identified the protective effects from stroke by regular consumption of fish,5 high consumption of fruit and vegetables,6 following a Mediterranean diet,7 and the Dietary Approaches to Stop Hypertension (DASH) diet.8 The Mediterranean diet is high in the monounsaturated/saturated fat ratio, using olive oil as a main cooking ingredient. Consumption of other traditional foods high in monounsaturated fats such as tree nuts and other plant-based foods including fruits, vegetables, legumes whole grains, and cereals; increased consumption of fish; low consumption of meat and meat products; and discouraging the consumption of red and processed meats have been shown to be beneficial. Low alcohol consumption should be encouraged. The vascular-healthy diet moderates the consumption of milk and dairy products, and discourages soda drinks, pastries, sweets, commercial bakery products and spread fats. It also emphasizes consumption of less than 1500 mg of sodium per day. The reader is encouraged to go the American Heart Association website (https://www.heart.org) for further recommendations.
Tobacco
Tobacco use is the number one preventable cause of death in the United States and globally. Cigarette smoking is the most common form of tobacco use and is a major risk factor for stroke. Other forms of tobacco use are becoming increasingly popular. Electronic cigarette use has risen dramatically among young adults. Its use among young people has increased by 900% from
6 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.003
2011 to 2015. Compared to non-users e-cigarette users had higher adjusted odds of stroke.9 The risk of ischemic stroke has been estimated to be twofold higher in those individuals who smoke, and there is a threefold higher risk of subarachnoid hemorrhage. The risk of stroke is reduced when those individuals quit smoking. Between two to five years after cessation of smoking, the stroke risk approaches those who have never smoked.10
Substance Abuse
Alcohol consumption and ischemic stroke have a J-shaped relationship, regardless of sex. Stroke risk is increased with heavy alcohol consumption (greater than three drinks per day for men and greater than two drinks per day for women).11 It is recommended that patients with an ischemic stroke or TIA who drink more than two alcoholic drinks a day (men) or more than one alcoholic drink (women) be counseled to eliminate or reduce their consumption of alcohol to reduce stroke risk.1 Acute ischemic stroke hospitalization is higher among cannabis users, and the US Centers for Disease Control and Prevention identified that young adults with recent cannabis use have higher odds of stroke compared with nonusers.12 In patients with stroke or TIA who have a substance use disorder (drugs or alcohol), specialized services are recommended to help manage this dependency.
Diabetes
Diabetes is defined as a heterogeneous mix of health conditions characterized by blood glucose dysregulation. The most common forms are type 2 diabetes, which affects 90 to 95% of those with diabetes, and type 1 diabetes which constitutes 5 to 10%. Diabetes is defined as having a fasting glucose of greater than 126, a 2-hour post challenge glucose greater than 200, or a hemoglobin A1c greater than 6.5. Prediabetes is defined as a fasting glucose 100-125, 2-hour glucose test of 140-199, hemoglobin A1c of 5.7-6.4.
Type 1 diabetes is an autoimmune disorder that results in absolute insulin deficiency. Type 2 diabetes results from progressive impairment of insulin sensitivity and pancreatic insulin secretion. The pathophysiology of prediabetes is the same, with the only difference in the blood sugar level.
In Delaware, more than 98,000 individuals (about the seating capacity of the Los Angeles Memorial Coliseum), reported that they had been diagnosed with diabetes. In 2017, approximately 95,000 Delawareans reported that they had been diagnosed with prediabetes. Delaware’s prevalence of diagnosed diabetes, 13%, is greater than the national average of 11%.13 Diabetes prevalence is increasing in Delaware: from 2002 to 2019 Delaware’s adult diabetes prevalence rate rose from 8% to 13%, and at the projected rate it is estimated to be over 121,000 residents in the State of Delaware by 2030.14
Diabetes increases the risk of stroke nearly three-fold and disproportionately affects the elderly and minority population.15 The duration of diabetes increases the risk of stroke by 3% per year.16 Prediabetes is present in approximately 30% of patients with acute ischemic stroke.17 Progression of prediabetes to diabetes can often be prevented by diet, weight control and exercise.
Despite the fact that diabetes is a disease having its pathophysiological effects related to impaired blood glucose control, there has been extremely limited data to support
tight glucose control and the reduction of stroke risk for other cardiovascular events. In the Action to Control Cardiovascular Risk and type 2 Diabetes (ACCORD) study, patients with a mean hemoglobin A1c of 8.1% assigned to intensive glucose control with a target hemoglobin A1c of less than 6 were compared to a standard control group with hemoglobin A1c of 7.0-7.9. The study was stopped secondary to higher mortality rates in the intensive treated group. There was no difference in the risk of nonfatal stroke.18 Further studies are needed.
In patients who have had an ischemic stroke or TIA and have diabetes, the goal for glycemic control should be individualized. This should be based on the risk for adverse events, patient characteristics, and patient preferences. For most patients, achieving a hemoglobin A1c of 7% is recommended to reduce the risk of microvascular complications. The American Diabetes Association (ADA) have revised their algorithms for the management of type 2 diabetes. An evidence-based consensus report by the ADA and the European Association for the Study of Diabetes recommends metformin and comprehensive lifestyle changes as the first-line therapy.19 Because of new classes of glucose lowering medications that also prevent clinical vascular disease, the ADA recommends that in patients with ischemic strokes, glucagon-like peptide 1 (GLP-1) receptor agonists should be added to metformin, independent of baseline hemoglobin A1c. When concern for heart failure or chronic kidney disease predominates, the addition of a sodium glucose cotransporter 2 inhibitor to metformin is recommended. Through shared decision making, the treating provider should help the patient decide if the GLP–1 receptor agonist or the sodium glucose co-transporter 2 inhibitor is right for them. Costs, side effects, desired weight loss, aversion to injection therapy, and desire to reduce risk for hypoglycemia are factors that should be weighed in this discussion.
Hypertension
Hypertension is one of the most modifiable risk factors for ischemic and hemorrhagic stroke. Data from randomized clinical trials and large meta-analysis provide compelling evidence that neurologically stable patients with cerebrovascular disease benefit from a blood pressure goal of less than 130/80 mmHg, and that blood pressure targets for stroke prevention should be more aligned with targets for prevention of other cardiovascular conditions. Treatment of hypertension includes weight reduction, aerobic activity, dietary modification including daily sodium consumption of less than 1500 mg, and medications. Diuretics, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blocking medications have demonstrated benefit in multiple trials in stroke prevention. Calcium channel blockers are recommended to treat hypertension, but there is limited data on their efficacy for secondary stroke prevention. However, if the use of calcium channel blockers is reasonable for patients who are having uncontrolled hypertension, this may be an option.13,20 The Randomized Evaluation of Recurrent Stroke Comparing PFO Closure to Established Current Standard of Care Treatment (RESPECT) trial, Prevention After Stroke- Blood pressure (PASTBP) trial and the Prevention of Decline in Cognition After Stroke (PODCAST) trial compared intensive control of systolic blood pressure ranges from less than 120-130 mmHg with standard blood pressure control targets of less than 140-150 mmHg in patients with prior strokes. These trials all reported significant
7
tendencies toward lower recurrent stroke rates in the intensive treatment groups.21–23 The exception to this may be in those patients with significant small vessel disease and/or significant intracranial atherosclerotic disease.
The degree of blood pressure lowering appears to be more important for the risk reduction of stroke than the class of antihypertensive agent used.24 The recommended threshold of blood pressure greater than 130/80 mmHg for starting hypertensive medication is due to the baseline blood pressure in patients of cerebrovascular disease studied in the above mentioned trials. There are, however, some unanswered questions concerning blood pressure management. Optimal blood pressure target for the very elderly population and for those individuals with extensive small vessel disease is unknown. The optimal blood pressure target for patients with diabetes and stroke and the optimal timing to begin blood pressure lowering after stroke need further study.
Lipid Management
Most studies have found high total cholesterol to be a risk factor for ischemic stroke. In the multiple risk factor intervention trials comprised of greater than 350,000 participants, relative risk of death resulting from non-hemorrhagic stroke increased progressively with each higher level of serum cholesterol.25 In the women’s Pulling project, which included 24,000 US women less than 55 years of age with no previous cardiovascular disease, and the Women’s Health study, a prospective study of 27,000 US women greater than 45 years of age, higher cholesterol levels were associated with increased risk of ischemic stroke.26,27 However, in the Atherosclerotic Risk In the Community (ARIC) study of 14,000 middle-aged men and women free of cardiovascular disease, the relationship between lipid values and incident ischemic stroke was weak.28 The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial and the Treat Stroke to Target trial evaluated lipid lowering therapy in patients after ischemic stroke and found significant benefit from cholesterol-lowering therapy in preventing vascular events including stroke.29 SPARCL found atorvastatin 80 mg daily reduced stroke recurrence in patients without another indication for statin therapy. The Treat Stroke to Target trial confirmed that target LDL less than 70 was superior to target of 90-110 for preventing major cardiovascular events. These specific treatment trials and numerous other randomized clinical trials of lipid lowering drugs indicate that high risk patients with atherosclerotic cardiovascular disease should receive high intensity statin therapy. If the LDL-C remains greater than 70 on maximally tolerated statin therapy, it may be reasonable to add ezetimibe and then a PCSK9 inhibitor if the patient is deemed to be at very high risk.29 Accordingly, the 2018 American Heart Association/American College of cardiology guidelines on management of blood cholesterol for high intensity statin therapy recommend atorvastatin 80 mg daily or rosuvastatin 20 mg daily.1
Sleep Apnea
Sleep apnea is associated with an increased risk of cardiovascular disease and stroke. In a longitudinal study it was found that patients with severe obstructive sleep apnea doubled their risk of stroke.30 The ASA guidelines recommend patients with ischemic stroke or TIA and obstructive sleep apnea be treated with continuous positive airway pressure (CPAP). This can be beneficial for improved sleep apnea, blood pressure, sleepiness, and other apnea related outcomes. In addition, treatment of sleep apnea is felt to be important in maintaining overall good brain health.
Atrial Fibrillation
Nonvalvular atrial fibrillation (AF) is an important and treatable risk factor for stroke. In patients with nonvalvular AF and stroke or TIA, oral anticoagulation with apixaban, dabigatran, edoxaban, rivaroxaban or warfarin is recommended to reduce the risk of stroke, regardless of whether the AF is permanent, paroxysmal, or persistent. In patients with AF and stroke or TIA who do not have moderate to severe mitral stenosis or a mechanical heart valve, apixaban, dabigatran, edoxaban, or rivaroxaban, are recommended over warfarin to reduce the risk of stroke. These recommendations are made based on the evidence from four large, randomized trials comparing the direct oral anticoagulants versus the vitamin K antagonist, warfarin.31–34
There are other prevention strategies for specific stroke types that go beyond the scope of this article. The reader is advised to read the American Stroke Association guidelines, which are continually updated, for specific recommendations.
CONCLUSION
Risk factor modification is vital for both primary and secondary stroke prevention. In order to achieve this auspicious goal, clinicians and patients must work together to create a comprehensive prevention and treatment plan. Communicating the importance of lifestyle modification and medical compliance is vital. The rewards of successfully making these changes are great, not only in stroke prevention, but in improving overall brain health, and preventing cognitive decline and allowing patients to remain independent and productive.
Dr. Dopler may be contacted at bdopler@comcast.net
REFERENCES
1. Kleindorfer, D. O., Towfighi, A., Chaturvedi, S., Cockroft, K. M., Gutierrez, J., Lombardi-Hill, D., . . . Williams, L. S. (2021). AHA/ASA guideline for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke, 52(7), e364–e467. https://doi.org/10.1161/STR.0000000000000375
2 Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., . . . Tsao, C. W., & the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2020, March 3). Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation, 141(9), e139–e596 https://doi.org/10.1161/CIR.0000000000000757
3. Meschia, J. F., Bushnell, C., Boden-Albala, B., Braun, L. T., Bravata, D. M., Chaturvedi, S., Wilson, J. A., & the American Heart Association Stroke Council, & the Council on Cardiovascular and Stroke Nursing, & the Council on Clinical Cardiology, & the Council on Functional Genomics and Translational Biology, & the Council on Hypertension. (2014, December). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(12), 3754–3832. https://doi.org/10.1161/STR.0000000000000046
4. Sacco, R. L., Gan, R., Boden-Albala, B., Lin, I. F., Kargman, D. E., Hauser, W. A., Paik, M. C. (1998, February). Leisure-time physical activity and ischemic stroke risk: The Northern Manhattan Stroke Study. Stroke, 29(2), 380–387 https://doi.org/10.1161/01.STR.29.2.380
8 Delaware Journal of Public Health - August 2023
5 Zhao, W., Tang, H., Yang, X., Luo, X., Wang, X., Shao, C., & He, J. (2019, March). Fish consumption and stroke risk: A meta-analysis of prospective cohort studies. J Stroke Cerebrovasc Dis, 28(3), 604–611 https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.10.036
6. Aune, D., Giovannucci, E., Boffetta, P., Fadnes, L. T., Keum, N., Norat, T., . . . Tonstad, S. (2017, June 1). Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. International Journal of Epidemiology, 46(3), 1029–1056 https://doi.org/10.1093/ije/dyw319
7. Rees, K., Takeda, A., Martin, N., Ellis, L., Wijesekara, D., Vepa, A., . . . Stranges, S. (2019, March 13). Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev, 2019(3), CD009825. https://doi.org/10.1002/14651858.CD009825.pub3
8 Chiavaroli, L., Viguiliouk, E., Nishi, S. K., Blanco Mejia, S., Rahelić, D., Kahleová, H., Sievenpiper, J. L. (2019, February 5). DASH dietary pattern and cardiometabolic outcomes: An umbrella review of systematic reviews and meta-analyses. Nutrients, 11(2), 338 https://doi.org/10.3390/nu11020338
9. Ndunda, P. M., & Muutu, T. M. (2019, January). Abstract 9: Electronic cigarette use is associated with a higher risk of stroke. Stroke, 50(Suppl_1), A9 https://doi.org/10.1161/str.50.suppl_1.9
10. Pan, B., Jin, X., Jun, L., Qiu, S., Zheng, Q., & Pan, M. (2019, March). The relationship between smoking and stroke: A meta-analysis. Medicine, 98(12), e14872
https://doi.org/10.1097/MD.0000000000014872
11. Reynolds, K., Lewis, B., Nolen, J. D. L., Kinney, G. L., Sathya, B., & He, J. (2003, February 5). Alcohol consumption and risk of stroke: A meta-analysis. JAMA, 289(5), 579–588 https://doi.org/10.1001/jama.289.5.579
12. Parekh, T., Pemmasani, S., & Desai, R. (2020, January). Marijuana use among young (18-44 years of age) and stroke risk: A Behaviorial Risk Factor Surveillance System Survey analysis. Stroke, 51(1), 308–310. https://doi.org/10.1161/STROKEAHA.119.027828
13 Zonneveld, T. P., Richard, E., Vergouwen, M. D., Nederkoorn, P. J., de Haan, R., Roos, Y. B., & Kruyt, N. D. (2018, July 19). Blood pressure-lowering treatment for preventing recurrent stroke, major vascular events, and dementia in patients with a history of stroke or transient ischaemic attack. Cochrane Database Syst Rev, 2018(8), CD007858. https://doi.org/10.1002/14651858.CD007858.pub2
14 Delaware Department of Health and Human Services (2021, Jun). Impact of diabetes in Delaware. Retrieved from https://www.dhss.delaware.gov/dhss/dph/dpc/diabetes.html
15. Air, E. L., & Kissela, B. M. (2007, December). Diabetes, the metabolic syndrome, and ischemic stroke: Epidemiology and possible mechanisms. Diabetes Care, 30(12), 3131–3140 https://doi.org/10.2337/dc06-1537
16. Banerjee, C., Moon, Y. P., Paik, M. C., Rundek, T., MoraMcLaughlin, C., Vieira, J. R., Elkind, M. S. V. (2012, May). Duration of diabetes and risk of ischemic stroke: The Northern Manhattan Study. Stroke, 43(5), 1212–1217. https://doi.org/10.1161/STROKEAHA.111.641381
17 Kernan, W. N , Viscoli, C. M., Inzucchi, S. E., Brass, L. M., Bravata, D. M., Shulman, G. I., & McVeety, J. C. (2005, January 24). Prevalence of abnormal glucose tolerance following a transient ischemic attack or ischemic stroke. Archives of Internal Medicine, 165(2), 227–233 https://doi.org/10.1001/archinte.165.2.227
18. Gerstein, H. C., Miller, M. E., Byington, R. P., Goff, D. C., Jr., Bigger, J. T., Buse, J. B., . . . Friedewald, W. T., & the Action to Control Cardiovascular Risk in Diabetes Study Group. (2008, June 12). Effects of intensive glucose lowering in type 2 diabetes. The New England Journal of Medicine, 358(24), 2545–2559. https://doi.org/10.1056/NEJMoa0802743
19 Buse, J. B., Wexler, D. J., Tsapas, A., Rossing, P., Mingrone, G., Mathieu, C., Davies, M. J. (2020, February). 2019 Update to management of hyperglycemia in type 2 diabetes, 2018 a consensus report by the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care, 43(2), 487–493 https://doi.org/10.2337/dci19-0066
20. PROGRESS Collaborative Group. (2001, September). Randomised trial of perindopril-based blood-pressure lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet, 358(9287), 1033–1041. https://doi.org/10.1016/S0140-6736(01)06178-5
21 Kitagawa, K., Yamamoto, Y., Arima, H., Maeda, T., Sunami, N., Kanzawa, T., Shimada, K., & the Recurrent Stroke Prevention Clinical Outcome (RESPECT) Study Group. (2019, November 1). Effect of standard vs intensive blood pressure control on the risk of recurrent stroke: A randomized clinical trial and meta-analysis. JAMA Neurology, 76(11), 1309–1318 https://doi.org/10.1001/jamaneurol.2019.2167
22. Mant, J., McManus, R. J., Roalfe, A., Fletcher, K., Taylor, C. J., Martin, U., . . . Hobbs, F. D. R. (2016, February 24). Different systolic blood pressure targets for people with history of stroke or transient ischaemic attack: PAST-BP (Prevention After Stroke—Blood Pressure) randomised controlled trial. BMJ (Clinical Research Ed.), 352, i708. https://doi.org/10.1136/bmj.i708
23 Bath, P. M., Scutt, P., Blackburn, D. J., Ankolekar, S., Krishnan, K., Ballard, C., Ford, G. A., & the PODCAST Trial Investigators. (2017, January 17). Intensive versus guideline blood pressure and lipid lowering in patients with previous stroke: Main results from the pilot ‘prevention of decline in cognition after stroke trial’ (PODCAST) randomized control trial. PLoS One, 12(1), e0164608 https://doi.org/10.1371/journal.pone.0164608
24. Rashid, P., Leonardi-Bee, J., & Bath, P. (2003, November). Blood pressure reduction and secondary prevention of stroke and other vascular events: A systematic review. Stroke, 34(11), 2741–2748. https://doi.org/10.1161/01.STR.0000092488.40085.15
25 Iso, H., Jacobs, D. R., Jr., Wentworth, D., Neaton, J. D., & Cohen, J. D. (1989, April 6). Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. The New England Journal of Medicine, 320(14), 904–910 https://doi.org/10.1056/NEJM198904063201405
9
26 Horenstein, R. B., Smith, D. E., & Mosca, L. (2002, July). Cholesterol predicts stroke mortality in the Women’s Pooling Project. Stroke, 33(7), 1863–1868. https://doi.org/10.1161/01.STR.0000020093.67593.0B
27. Kurth, T., Everett, B. M., Buring, J. E., Kase, C. S., Ridker, P. M., & Gaziano, J. M. (2007, February 20). Lipid levels and the risk of ischemic stroke in women. Neurology, 68(8), 556–562. https://doi.org/10.1212/01.wnl.0000254472.41810.0d
28. Shahar, E., Chambless, L. E., Rosamond, W. D., Boland, L. L., Ballantyne, C. M., McGovern, P. G., & Sharrett, A. R., & the Atherosclerosis Risk in Communities Study. (2003, March). Plasma lipid profile and incident ischemic stroke: The Atherosclerosis Risk in Communities (ARIC) study. Stroke, 34(3), 623–631. https://doi.org/10.1161/01.STR.0000057812.51734.FF
29. Amarenco, P., Kim, J. S., Labreuche, J., Charles, H., Abtan, J., Béjot, Y., . . . Bruckert, E., & the Treat Stroke to Target Investigators. (2020, January 2). A comparison of two LDL cholesterol targets after ischemic stroke. The New England Journal of Medicine, 382(1), 9–19
https://doi.org/10.1056/NEJMoa1910355
30 Munoz, R., Duran-Cantolla, J., Martínez-Vila, E., Gallego, J., Rubio, R., Aizpuru, F., & De La Torre, G. (2006, September). Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke, 37(9), 2317–2321.
https://doi.org/10.1161/01.STR.0000236560.15735.0f
31 Connolly, S. J., Ezekowitz, M. D., Yusuf, S., Eikelboom, J., Oldgren, J., Parekh, A., Wallentin, L., & the RE-LY Steering Committee and Investigators. (2009, September 17). Dabigatran versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine, 361(12), 1139–1151. https://doi.org/10.1056/NEJMoa0905561
32. Patel, M. R., Mahaffey, K. W., Garg, J., Pan, G., Singer, D. E., Hacke, W., Califf, R. M., & the ROCKET AF Investigators. (2011, September 8). Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. The New England Journal of Medicine, 365(10), 883–891 https://doi.org/10.1056/NEJMoa1009638
33 Granger, C. B., Alexander, J. H., McMurray, J. J. V., Lopes, R. D., Hylek, E. M., Hanna, M., . . . Wallentin, L., & the ARISTOTLE Committees and Investigators. (2011, September 15). Apixaban versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine, 365(11), 981–992 https://doi.org/10.1056/NEJMoa1107039
34 Giugliano, R. P., Ruff, C. T., Braunwald, E., Murphy, S. A., Wiviott, S. D., Halperin, J. L., Antman, E. M., & the ENGAGE AF-TIMI 48 Investigators. (2013, November 28). Edoxaban versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine, 369(22), 2093–2104. https://doi.org/10.1056/NEJMoa1310907
Even the best rider is at the mercy of other drivers. If you go too fast, they may cut you off, change lanes, or make turns before they see you coming.
SO WATCH YOUR SPEED, WATCH OUT FOR OTHER DRIVERS, AND STAY SOBER.

10 Delaware Journal of Public Health - August 2023
ArriveAliveDE.com/Respect-The-Ride Life'stooshorttogo too fast
August 2023
The Nation’s Health headlines
Online-only news from The Nation’s Health newspaper

Stories of note include:
One year in, AmeriCorps boosts US public health workforce
Teddi Nicolaus
Legislators rolling back child labor protections
Kim Krisberg
State of emergency declared for LGBTQ+ people as rights eroded
Mark Barna
States embrace move to cover Medicaid users for a year after childbirth
Mark Barna
Summer Reads: Catch up on hot topics with these public health sizzlers
Kim Krisberg
Q&A: How commercial determinants of health worsen racial inequities
Minoli Ediriweera
Protecting people who have trouble fighting infections
Teddi Nicolaus
New APHA Press book explores reproductive justice for Black women

Mark Barna
Newsmakers: August 2023
Minoli Ediriweera https://www.thenationshealth.org/
HIGHLIGHTS FROM The NATION’S HEALTH A PUBLICATION OF THE AMERICAN PUBLIC HEALTH ASSOCIATION 11
Atrial Fibrillation: A Common Cause of Stroke
Waimei Tai, M.D., F.A.A.N., F.A.H.A. Vascular Neurologist, ChristianaCare Neurology Specialists
ABSTRACT
Atrial fibrillation is the culprit causal mechanism of twenty percent of acute ischemic strokes. As the population of Delaware ages, atrial fibrillation is a growing cause of stroke. Thus, the detection of atrial fibrillation and treatment of this cardioembolic risk factor of stroke is paramount.
ATRIAL FIBRILLATION DEFINITIONS
Atrial fibrillation (AF) is a type of cardiac arrhythmia characterized by irregular and often rapid electrical activity in the atria. During AF, the atria quiver instead of contracting normally, which can lead to an irregular heart rate and inefficient blood flow. AF can be classified into four types, by duration and if it is recurrent or sustained1:
1. Paroxysmal AF: AF that comes and goes on its own, typically lasting less than 7 days.
2. Persistent AF: AF that continues for longer than 7 days, or requires medical intervention to terminate.
3. Long-standing persistent AF: AF that lasts for more than 12 months.
4. Permanent AF: AF that is present and accepted as a permanent condition, and efforts to restore normal rhythm have been discontinued.2
AF can occur in individuals with underlying heart disease, such as hypertension, coronary artery disease, or heart failure, or it can occur in individuals without any known underlying heart disease. AF can be asymptomatic or may cause symptoms such as palpitations, shortness of breath, chest discomfort, and fatigue.3
ATRIAL FIBRILLATION EPIDEMIOLOGY
Atrial fibrillation (AF) is the most common arrhythmia in the United States, affecting approximately 2.7 million Americans. The prevalence of AF increases with age, with 5% of individuals over the age of 65 and 10% of those over the age of 80 having this condition.4
The incidence of AF is also increasing, with an estimated 160,000 new cases diagnosed each year. This increase is likely due to the aging population and the increasing prevalence of risk factors such as hypertension, obesity, and diabetes.5 AF is more common in men than women, and in individuals of European descent compared to other racial and ethnic groups. However, it is important to note that AF can occur in anyone, regardless of age, gender, or ethnicity.6
AF is associated with an increased risk of stroke, heart failure, and mortality. The burden of AF on the healthcare system is significant, with estimated costs of over $26 billion annually in United States.1 AF contributes to more than 20% of acute ischemic strokes.7
EVALUATION AND DETECTION OF ATRIAL FIBRILLATION
For patients with acute ischemic stroke, evaluation for occult AF is important. This should include electrocardiographic monitoring in the hospital for at least 24 hours.8 For patients with a cryptogenic stroke who do not have a contraindication to anticoagulation, further testing with outpatient remote monitoring should be considered to evaluate for occult AF. Remote monitoring options include outpatient telemetry or an implantable cardiac monitor.
A 2016 randomized controlled trial showed AF in 30% of 221 patients with implantable cardiac monitors and in 3% of 220 control patients after 36 months of follow-up (hazard ratio 8.8; 95% CI = 3.5-22.2; P <0.0001).9 It is unknown whether this monitoring with subsequent initiation of oral anticoagulants in affected patients will lower the rate of subsequent stroke, but it is now routine practice to offer prolonged cardiac monitoring for patients with embolic stroke of unknown source (ESUS type stroke).10
The American Heart Association/American Stroke Association (AHA/ASA) guidelines for stroke prevention in patients with previous stroke do not recommend an echocardiogram for all patients. However, they do advise that an echocardiogram be obtained for patients with cryptogenic stroke of unknown source to evaluate for structural heart pathology.10 While transthoracic echocardiography (TTE) alone may not definitively predict the occurrence of AF, certain echocardiographic features have been associated with an increased risk of AF. These features include left atrial enlargement, left ventricular dysfunction, increased left ventricular mass, valvular heart disease, diastolic dysfunction, and left atrial appendage dysfunction.11
TREATMENT OPTIONS FOR ATRIAL FIBRILLATION
After the diagnosis of AF is made, it is important to decide who to treat with anti-coagulants. The CHA2DS2-VASc score is used to calculate the risk of ischemic stroke in patients with AF (Table 1).12 For patients with nonvalvular AF, a CHA2DS2-VASc score of 2 or greater, and an acceptably low risk of bleeding, the 2019 AHA/ACC/Hearth Rhythm Society (HRS) guidelines for AF management suggest that the use of direct-acting oral anticoagulants (DOACs)-is preferable (Table 2).13 For stroke prevention in these patients, recommended DOACs include apixaban (Eliquis, 5 mg 2 times/day), dabigatran (Pradaxa, 150 mg 2 times/day), and rivaroxaban (Xarelto, 20 mg once daily).14
12 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.004
CHA2DS2-VASc = congestive heart failure, hypertension, age ≥75 years (doubled), diabetes mellitus, prior stroke or TIA or thromboembolism (doubled), vascular disease, age 65 to 74 years, sex category; MI = myocardial infarction; PAD = peripheral artery disease; TIA = transient ischemic attack.
For patients with AF who need anticoagulation and who are also on hemodialysis, apixaban would be the novel oral anticoagulant of choice. The recommended dosage is 5 mg 2 times/day, with a dosage reduction to 2.5 mg 2 times/day for patients 80 years and older and with a body weight of 60 kg/132.28 lb or less.3 Controversy exists as to whether any anticoagulant should be used in patients receiving dialysis given other risks of bleeding. Shared decision-making should be used in prescribing these drugs.13 The AHA/ACC/HRS guidelines suggest that warfarin or apixaban can be used in patients with end-stage renal disease.
The HAS-BLED (hypertension, abnormal liver/renal function, stroke, bleeding tendency/predisposition, labile INR, elderly [older than 65 years], drug/alcohol concomitantly) score can be used to calculate the risk of rebleeding in patients with a history of bleeding (Table 3 and Table 4).16 It has been validated in patients taking warfarin but has not been studied in patients taking DOACs. If the annual risk of bleeding is higher than the annual risk of ischemic stroke, alternative stroke prophylaxis should be discussed with the patient and considered.13
Table 3, HAS-BLED Score to Estimate Bleeding Risk in Anticoagulated Patients With Atrial Fibrillation16
aData from the Friberg validation study, but in general would assume the higher the score, the higher the risk of ischemic stroke. CHA2DS2-VASc = congestive heart failure, hypertension, age ≥75 years (doubled), diabetes mellitus, prior stroke or TIA or thromboembolism (doubled), vascular disease, age 65 to 74 years, sex category.
The criteria for modified dosages vary by drug. A reduced dosage of apixaban (2.5 mg 2 times/day) is recommended if two of three criteria are met: creatinine level of 1.5 mg/dL or greater, age 80 years or older, and body weight of 60 kg/132.3 lb or less. A reduced dosage of dabigatran (75 mg 2 times/ day) is recommended for patients with a creatinine clearance of 15 to 30 mL/minute. A reduced dosage of rivaroxaban (15 mg once daily) is recommended for patients with a creatinine clearance of 50 mL/min or less.
Shared decision-making is indicated when prescribing these drugs, with patient preference, cost, and adherence being considerations.13,14 Patients taking warfarin require regular monitoring to achieve and maintain a therapeutic INR. Warfarin is associated with substantial drug-drug interactions but its effects can be rapidly reversed. The DOACs have simpler dosing than warfarin.15 Dabigatran, rivaroxaban, and apixaban appear to have similar effectiveness, although apixaban may be associated with lower bleeding risk and rivaroxaban may be associated with higher bleeding risk. Drugs to reverse the effects of DOACs now are available for emergency use.15
ALT = alanine aminotransferase; AP = alkaline phosphatase; AST = aspartate aminotransferase; Cr = creatinine; HAS-BLED = hypertension, abnormal liver/renal function, stroke, bleeding tendency/ predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly; INR = international normalized ratio; NSAIDs = nonsteroidal antiinflammatory drugs; ULN = upper limits of normal.
aData are limited, but a score >5 is thought to be associated with a high
13
Risk Factor (score if yes) Number of Points Congestive heart failure history 1 Hypertension history 1 Age ≥75 years 2 Diabetes history 1 Stroke/TIA/thromboembolism history 2 Vascular disease history (prior MI, PAD) 1 Age 65-74 years 1 Sex category - female 1 Age <65 years 0
Table 1. CHA2DS2-VASc Score to Estimate Stroke Risk in Patients with Atrial Fibrillation12
Score Risk of Ischemic Stroke (Event/Hundred Years at Risk)a 0 0.2 1 0.6 2 2.2 3 3.2 4 4.8 5 7.2 6 9.7 7 11.2 8 10.8a 9 12.2
Table 2. CHA2DS2-VASc Score Interpretation
Risk Factor Number of Points Hypertension (uncontrolled, >160 mm Hg systolic) 1 Renal disease (Cr level >2.26 mg/dL, dialysis or transplant) 1 Liver disease (cirrhosis or bilirubin >2x ULN with AST/ALT/AP >3x ULN) 1 Stroke history 1 Prior major bleeding or predisposition to bleeding 1 Labile INR (unstable INR, time in therapeutic range <60%) 1 Elderly (age >65 years) 1 Drugs (predisposing to bleeding [aspirin, clopidogrel, NSAIDS]) 1 Alcohol (≥8 drinks/week) 1
Score Annual Risk of Major Bleeding (%) Recommendation 0 0.9 Anticoagulation can be considered 1 3.4 2 4.1 3 5.8 More frequent monitoring and review of risk factors. Alternative to anticoagulation can be considered 4 8.9 5 9.1 >5 >10a
Table 4. HAS-BLED Score Interpretation17,18
of
risk
bleeding.
Patients with AF who cannot undergo anticoagulation may be considered for placement of a left atrial appendage device, closure device, or surgical ligation of the left atrial appendage.13,14 Use of a closure device has been found to be noninferior compared with a DOAC in preventing a composite of stroke, transient ischemic attack (TIA), embolism, mortality, and bleeding in patients with AF.19
For patients who recently had stroke due to AF, the question when to re-initiate anti-coagulation often occurs. One recent large observational trial, the ELAN study, looked at this question.20 Small stroke was defined as <1.5 cm size stroke. Moderate size stroke was one superficial branch occlusion. Large stroke was defined as involving one branch or more, or a >1.5cm infarct in the brainstem. The early group started anticoagulation in 48 hours for small/moderate strokes and on day 6-7 for large strokes. The late group had initiation of a DOAC in participants with a minor stroke on day 3 or 4 after stroke onset, in moderate strokes on day 6-7, and in participants with a major stroke on day 12-14. This study suggests that early re-initiation of anticoagulation is safe and better at preventing recurrent ischemic stroke (1.4% vs 2.5% in the late initiation group), without significant added burden of hemorrhage (0.2% in both groups).
In summary, recognition of AF and appropriate treatment of this risk factor is important in the prevention of acute ischemic stroke in the aging population.
Dr. Tai may be contacted at waimei.a.tai@christianacare.org
REFERENCES
1. January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland, J. C., Jr., . . . Yancy, C. W., & the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. (2014, December 2). 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 64(21), e1–e76. https://doi.org/10.1016/j.jacc.2014.03.022
2 American Heart Association. (2021). What is atrial fibrillation (AFib or AF)? Retrieved from https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrialfibrillation-afib-or-af
3. National Heart, Lung, and Blood Institute. (2011). What is atrial fibrillation? Retrieved from https://www.nhlbi.nih.gov/health-topics/atrial-fibrillation
4 Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., . . . Turner, M. B., & the Writing Group Members, & the American Heart Association Statistics Committee, & the Stroke Statistics Subcommittee. (2016, January 26). Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation, 133(4), e38–e360 https://doi.org/10.1161/CIR.0000000000000350
5 Colilla, S., Crow, A., Petkun, W., Singer, D. E., Simon, T., & Liu, X. (2013, October 15). Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. The American Journal of Cardiology, 112(8), 1142–1147 https://doi.org/10.1016/j.amjcard.2013.05.063
6 Schnabel, R. B., Yin, X., Gona, P., Larson, M. G., Beiser, A. S., McManus, D. D., Levy, D. (2015, July 11). 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. Lancet, 386(9989), 154–162.
https://doi.org/10.1016/S0140-6736(14)61774-8
7. Sposato, L. A., Cipriano, L. E., Saposnik, G., Ruíz Vargas, E., Riccio, P. M., & Hachinski, V. (2015, April). Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: A systematic review and meta-analysis. Lancet Neurol, 14(4), 377–387
https://doi.org/10.1016/S1474-4422(15)70027-X
8 Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., . . . Tirschwell, D. L. (2019, December). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 50(12), e344–e418.
https://doi.org/10.1161/STR.0000000000000211
9 Brachmann, J., Morillo, C. A., Sanna, T., Di Lazzaro, V., Diener, H. C., Bernstein, R. A., . . . Passman, R. S. (2016, January). Uncovering atrial fibrillation beyond short-term monitoring in cryptogenic stroke patients: Three-year results from the cryptogenic stroke and underlying atrial fibrillation trial. Circ Arrhythm
Electrophysiol, 9(1), e003333
https://doi.org/10.1161/CIRCEP.115.003333
10 Kleindorfer, D. O., Towfighi, A., Chaturvedi, S., Cockroft, K. M., Gutierrez, J., Lombardi-Hill, D., . . . Williams, L. S. (2021, July). 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/ American Stroke Association. Stroke, 52(7), e364–e467
https://doi.org/10.1161/STR.0000000000000375
11 Verdecchia, P., Reboldi, G., Gattobigio, R., Bentivoglio, M., Borgioni, C., Angeli, F., Porcellati, C. (2003, February). Atrial fibrillation in hypertension: Predictors and outcome. Hypertension, 41(2), 218–223.
https://doi.org/10.1161/01.HYP.0000052830.02773.E4
12. Lip, G. Y., Nieuwlaat, R., Pisters, R., Lane, D. A., & Crijns, H. J. (2010, February). Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest, 137(2), 263–272
https://doi.org/10.1378/chest.09-1584
13 January, C. T., Wann, L. S., Calkins, H., Chen, L. Y., Cigarroa, J. E., Cleveland, J. C., Jr., Yancy, C. W. (2019, July 9).
2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation, 140(2), e125–e151
https://doi.org/10.1161/CIR.0000000000000665
14 Delaware Journal of Public Health - August 2023
Meschia, J. F., Bushnell, C., Boden-Albala, B., Braun, L. T., Bravata, D. M., Chaturvedi, S., Wilson, J. A., & the American Heart Association Stroke Council, & the Council on Cardiovascular and Stroke Nursing, & the Council on Clinical Cardiology, & the Council on Functional Genomics and Translational Biology, & the Council on Hypertension (2014, December). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(12), 3754–3832.
https://doi.org/10.1161/STR.0000000000000046
15. Noseworthy, P. A., Yao, X., Abraham, N. S., Sangaralingham, L. R., McBane, R. D., & Shah, N. D. (2016, December). Direct comparison of dabigatran, rivaroxaban, and apixaban for effectiveness and safety in nonvalvular atrial fibrillation.
Chest, 150(6), 1302–1312
https://doi.org/10.1016/j.chest.2016.07.013
16 Pisters, R., Lane, D. A., Nieuwlaat, R., de Vos, C. B., Crijns, H. J., & Lip, G. Y. (2010, November). A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest, 138(5), 1093–1100.
https://doi.org/10.1378/chest.10-0134
17. Lip, G. Y., Frison, L., Halperin, J. L., & Lane, D. A. (2011, January 11). Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: The HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. Journal of the American College of Cardiology, 57(2), 173–180.
https://doi.org/10.1016/j.jacc.2010.09.024
18 Lip, G. Y. (2011, February). Implications of the CHA(2) DS(2)-VASc and HAS-BLED Scores for thromboprophylaxis in atrial fibrillation. The American Journal of Medicine, 124(2), 111–114. https://doi.org/10.1016/j.amjmed.2010.05.007
19. Osmancik, P., Herman, D., Neuzil, P., Hala, P., Taborsky, M., Kala, P., . . . Reddy, V. Y., & the PRAGUE-17 Trial Investigators. (2020, June 30). Left atrial appendage closure versus direct oral anticoagulants in high-risk patients with atrial fibrillation. Journal of the American College of Cardiology, 75(25), 3122–3135
https://doi.org/10.1016/j.jacc.2020.04.067
20 Fischer, U., Koga, M., Strbian, D., Branca, M., Abend, S., Trelle, S., . . . Dawson, J., & the ELAN Investigators. (2023, June 29). Early versus later anticoagulation for stroke with atrial fibrillation. The New England Journal of Medicine, 388(26), 2411–2421
https://doi.org/10.1056/NEJMoa2303048

15 14
Immunization Summit 2023 Thursday, December 7, 2023 1pm-6pm Bally’s Dover Casino Resort (Dover Downs) 1131 N. Dupont Hwy, Dover SAVE THE DATE Online registration and additional details soon at immunizedelaware.org
Stroke Systems of Care: A Systematic Approach to Saving Neurons
Kim Gannon, M.D., Ph.D., F.A.H.A. ChristianaCare Neurosciences
ABSTRACT
Stroke continues to be a major public health concern, accounting for more than 800,000 strokes per year and remains the leading cause of disability. Stroke systems of care are comprehensive frameworks designed to ensure efficient and effective management of stroke patients. This article provides a brief overview of the coordinated network of healthcare providers, emergency medical services, and hospitals working together to deliver timely and specialized care including pre-hospital care, acute hospital care, rehabilitation, and community reintegration.
The author wishes to give special thanks to Ron Brown B.S., N.R.P., Account Executive - Air Methods; Paul Westlake, Public Health Treatment Program Administrator and Systems of Care Coordinator; and John Roussis, MBA,CMTE, NRP, FP-C, Director of Pre-Hospital Services CareNet/LifeNet/ Transfer Center/ Mobile Integrated Health Paramedics for their assistance with State data collection and fact checking.
INTRODUCTION
Stroke continues to be the 5th leading cause of death and the leading cause of disability in the United States. This burden is significant – one stroke every 40 seconds in the United States, and one death from stroke every four minutes, totaling about 800,000 initial or recurrent strokes per year. The total cost of stroke is estimated to climb to $143 BILLION by 2035. Not only does this burden of stroke affect the individual, but also the family and care providers for this individual.1 While interventions for detection and treatment of stroke have improved significantly over the past decade, systems of care surrounding stroke patients have improved identification and access to the right treatment at the right time. The American Stroke Association (ASA) first published recommendation in 2005 for the establishment of systems of care for stroke, followed by expansion in 2013 and updates in 2019.2 Improving systems of care and improving access to care improves outcomes and prolongs healthy lives. Standards and systems impact outcomes – the American Heart Association’s (AHA) “Get with the Guidelines” led to an 8% reduction in mortality and improved functional outcome at discharge.3
Key stakeholders in stroke systems of care consist of roles in the pre-hospital, acute care, and post-hospital setting including rehabilitation centers as well as primary care and ambulatory neurology. Acute care healthcare providers include physicians representing the emergency department, vascular and general neurology, neurointerventional surgery, neurosurgery, neuroradiology, and hospitalists. The acute care team also relies on highly qualified nurses, pharmacists, therapists, and stroke center coordinators. Post discharge coordination relies on acute and subacute rehabilitation, physiatry and therapy teams along with social workers to ensure continued care. Coordination and collaboration of these teams are essential to ensure optimal care.
The AHA and the Centers for Disease Control and Prevention (CDC) have published recommendations for establishing systems of care for optimal stroke management that include legislation, prehospital care, inter-facility transfer, and acute hospital care, as well as post-hospital discharge.
ROLE OF STATE LEGISLATION
Delaware passed state legislation establishing the State Stroke Committee and the State System of Care in 2016. This collaboration represents ongoing work across our state including all non-government hospital systems. The Delaware State Stroke Committee represents the Joint Commission designated Comprehensive Stroke Center at ChristianaCare - Newark, and Primary Stroke Centers at Bayhealth Kent Campus, Bayhealth Sussex Campus, Beebe Healthcare, ChristianaCare - Wilmington Hospital, Saint Francis Healthcare, and Tidal Health – Nanticoke. State laws that support stroke systems of care can facilitate stroke care by providing a framework for collaboration and standardization of best practices.
A key aspect of stroke systems of care is continuous quality improvement, including tracking outcomes and identifying areas for improvement in stroke care delivery. State registries are used to collect data on stroke patients, track outcomes, and identify areas where care can be improved. This information is used to standardize best practices and ensure adherence to established standards of care. Shared learnings and adhering to standards of care reduces mortality rates, minimizes long-term disability, and improves quality of life for stroke survivors.3,4 The Delaware State Stroke Committee meets regularly for continuous quality improvement review and standardization.
PRE-HOSPITAL CARE
Prehospital care is essential for identification and urgent routing of patients, relying on emergency medical services and flight center coordination of care, along with transportation and safety authorities. The prehospital care starts at the location of the patient – in the community. The AHA has worked to inform the public of signs and symptoms of acute stroke using the acronym “FAST,” which stands for “Facial weakness,” “Arm drift or weakness,” “Speech abnormality,” and “Time to call 911.”4 This quick and easy to remember acronym summarizes some of the major symptoms associated with stroke. Despite the efforts, more work needs to be done regarding public education and the importance of immediately seeking care for any symptoms of acute stroke. Optimal care for stroke must be accurate and speedy – after all, time is brain!
16 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.005
The Delaware State Stroke Committee has developed policy for standards of care for stroke in the state, including working with legislation to ensure systematic routing policies. Over the past year, the team has revised the recommended systematic approach to the stroke evaluation by the Emergency Medical Services (EMS) teams prehospital. The VAN score, which quickly assess Vision, Aphasia, and Neglect, has been adopted for quick field assessment of stroke symptoms concerning for large vessel occlusion.5 The EMS team communicates directly with emergency physicians at the nearest emergency department who guide routing to the nearest appropriate facility based on the symptoms that the patient is experiencing. When appropriate, the EMS team can call for air support directly to the scene –significantly improving outcomes, specifically for patients who have symptoms of a large vessel occlusion. Helicopter transport has improved transport capabilities and significantly decreased time from EMS patient retrieval to treatment at the correct facility, especially for more rural locations.6 An alternative to air transport is Mobile Stroke Units (MSU) – ambulances with a CT scanner and ability to administer IV thrombolytics. MSUs have been changing the landscape of stroke care since 2008.7,8 This type of specialized ambulance originated in Germany with a goal of bringing stroke care to the patient – improving thrombolysis times and overall improving stroke outcome. Over the next decade, MSUs have expanded to over 25 sites around the world. The rig not only includes CT scanner technology, but also has the ability to perform point-of-care lab tests, routine medications, and IV thrombolytics (Alteplase/tPA or Tenecteplase/TNK), and is staffed by EMS personnel, a radiology technician, a nurse, and a neurologist – either on board or available via telemedicine.9 While Delaware does not currently have a Mobile Stroke Unit, this could be an opportunity to improve care for patients that are far from a stroke center.
The overall goal of pre-hospital and acute stroke care is to decrease the time between stroke onset to stroke treatment, which can be accomplished by decreasing the time between symptom identification and EMS activation, or EMS activation and medical treatment. While the MSU takes the hospital to the patient, other technologies can be used to improve the readiness of the hospital to receive the patient, thus speeding up decision making abilities once the patient arrives to the Emergency Department (ED). Sussex and Kent County EMS teams have adopted a prehospital communication technology, Twiage®, to alert accepting hospitals of pertinent information prior to hospital arrival. New Castle County has started using Twiage® for cardiac events and is planning to implement this technology for stroke care. This pre-hospital alert notification has been a game-changer in the ability of the acute hospital team to be prepared for the patient with the right team and tools in place to treat the patient emergently. Pre-hospital notification allows the ED team to alert the Stroke Neurology team before the patient arrives and allows time to review medications and any other past medical history stored in the electronic medical record that would impact patient treatment. By having this information prior to the patient’s arrival, systems of care have been able to reduce the door to treatment time by 18 minutes, and ensure that IV thrombolytics are not given to patients with contraindications. Every minute delay causes 12 million brain cells to die – prehospital notification is estimated to save more than 225 million brain cells for each patient!10
INTERFACILITY TRANSFER
Interfacility transfer is a crucial aspect of stroke care as it allows patients to receive specialized treatment and rehabilitation services that may not be available at their local hospital. Since 2019, the ChristianaCare LifeNet Air Medical team has placed an “EZ button” in the ED of many Delaware hospitals. This quick access technology notifies ChristianaCare LifeNet’s Air Medical Dispatch Center to place a helicopter resource on standby. The Air Medical Dispatch team starts to source a helicopter to transfer to the scene of the pressed button even before the clinician speaks to an accepting hospital. This has substantially decreased the time required to source transit for the patient. While the clinician’s attention is on the patient, the air command team is working to provide transit capabilities. This rapid access to interfacility transport significantly decreases delays in care. ChristianaCare LifeNet Air Medical has provided 215 flights for Neurologic care over the past 12 months, with 115 of these resulting from activation of the EZ button. This link in the State System of Care has significantly reduced not only the “door in, door out” time, but also improved the speed of interfacility transfer overall for our state.
However, transfer can also be associated with increased costs, longer hospital stays, and decreased quality of life for patients and their families. To minimize the negative effects of interfacility transfer, a triage system can be implemented to keep patients as close to home as safely possible. This system involves evaluation of the patient’s medical history, physical condition, and current symptoms to determine the appropriate level of care. Patients with mild to moderate strokes could receive treatment at their local hospital, while those with more severe strokes or who need surgical intervention may require transfer to a higher level of care. Determining which patients will benefit prior to transfer can facilitate keeping patients at their home institution.3,4 Developing telemedicine programs, providing community-based rehabilitation services, and educating healthcare providers on the latest stroke care guidelines can also facilitate keeping patients at their local healthcare facilities. Delaware has implemented these strategies so that stroke patients can receive timely and appropriate care while minimizing the negative effects of interfacility transfer.
ACUTE HOSPITAL CARE
The ED plays a critical role in acute stroke care, with protocols designed to ensure rapid triage and timely interventions. Decreasing goal times for each step of acute stroke care – including door to triage, triage to imaging, imaging to interpretation, and interpretation to intervention – all work to reduce the time between symptom onset and definitive treatment. Team members involved in ED acute stroke care include nursing, physicians, pharmacy, clerks/registration team, CT techs, radiology, and others - each vital link in this sequenced chain of events helps to ensure efficient and effective care.11 To decrease door to needle time, small things like delaying lab draws or using blood drawn by EMS, delaying EKG, not changing the patient into a gown, and removing jewelry prior to imaging can all work to improve treatment times. Access to artificial intelligence (AI) enabled imaging, such as RAPID AI®, allows for more expeditious treatment of patients. Not only does this type of technology reduce time to treatment and improve outcomes, but also allows
17
for streamlined communications across systems to allow for more expeditious transfer.12 Many Delaware hospitals are using RAPID AI® technology for image review. Utilization of this technology allows for expeditious review of images and decision making for transfer to a higher level of care for emergent intervention. Using imaging tools empowers physicians to make faster more accurate decisions for treatment.
ED treatment of patients with stroke has been revolutionized over the past decade by the increase in telemedicine. Even pre-COVID, stroke care was being provided by telemedicine. Telemedicine allows the neurologist with stroke expertise to be virtually present at bedside nearly immediately in the ED. Prior to the utilization of telemedicine, physicians relied on a reported examination by a physician who may or may not have expertise in the neurologic examination. By personally visualizing the patient, the neurologist can ask questions, go with the patient to CT and review any changing examination findings. This continued virtual presence allows for ongoing rapid decision making and communication with the nursing team at bedside. Telemedicine is one more way that Neurology has leaned on technology to expedite acute stroke care.4
Choice of medication has impacted the speed of interfacility transfer, as well as door to needle times. Recent data has supported transition from Alteplase (tPA) to Tenecteplase (TNK) for IV lytic management of acute ischemic stroke. This transition facilitates improved times for interfacility transfer given the one dose medication for TNK compared to the infusion “drip and ship” model required by tPA.13 In the past two years, substantial data has developed safety standards for IV thrombolytic therapy; not only is TNK easier to use with equitable, if not superior safety data, but it is also cheaper to dose. The medication itself is about $2000 less costly, but also does not require additional utilization of tubing, IV Saline and an IV pump.13 The movement to TNK has been a game changer for systems across the State of Delaware.
POST-HOSPITAL CARE
Post-hospital follow up is just as important in the stroke system of care as inpatient care. It has been suggested that patients are brought into the hospital in a Ferrari but sent out with a parachute – alluding to the lack of outpatient follow up and support available to patients post-stroke. After optimal hospital treatment, many stroke patients are discharged to acute or subacute rehabilitation. It is incumbent on the discharging facility to provide the appropriate information to continue optimal care while in the rehabilitation facility. Ambulatory follow up with neurology is sometimes part of the patient’s care plan, especially if the etiology of stroke remains unknown. However, there are some settings in which follow up with a stroke neurologist is not needed – specifically if the etiology of stroke is known. Other providers are key in post-stroke care outside of neurology. Primary care physicians and advanced practice providers are instrumental in the Stroke System of Care by encouraging patients to continue secondary prevention of stroke, including medications, management of comorbidities, and lifestyle modification. Physical medicine and rehab / physiatry specialists are key to a patient’s rehabilitation journey. The expertise they provide assists patients on the road to recovery and enables them
to achieve mobility post-stroke. Psychiatry and psychology can also play a key role in helping patients recover from stroke. The psychologic challenges faced by patients and family can be better met with support from specialists. Many stroke patients face depression during their recovery – this is especially prevalent in the population of young stroke patients. The overall goal of poststroke care is prevention of recurrent stroke and recurrent need for hospitalization, and the return of a patient to as near their prior baseline as possible.
CONCLUSION
Implementation of a Stroke System of Care establishes a systematic approach to stroke and enables our teams to work together for the best outcomes of the patient. Together, we work to decrease the time from symptom onset to treatment by utilizing community education, EMS partnerships, technology implementation and acute hospital care. We work to provide the right care in the right location at the right time, and provide expeditious transfer when required. Delaware Stroke System of Care provides access to the highest quality treatment and recovery options and is committed to continued excellence in the future.
Dr. Gannon may be contacted at kim.p.gannon@christianacare.org
REFERENCES
1. Gorelick, P. B., Furie, K. L., Iadecola, C., Smith, E. E., Waddy, S. P., Lloyd-Jones, D. M., . . . Zerna, C., & the American Heart Association/American Stroke Association. (2017, October). Defining optimal brain health in adults: A presidential advisory from the American Heart Association/American Stroke Association. Stroke, 48(10), e284–e303.
https://doi.org/10.1161/STR.0000000000000148
2. Adeoye, O., Nyström, K. V., Yavagal, D. R., Luciano, J., Nogueira, R. G., Zorowitz, R. D., . . . Jauch, E. C. (2019, July). Recommendations for the establishment of stroke systems of care: A 2019 update. Stroke, 50(7), e187–e210
https://doi.org/10.1161/STR.0000000000000173
3 Centers for Disease Control and Prevention. (2021, Jul). Stroke systems of care: Framework resources.
https://www.cdc.gov/dhdsp/programs/framework_resources.htm
4 Centers for Disease Control and Prevention. (2018). What is the evidence for state laws to enhance in-hospital and posthospital stroke care? A policy evidence assessment report. Atlanta, GA: Centers for Disease Control and Prevention.
https://www.cdc.gov/dhdsp/pubs/docs/Pre-Hospital_Post-Hospital_ Stroke_PEAR-508.pdf
5. Birnbaum, L., Wampler, D., Shadman, A., de Leonni Stanonik, M., Patterson, M., Kidd, E., . . . Miramontes, D. (2021, June). Paramedic utilization of Vision, Aphasia, Neglect (VAN) stroke severity scale in the prehospital setting predicts emergent large vessel occlusion stroke. Journal of Neurointerventional Surgery, 13(6), 505–508
https://doi.org/10.1136/neurintsurg-2020-016054
6 Jauch, E. C., Schwamm, L. H., Panagos, P. D., Barbazzeni, J., Dickson, R., Dunne, R., . . . Yallapragada, A., & the Prehospital Stroke System of Care Consensus Conference. (2021, May).
Recommendations for Regional Stroke Destination Plans in Rural, Suburban, and Urban Communities From the
18 Delaware Journal of Public Health - August 2023
Prehospital Stroke System of Care Consensus Conference: A Consensus Statement From the American Academy of Neurology, American Heart Association/American Stroke Association, American Society of Neuroradiology, National Association of EMS Physicians, National Association of State EMS Officials, Society of NeuroInterventional Surgery, and Society of Vascular and Interventional Neurology: Endorsed by the Neurocritical Care Society. Stroke, 52(5), e133–e152
https://doi.org/10.1161/STROKEAHA.120.033228
7 Fassbender, K., Merzou, F., Lesmeister, M., Walter, S., Grunwald, I. Q., Ragoschke-Schumm, A., Grotta, J. (2021, May 25). Impact of mobile stroke units. Journal of Neurology, Neurosurgery, and Psychiatry, 92(8), 815–822. https://doi.org/10.1136/jnnp-2020-324005
8. Harris, J. (2021, September). A review of mobile stroke units. Journal of Neurology, 268(9), 3180–3184. https://doi.org/10.1007/s00415-020-09910-4
9. Navi, B. B., Audebert, H. J., Alexandrov, A. W., Cadilhac, D. A., & Grotta, J. C., & the PRESTO (Prehospital Stroke Treatment Organization) Writing Group. (2022, June). Mobile stroke units: Evidence, gaps, and next steps. Stroke, 53(6), 2103–2113
https://doi.org/10.1161/STROKEAHA.121.037376
10 Kim, S. K., Lee, S. Y., Bae, H. J., Lee, Y. S., Kim, S. Y., Kang, M. J., & Cha, J. K. (2009, December). Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. European Journal of Neurology, 16(12), 1331–1335.
https://doi.org/10.1111/j.1468-1331.2009.02762.x
11 Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., Tirschwell, D. L. (2019, December). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 50(12), e344–e418
https://doi.org/10.1161/STR.0000000000000211
12 Cirio, J. J., Ciardi, C., Buezas, M., Diluca, P., Caballero, M. L., Lopez, M., Lylyk, P. (2021). Implementation of artificial intelligence in hyperacute arterial reperfusion treatment in a comprehensive stroke center. Neurol Argentina, 13(4), 212–220.
https://doi.org/10.1016/j.neuarg.2021.07.003
13. Warach, S. J., Dula, A. N., Milling, T. J., Miller, S., Allen, L., Zuck, N. D., Paydarfar, D. (2022, December). Prospective observational cohort study of tenecteplase versus alteplase in routine clinical practice. Stroke, 53(12), 3583–3593
https://doi.org/10.1161/STROKEAHA.122.038950
Delaware Journal of Upcoming Issues
Public Health
Each year, the Delaware Journal of Public Health publishes five different theme issues. Article submissions are accepted on a rolling basis, and the editorial board considers all submissions, both those connected directly to a theme issue, and non-thematic submissions. The editorial board reserves the right to include non-thematic submissions in each issue.
The working publishing calendar and thematic issues for 2023 are as follows:
If you have questions about submissions, ideas for an article, or suggestions for a future theme issue, please email managingeditor@djph.org
All submissions can be submitted via the online submission portal: https://www.surveymonkey.com/r/2DSQN98 Submissions guidelines can be found at: https://djph.org
19
Issue Submission Publication Oral Health March 2023 April 2023 Homelessness April 2023 May 2023 Neurological Impairment/Stroke July 2023 September 2023 Bio Tech/Research September 2023 October 2023 Health Policy/Ethics November 2023 December 2023
Medical Management of Acute Cerebral Ischemia
Usman Shehzad, M.D.
Vascular Neurologist, Bayhealth Medical Center; Chair, Stroke System of Care, Delaware
ABSTRACT
This review article discusses medical management of acute cerebral ischemia including recent advances. Expansion of the thrombolysis eligibility criteria are discussed. Tenecteplase as a promising new thrombolytic is explored and the evidence supporting the use of Mobile Stroke Units is presented.
INTRODUCTION
Stroke remains a leading cause of serious long-term disability in the United States, with more than 795,000 individuals suffering from a stroke every year.1 More than 160,000 deaths occur annually with stroke as the underlying cause and in 2020, stroke was responsible for approximately 1 out of 21 deaths in the nation.1 Within Delaware, 3135 strokes were reported in the calendar year 2022.2 While the term stroke encompasses both hemorrhagic and acute ischemic strokes (AIS), the latter is the most common stroke type accounting for 87% of all strokes.1 For the purpose of this review, stroke is used interchangeably with AIS. It must be noted that tremendous leaps have been made in the interventional/surgical management of AIS and are discussed elsewhere in this issue. This review will focus on the medical management of acute cerebral ischemia.
HYPERACUTE ASSESSMENT OF STROKE PATIENTS
Optimal management of stroke requires efficient delivery of care starting from the moment a patient recognizes their stroke symptoms and contacts Emergency Medical Services (EMS). Routing of the patient to a correct medical facility is of critical importance and is discussed in the stroke systems of care article published in this issue. Upon arriving at the emergency room (ER), multidisciplinary care is required to ensure there are no delays in the delivery of care to these patients as early treatment is shown to result in the best outcomes possible.3 Many events need to occur in parallel on patient arrival as initially their airway, breathing and circulation (ABCs) are assessed. A focused physical examination, as well as obtaining the National Institute of Health Stroke Scale (NIHSS), occurs as the patient is being rushed to the CT scanner for head and neck imaging. Review of imaging, focused history taking, and obtaining collateral information need to occur simultaneously as the nursing staff draws blood, obtains intravenous (IV) access, weighs the patient, records an EKG, connects the patient to telemetry monitoring, etc. Given the complexity of assessment and the need for efficiency, the American Heart Association (AHA) Stroke guidelines recommend an organized protocol for the emergency evaluation of patients with suspected stroke, as well as designation of an acute stroke team that includes physicians, nurses, and laboratory/ radiology personnel.3
The phrase “time is brain” was coined by Dr. Camilo R. Gomez in 1993 to signify the importance of timely intervention in stroke management4 and in 2005, Dr. Jeffrey Saver provided quantification of this concept by showing that a typical stroke patient loses 1.9 million neurons each minute in which stroke is left untreated.5 Therefore, optimizing stroke pathways must be made a high priority for any healthcare system providing acute stroke treatment.
Early review and management of vital signs, EKG changes, and laboratory abnormalities play an important role in the assessment of acute stroke patients. Allowing for permissive hypertension is the norm, though it is not known what blood pressure range produces the best outcome for stroke patients, and these decisions should be made on a case-by-case basis. Hypotension and hypovolemia should be corrected to maintain systemic perfusion levels necessary to support vital organs. For patients that are eligible for thrombolysis, the blood pressure should be <185 mm Hg systolic and <110 mm Hg diastolic. Hypoglycemia (blood glucose < 60 mg/dL) should be corrected in patients presenting with stroke symptoms. Of note, in patients that are eligible for thrombolysis, finger stick glucose is the only lab work that is required prior to thrombolytic administration, unless the patient has a known condition necessitating blood work such as underlying coagulopathy, thrombocytopenia, etc.3
Head positioning, particularly the benefits of laying flat as opposed to elevated head positioning, are not well studied. A single large trial studying this practice found no difference in outcome for patients with flat head positioning vs. elevated head positioning. The trial had many limitations, but importantly concluded that there was no increase in risk of aspiration pneumonia with flat head positioning.6 Thus, this decision should also be made on a case-by-case basis.
INTRAVENOUS THROMBOLYSIS
tPA Development and Initial Approval
IV thrombolysis was first reported in literature in 1958 when Drs. Sussman and Fitch published a case series of three patients treated with IV infusion of fibrinolysin.7 Trials testing different candidates for thrombolysis became more frequent in the 1980s with urokinase and streptokinase being the most widely studied drugs. In 1991, mass production of recombinant tissue plasminogen activator (tPA) began.8 tPA is a naturally occurring
20 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.006
protease that lyses blood clots by attaching to fibrin found on the surface of the clot and activation of plasminogen, which in turn produces plasmin leading to clot lysis . Recombinant technology has allowed for the creation of modified versions of tPA, such as alteplase, reteplase, and tenecteplase. These modified versions of tPA have slightly different properties, such as their ability to bind to fibrin and their half-life.9 Alteplase was the first modified version of tPA to be studied.
The National Institute of Neurological Disorders and Stroke (NINDS) published a landmark trial in 1995 that showed the effectiveness of alteplase for the treatment of acute ischemic stroke in patients who were able to be treated within 180 minutes of their last known well time.10 The trial had two parts:
• Part 1 tested whether alteplase was more effective than placebo at improving the NIHSS score at 24 hours. The NIHSS is a scale that measures the severity of stroke symptoms.
• Part 2 tested whether alteplase was more effective than placebo at improving clinical outcomes at three months. Clinical outcomes were measured using the Berthel Index, modified Rankin Scale (mRS) (Table 1), Glasgow Outcome Scale, and NIHSS.
Part 1 of the trial did not show a significant difference between alteplase and placebo. However, Part 2 of the trial showed that alteplase was more effective than placebo at improving clinical outcomes at three months. The global odds ratio for a favorable outcome including mRS score of 0 or 1 was 1.7, meaning that patients who received alteplase were 70% more likely to have a favorable outcome than patients who received placebo (Figure 1).
The administration of alteplase did result in an increased risk of symptomatic intracranial hemorrhage (sICH). The incidence of sICH was 6% in the alteplase arm as compared to 0.6% in the placebo arm. The study authors concluded that “despite an increased incidence of symptomatic intracerebral hemorrhage, treatment with intravenous alteplase within three hours of the onset of ischemic stroke improved clinical outcome at three months.” The results of this trial led to the ultimate approval by the Food and Drug Administration (FDA) of alteplase for use in acute ischemic strokes within 180 minutes of last known well in March 1996.11v
The European Cooperative Acute Stroke Study (ECASS) III trial was published in September 2008.12 This trial tested the efficacy of alteplase compared to placebo in patients treated 3-4.5 hours from their last known well times. The primary endpoint of the study was disability at 90 days, as measured by the mRS (Table 1). A favorable outcome was defined as an mRS score of 0 or 1. The odds ratio for a favorable outcome with alteplase was 1.28 compared to placebo. The incidence of sICH was higher with alteplase than with placebo. In this trial, 2.4% of patients who received alteplase experienced sICH, compared to 0.2% of patients who received placebo. The results of the ECASS III trial suggest that alteplase can be an effective treatment for acute ischemic stroke when given within 3-4.5 hours of the last known well time. While the FDA has not approved alteplase in the 3-4.5 hour time window, several organizations, including the American Heart Association/American Stroke Association have recommended using it in this time frame.3
Given the significant risks of hemorrhage associated with alteplase use, it is of critical importance to be familiar with the exclusion criteria for IV thrombolysis. The initial alteplase contraindications strictly adhered to the exclusion criteria in the above-mentioned trials. Over time, these exclusion criteria have become less restrictive as more evidence has shown favorable risk-to-benefit profiles in some of the situations where alteplase administration was previously an absolute contraindication. As an example, patients who had seizure at the onset of stroke were excluded from the NINDS trial and stroke guidelines that were published in 1996 recommended against giving alteplase in this scenario.13 Whereas, the most recent stroke guidelines state “IV alteplase is reasonable in patients with a seizure at the time of onset of acute stroke if evidence suggests that residual impairments are secondary to stroke and not a postictal phenomenon.”3 It is important to note that despite an increase in utilization of IV thrombolysis, reported incidence of sICH from alteplase use in recent studies is much lower than the NINDS trial summarized above.14
Extending the tPA Window
In addition to the exclusion criteria becoming less restrictive, there has been an effort to safely expand thrombolysis eligibility by using what is referred to as the “tissue window” in patients that cannot be treated using the “time window.” It was hypothesized that advanced imaging parameters can be used to determine eligibility for thrombolysis in patients presenting with stroke symptoms outside of the 4.5-hour time window. The research supporting this concept culminated in the publication of two trials discussed next.
In 2018, Thomella and colleagues published the WAKE-UP trial15 in which they used Magnetic Resonance Imaging (MRI) to guide treatment. While a detailed discussion on MRI sequences is beyond the scope of this article, Figure 2 provides a brief overview of MRI sequences relevant to this research. WAKE-UP trial investigators selected patients with a large DWI signal (tissue at risk of infarction) who had little or no FLAIR signal (already infarcted tissue) and randomized them to receive alteplase or placebo. This trial showed that patients who received alteplase based on the imaging criteria were more likely to have an MRS of 0 or 1 compared to placebo with the odds ratio of 1.61. Death or dependency at 90 days was numerically higher in the placebo group (18.3% vs 13.5%); death at 90 days was numerically higher
21
Description
The patient has no residual symptoms.
Table 1. Modified Rankin Scale (mRS) Score, a Scale to Assess the Degree of Disability after Stroke
Score
0
1 The patient has no significant disability; able to carry out all pre-stroke activities. 2 The patient has slight disability; unable to carry out all pre-stroke activities but able to look after self without daily help
3 The patient has moderate disability; requiring some external help but able to walk without the assistance of another individual 4 The patient has moderately severe disability; unable to walk or attend to bodily functions without assistance of another individual
in the alteplase group (4.1% vs 1.2%) but neither of these reached statistical significance. Rate of sICH was numerically higher in the alteplase group (2% vs 0.4%), however, this did not reach statistical significance either.
In 2019 Ma and colleagues published the EXTEND trial16 in which MRI or Computed Tomography Perfusion (CTP) scans were used to determine patient eligibility for thrombolysis. CTP is an imaging technique in which IV iodinated contrast bolus is administered and rapid sequential scans are obtained to assess the blood perfusion status of the brain parenchyma, pertinent sequences are described in Figure 3. Similar in concept to the DWI/ FLAIR discussion above, if the CTP showed a mismatch

between Tmax > 6 seconds and CBF < 30%, the patient was eligible for enrollment in the trial. The EXTEND trial also concluded that patients who received alteplase using imaging criteria were more likely to have minimal or no disability (mRS 0 or 1) at 90 days with an adjusted risk ratio of 1.44 compared to placebo. Death within 90 days and rates of sICH were numerically higher in the alteplase group, but this did not reach statistical significance.
Based on the WAKE-UP trial, the AHA added a Level IIa recommendation supporting the use of alteplase in patients selected using MRI guidance3; the EXTEND trial results did not get released in time for consideration by the guidelines committee.

22 Delaware Journal of Public Health - August 2023
Figure 1. Modified Rankin Scale Score Distribution at 90 Days for Patients Treated with Alteplase Compared to Placebo for Acute Ischemic Stroke. Image created using data from the NINDS tPA trial10
Figure 2. A Brief Description of Select MRI Sequences
ACUTE TREATMENT OF MILD NON-DISABLING STROKE
In 2016, Messé and colleagues used the Get With the Guidelines registry to determine common causes for otherwise eligible patients to not receive IV alteplase.17 “Rapid improvement or mild stroke” was most commonly documented as a cause for withholding alteplase, sighted in 51.4% of the cases. At the time, the AHA stroke guidelines indicated uncertainty regarding using alteplase in patients with low NIHSS scores and non-disabling deficits. This was only a Class IIB (weak) recommendation with quality of evidence level C-LD (limited data).18
This led to the design of the PRISMS trial in which investigators sought to test efficacy and safety of alteplase in suspected stroke patients who presented with minor deficits.19 Patients were enrolled if they had an NIHSS score ≤ 5 and a mild nondisabling deficit. The determination of non-disabling was made in consultation with the patients and available family members. Patients were randomized to receive alteplase or aspirin 325 mg, and the primary outcome was mRS score of 0 or 1 at 90 days. Alteplase was not shown to increase the likelihood of favorable functional outcome at 90 days in this study.
The more recently published ARAMIS trial was designed to investigate whether dual antiplatelet therapy (DAPT) was noninferior to alteplase in patients presenting with minor nondisabling strokes.20 DAPT in this trial was defined as aspirin 100 mg daily as well as clopidogrel 300 mg on day 1 followed by 75 mg daily. Eligible patients were randomized to be treated with either alteplase or DAPT and the primary endpoint was excellent functional outcome (defined as mRS score of 0 or 1) at 90 days. The study succeeded in showing that DAPT is non-inferior to alteplase in achieving excellent functional outcome at 90 days in patients presenting with minor, non-disabling strokes.
The most recent AHA guidelines added a new recommendation stating that for otherwise eligible patients with mild nondisabling stroke symptoms, alteplase is not recommended.3 Since what constitutes disabling is a subjective matter, it is prudent to include the patient and their family in determining severity of their presenting symptoms.
Tenecteplase for Thrombolysis in Acute Stroke
Tenecteplase is a genetically modified variant of alteplase optimized to have increased fibrin specificity. Additionally, tenecteplase has a longer half-life than alteplase, meaning it can be given as a single injection whereas alteplase must be given as a bolus followed by an infusion. The latest AHA stroke guidelines state that “tenecteplase might be considered as an alternative to alteplase in patients with minor neurological impairments and no major intracranial occlusions.”3 However, these guidelines predate the release of recent compelling data supporting the use of tenecteplase.

The larger early trials testing efficacy of tenecteplase were included in a meta-analysis by Drs. Burgos and Saver.21 The meta-analysis included five randomized trials enrolling 1585 patients. As there was not an established therapeutic dose of tenecteplase, there was a variety of doses used in these five trials. The primary outcome of this meta-analysis was a mRS score of 0 or 1 after 90 days. This endpoint was reached in 57.9% of the patients treated with tenecteplase and 55.4% of the patients treated with alteplase. The authors concluded that tenecteplase was non-inferior to alteplase for the treatment of acute ischemic stroke. Subgroup analysis looking at the doses tested showed that only the patients treated with 0.25 mg/kg and 0.4 mg/kg doses met the primary outcome.
Two recent trials have provided more information regarding tenecteplase dosing. The AcT trial was a non-inferiority trial in which patients eligible for thrombolysis were randomly assigned to receive either the standard dose of alteplase or tenecteplase 0.25 mg/kg.22 This trial showed that 0.25 mg/kg dose of tenecteplase “is a reasonable alternative to alteplase for all patients presenting with acute ischemic stroke who meet standard criteria for thrombolysis.”
NOR-TEST 2 was a non-inferiority trial in which patients eligible for thrombolysis received either standard dose of alteplase or 0.4 mg/kg dose of tenecteplase.23 The trial was stopped early for safety reasons and showed that “tenecteplase at a dose of 0.4 mg/ kg yielded worse safety and functional outcomes compared with alteplase.” Thus, the current practice in most centers is to use 0.25 mg/kg dose of tenecteplase.
23
Figure 3. A Brief Description of Select CTP Sequences
One subgroup of stroke patients in which tenecteplase has been shown to be superior to alteplase are the patients that are eligible for both IV thrombolysis and mechanical thrombectomy. The EXTEND-IA TNK trial enrolled such patients and randomized them to receive standard dose of alteplase or 0.25 mg/kg dose of tenecteplase.24 Patients in the tenecteplase arm were twice as likely to have substantial reperfusion before thrombectomy (22% vs 10%). Additionally, secondary analysis showed that the median mRS at 90 days for tenecteplase treated patients was 2 compared to a median mRS of 3 for the alteplase treated group. This has led to a level IIb recommendation by the AHA that it may be reasonable to choose tenecteplase over alteplase in patients who are also eligible to undergo mechanical thrombectomy.3
PATIENTS OUTSIDE THE TPA WINDOW
While the importance of thrombolysis cannot be overstated, it is important to recognize that almost 90% of the patients that present to the hospital with stroke symptoms are not candidates for IV thrombolysis.9 Early treatment for these patients starts with the initial evaluation and correction of blood glucose, blood pressure, and other measures outlined above.
Early antiplatelet therapy (initiated within 48 hours) with aspirin25,26 or clopidogrel27 has been shown to be beneficial for patients presenting with acute ischemic stroke. In patients presenting with mild stroke symptoms, a limited course of dual antiplatelet therapy with aspirin and clopidogrel was shown to be superior to single antiplatelet therapy in the CHANCE and POINT trials.28,29 Mild strokes in these trials were defined as those patients that presented with NIHSS ≤ 3 or those with high risk Transient Ischemic Attack (TIA) defined as ABCD2 score of ≥ 4. ABCD2 is a score that takes into account the patient’s age, blood pressure, clinical features, duration, and presence of diabetes to stratify patients into low, medium or high risk for recurrence of stroke. While both of these trials administered DAPT for different durations, a meta-analysis of these two trials showed that the benefit of DAPT was confined to the first 21 days after the minor stroke or high-risk TIA.30 Thus in patients with mild ischemic strokes or high risk TIAs, a 21-day course of DAPT should be used unless contraindicated.
Other than these initial management decisions, a thorough investigation into determining the stroke etiology is critical. While it may be over simplified, the TOAST trial’s classification of stroke subtypes is a good starting point.31 TOAST categorized stroke etiology into the following five categories: large-artery atherosclerosis, cardioembolism, small-vessel occlusion, stroke of other determined etiology, and stroke of undetermined etiology. Once a stroke is categorized into one of these general categories, risk factors specific to the individual patient can be identified and treated appropriately based on best evidence.
MOBILE STROKE UNIT
As emphasized throughout this article, timely stroke care is of the utmost importance to ensure best outcomes for patients. In addition to optimizing stroke care after a patient’s arrival to the emergency room, a Mobile Stroke Unit (MSU) can bring the “emergency room” to the patient. The concept of MSU was introduced by Dr. Fassbender and colleagues in 2003.32 They proposed designing a vehicle capable of carrying all the relevant personnel, equipment and diagnostic tools
(including a CT scanner) required for safe administration of IV thrombolysis in the field prior to bringing the patient to the ER. Since then, this proposed vehicle has been developed, deployed and studied extensively. A meta-analysis of the published studies comparing MSU and conventional stroke treatment showed that compared with usual care, MSU use was associated with a 30 minute reduction in stroke onset to IV thrombolysis administration and a 65% increase in the odds of excellent outcome (mRS 0 or 1 at 90 days).33 While implementation of an MSU is a costly undertaking, studies have shown MSU use to be cost effective considering internationally accepted thresholds and associated with higher quality adjusted life years (QALY)34–36
FUTURE DIRECTIONS
The past decade has seen an increase in the speed of evolution of stroke care as interventional management of stroke, improvements in medical management as well as improvement in stroke rehabilitation has led to overall declines in death and Disability Adjusted Life-Years (DALY) resulting from stroke.37 There are ongoing studies looking to expand the inclusion criteria for IV thrombolysis even further such as in the patients taking direct oral anticoagulants.38 Other studies are evaluating the combination of IV antiplatelets such as eptifibatide and argatroban with thrombolysis to improve reperfusion.39 Mobile Stroke Units have the potential to significantly improve outcomes for stroke patients. However, there are financial (appropriate reimbursement) and logistical challenges (development of optimal deployment protocols in different geographical locations) that need to be addressed before mobile stroke units can be widely implemented. Combining acute stroke treatment with neuroprotection has thus far been unsuccessful however the advent of endovascular therapies has brought renewed interest in this field.40
CONCLUSION
In patients presenting with acute ischemic stroke, rapid evaluation and efficient decision making is of utmost importance to improve patient outcomes. Expansion in the thrombolysis eligibility criteria by elimination of some previous contraindications and development of new selection criteria in the extended time window has allowed for more patients to be treated with IV thrombolysis. Furthermore, the advent of Mobile Stroke Units has brought a new paradigm to the treatment of AIS patients.
Dr. Shehzad may be contacted at usman_shehzad@bayhealth.org
REFERENCES
1. Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., . . . Martin, S. S., & the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2023, February 21). Heart disease and stroke statistics-2023 update: A report from the American Heart Association. Circulation, 147(8), e93–e621. https://doi.org/10.1161/CIR.0000000000001123
2. Westlake, P. (2023, July 19). Delaware Stroke System of Care Presentation [Quarterly Meeting].
24 Delaware Journal of Public Health - August 2023
3. Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., . . . Tirschwell, D. L. (2019, December). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 50(12), e344–e418.
https://doi.org/10.1161/STR.0000000000000211
4. Gomez, C. R. (1993). Editorial: Time is brain! J Stroke Cerebrovasc Dis, 3(1), 1–2.
https://doi.org/10.1016/S1052-3057(10)80125-9
5. Saver, J. L. (2006, January). Time is brain—Quantified. Stroke, 37(1), 263–266.
https://doi.org/10.1161/01.STR.0000196957.55928.ab
6. Muñoz-Venturelli, P., Arima, H., Lavados, P., Brunser, A., Peng, B., Cui, L., . . . Anderson, C. S., & the HeadPoST Collaborative Investigators. (2015, June 5). Head Position in Stroke Trial (HeadPoST)—sitting-up vs lying-flat positioning of patients with acute stroke: Study protocol for a cluster randomised controlled trial. Trials, 16, 256.
https://doi.org/10.1186/s13063-015-0767-1
7. Sussman, B. J., & Fitch, T. S. (1958, August 2). Thrombolysis with fibrinolysin in cerebral arterial occlusion. Journal of the American Medical Association, 167(14), 1705–1709.
https://doi.org/10.1001/jama.1958.02990310011002
8. Marshall, R. S. (2015, August). Progress in intravenous thrombolytic therapy for acute stroke. JAMA Neurology, 72(8), 928–934.
https://doi.org/10.1001/jamaneurol.2015.0835
9. Grotta, J. C. (2023, April 1). Intravenous thrombolysis for acute ischemic stroke. Continuum (Minneapolis, Minn.), 29(2), 425–442.
https://doi.org/10.1212/CON.0000000000001207
10. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995). Tissue plasminogen activator for acute ischemic stroke. The New England journal of medicine, 333(24), 1581–1587.
https://doi.org/10.1056/NEJM199512143332401
11. U.S. Food and Drug Administration, Center for Drug Evaluation and Research. (1996, Mar 29). Alteplase approval letter. Retrieved from https://www.accessdata.fda.gov/drugsatfda_ docs/nda/96/altegen061896s.pdf
12. Hacke, W., Kaste, M., Bluhmki, E., Brozman, M., Dávalos, A., Guidetti, D., . . . Toni, D., & the ECASS Investigators. (2008, September 25). Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. The New England Journal of Medicine, 359(13), 1317–1329.
https://doi.org/10.1056/NEJMoa0804656
13. Adams, H. P., Jr., Brott, T. G., Furlan, A. J., Gomez, C. R., Grotta, J., Helgason, C. M., . . . Thies, W. (1996, September 1). Guidelines for thrombolytic therapy for acute stroke: A supplement to the guidelines for the management of patients with acute ischemic stroke. A statement for healthcare professionals from a Special Writing Group of the Stroke Council, American Heart Association. Circulation, 94(5), 1167–1174.
https://doi.org/10.1161/01.CIR.94.5.1167
14. Warach, S. J., Ranta, A., Kim, J., Song, S. S., Wallace, A., Beharry, J., . . . Wu, T. Y. (2023, July 1). Symptomatic intracranial hemorrhage with tenecteplase vs alteplase in patients with acute ischemic stroke: The comparative effectiveness of routine tenecteplase vs alteplase in acute ischemic stroke (CERTAIN) collaboration. JAMA Neurology, 80(7), 732–738.
https://doi.org/10.1001/jamaneurol.2023.1449
15. Thomalla, G., Simonsen, C. Z., Boutitie, F., Andersen, G., Berthezene, Y., Cheng, B., . . . Gerloff, C., & the WAKE-UP Investigators. (2018, August 16). MRI-guided thrombolysis for stroke with unknown time of onset. The New England Journal of Medicine, 379(7), 611–622.
https://doi.org/10.1056/NEJMoa1804355
16. Ma, H., Campbell, B. C. V., Parsons, M. W., Churilov, L., Levi, C. R., Hsu, C., . . . Donnan, G. A., & the EXTEND Investigators. (2019, May 9). Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. The New England Journal of Medicine, 380(19), 1795–1803.
https://doi.org/10.1056/NEJMoa1813046
17. Messé, S. R., Khatri, P., Reeves, M. J., Smith, E. E., Saver, J. L., Bhatt, D. L., . . . Schwamm, L. H. (2016, October 11). Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology, 87(15), 1565–1574.
https://doi.org/10.1212/WNL.0000000000003198
18. Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., . . . Tirschwell, D. L., & the American Heart Association Stroke Council. (2018, March). 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 49(3), e46–e110.
https://doi.org/10.1161/STR.0000000000000158
19. Khatri, P., Kleindorfer, D. O., Devlin, T., Sawyer, R. N., Jr., Starr, M., Mejilla, J., . . . Yeatts, S. D., & the PRISMS Investigators. (2018, July 10). Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: The PRISMS randomized clinical trial. JAMA, 320(2), 156–166.
https://doi.org/10.1001/jama.2018.8496
20. Chen, H. S., Cui, Y., Zhou, Z.-H., Zhang, H., Wang, L.-X., Wang, W.-Z., . . . Nguyen, T. N., & the ARAMIS Investigators. (2023, June 27). Dual antiplatelet therapy vs alteplase for patients with minor nondisabling acute ischemic stroke: The ARAMIS randomized clinical trial. JAMA, 329(24), 2135–2144.
https://doi.org/10.1001/jama.2023.7827
21. Burgos, A. M., & Saver, J. L. (2019, August). Evidence that tenecteplase is noninferior to alteplase for acute ischemic stroke: Meta-analysis of 5 randomized trials. Stroke, 50(8), 2156–2162.
https://doi.org/10.1161/STROKEAHA.119.025080
22. Menon, B. K., Buck, B. H., Singh, N., Deschaintre, Y., Almekhlafi, M. A., Coutts, S. B., . . . Swartz, R. H., & the AcT Trial Investigators. (2022, July 16). Intravenous tenecteplase compared with alteplase for acute ischaemic stroke in Canada (AcT): A pragmatic, multicentre, open-label, registrylinked, randomised, controlled, non-inferiority trial. Lancet, 400(10347), 161–169.
https://doi.org/10.1016/S0140-6736(22)01054-6
25
23. Kvistad, C. E., Næss, H., Helleberg, B. H., Idicula, T., Hagberg, G., Nordby, L. M., . . . Thomassen, L. (2022, June). Tenecteplase versus alteplase for the management of acute ischaemic stroke in Norway (NOR-TEST 2, part A): A phase 3, randomised, open-label, blinded endpoint, non-inferiority trial. Lancet Neurol, 21(6), 511–519.
https://doi.org/10.1016/S1474-4422(22)00124-7
24. Campbell, B. C. V., Mitchell, P. J., Churilov, L., Yassi, N., Kleinig, T. J., Dowling, R. J., . . . Davis, S. M., & the EXTENDIA TNK Investigators. (2018, April 26). Tenecteplase versus alteplase before thrombectomy for ischemic stroke. The New England Journal of Medicine, 378(17), 1573–1582.
https://doi.org/10.1056/NEJMoa1716405
25. International Stroke Trial Collaborative Group. (1997, May 31). The International Stroke Trial (IST): A randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. Lancet, 349(9065), 1569–1581.
https://doi.org/10.1016/S0140-6736(97)04011-7
26. CAST (Chinese Acute Stroke Trial) Collaborative Group. (1997, June 7). CAST: Randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. Lancet, 349(9066), 1641–1649.
https://doi.org/10.1016/S0140-6736(97)04010-5
27. CAPRIE Steering Committee. (1996, November 16). A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet, 348(9038), 1329–1339.
https://doi.org/10.1016/S0140-6736(96)09457-3
28. Wang, Y., Wang, Y., Zhao, X., Liu, L., Wang, D., Wang, C., . . . Johnston, S. C., & the CHANCE Investigators. (2013, July 4). Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. The New England Journal of Medicine, 369(1), 11–19.
https://doi.org/10.1056/NEJMoa1215340
29. Johnston, S. C., Easton, J. D., Farrant, M., Barsan, W., Conwit, R. A., Elm, J. J., . . . Palesch, Y. Y., & the Clinical Research Collaboration, Neurological Emergencies Treatment Trials Network, and the POINT Investigators. (2018, July 19). Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. The New England Journal of Medicine, 379(3), 215–225. https://doi.org/10.1056/NEJMoa1800410
30. Pan, Y., Elm, J. J., Li, H., Easton, J. D., Wang, Y., Farrant, M., . . . Johnston, S. C. (2019, December 1). Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack: A pooled analysis of clopidogrel in high-risk patients with acute non-disabling cerebrovascular events (CHANCE) and platelet-oriented inhibition in new TIA and minor ischemic stroke (POINT) trials. JAMA Neurology, 76(12), 1466–1473.
https://doi.org/10.1001/jamaneurol.2019.2531
31. Adams, H. P., Jr., Bendixen, B. H., Kappelle, L. J., Biller, J., Love, B. B., Gordon, D. L., & Marsh, E. E., III. (1993, January). Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke, 24(1), 35–41.
https://doi.org/10.1161/01.STR.24.1.35
32. Fassbender, K., Walter, S., Liu, Y., Muehlhauser, F., Ragoschke, A., Kuehl, S., & Mielke, O. (2003, June). “Mobile stroke unit” for hyperacute stroke treatment. Stroke, 34(6), e44.
https://doi.org/10.1161/01.STR.0000075573.22885.3B
33. Turc, G., Hadziahmetovic, M., Walter, S., Churilov, L., Larsen, K., Grotta, J. C., . . . Audebert, H. J. (2022, March 1). Comparison of mobile stroke unit with usual care for acute ischemic stroke management: A systematic review and metaanalysis. JAMA Neurology, 79(3), 281–290.
https://doi.org/10.1001/jamaneurol.2021.5321
34. Oliveira Gonçalves, A. S., Rohmann, J. L., Piccininni, M., Kurth, T., Ebinger, M., Endres, M., . . . Audebert, H. J. (2023, May). Economic evaluation of a mobile stroke unit service in Germany. Annals of Neurology, 93(5), 942–951.
https://doi.org/10.1002/ana.26602
35. Chen, J., Lin, X., Cai, Y., Huang, R., Yang, S., & Zhang, G. (2022, March 9). A systematic review of mobile stroke unit among acute stroke patients: Time metrics, adverse events, functional result and cost-effectiveness. Frontiers in Neurology, 13, 803162.
https://doi.org/10.3389/fneur.2022.803162
36. Lund, U. H., Stoinska-Schneider, A., Larsen, K., Bache, K. G., & Robberstad, B. (2022, October). Cost-effectiveness of mobile stroke unit care in Norway. Stroke, 53(10), 3173–3181.
https://doi.org/10.1161/STROKEAHA.121.037491
37. Feigin, V. L., Stark, B. A., Johnson, C. O., Roth, G. A., Bisignano, C., Abady, G. G., . . . Murray, C. J. L., & the GBD 2019 Stroke Collaborators. (2021, October). Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol, 20(10), 795–820.
https://doi.org/10.1016/S1474-4422(21)00252-0
38. Meinel, T. R., Wilson, D., Gensicke, H., Scheitz, J. F., Ringleb, P., Goganau, I., . . . Seiffge, D. J., & the DOAC-IVT Writing Group for the International DOAC-IVT, TRISP, and CRCSK-NIH Collaboration. (2023, January 3). Intravenous thrombolysis in patients with ischemic stroke and recent ingestion of direct oral anticoagulants. JAMA Neurology, 80(3), 233–243; Advance online publication.
https://doi.org/10.1001/jamaneurol.2022.4782
39. Deeds, S. I., Barreto, A., Elm, J., Derdeyn, C.P., Berry, S., Khatri, P., … Adeoye, O. (2021). The multiarm optimization of stroke thrombolysis phase 3 acute stroke randomized clinical trial: Rationale and methods. International journal of stroke: official journal of the International Stroke Society, 16(7), 873–880.
https://doi.org/10.1177/1747493020978345
40. Buchan, A. M., & Pelz, D. M. (2022). Neuroprotection in acute ischemic stroke: A brief review. The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques, 49(6), 741–745.
https://doi.org/10.1017/cjn.2021.223
26 Delaware Journal of Public Health - August 2023
Smoke from Canadian wildfires ruins outdoor activities in Delaware
Smoke from wildfires in eastern Canada diminished Delaware’s air quality on June 8, 9, 29, and 30. On those dates, Delaware and other central and midAtlantic states experienced unhealthy air quality due to the smoke’s particulate matter.
When the first round of smoke finally cleared, the Delaware Department of Natural Resources and Environmental Control (DNREC) warned that it could return due to a change in weather patterns and wildfires still burning. Northerly winds pushed it here again, forcing people inside during air quality alerts
Inhaling smoke or fine particulate matter 2.5 can worsen underlying breathing diseases such as asthma, emphysema, bronchitis, and chronic obstructive pulmonary disease (COPD) and cause heart failure, heart attack, and stroke, according to the Division of Public Health (DPH).
DPH and DNREC advise the public to avoid the smoke by staying indoors in a cool and clean environment, and for individuals working outdoors to wear properly fitted N95 or KN95 masks (not cloth or surgical masks). The Centers for Disease Control and Prevention suggest closing off a room from outside air and setting up a portable air cleaner or a filter to keep that air clean.










Sign up to receive Delaware air quality alerts at de.gov/aqi. Access real-time U.S. AQI data and interactive maps at the Environmental Protection Agency’s website, www.airnow.gov
Wildfires can happen anywhere
While wildfires in Canada and western U.S. states dominate headlines, Delaware forests, grasslands, and marshes can catch fire. Build your resiliency to fire by taking these steps from the Federal Emergency Management Agency (FEMA):


• Receive alerts of hazards several ways. Download the Federal Emergency Management Agency (FEMA) app to receive 24/7 alerts.
• Make an emergency plan. Visit Ready.gov.
• Review your property insurance policies and coverage for all possible hazards Purchase flood insurance, which is not typically covered by homeowner’s insurance, from the National Flood Insurance Program
• Make sure your personal identification documents are up to date. Download the Emergency Financial First Aid Kit to gather your personal, financial, and medical documents in one place. Use the Safeguard Critical Documents and Valuables checklist.
• Use fire resistant materials to build your home, renovate, or make repairs.
• Create a fire-resistant zone of at least 30 feet around your home that is free of flammable materials such as leaves and debris Learn how to reduce your risk by preparing your home and landscaping; visit www.cdc.gov/disasters/wildfires
• Begin saving for emergencies. Keep a small amount of small bills at home in a safe place in case you need to purchase emergency supplies, fuel, or food. ATMs and credit cards may not work during a disaster.
27
Public Health July 202
From the Delaware Division of
Keep recreational vehicle trailer chains off of the ground to prevent spar k s that can cause accidental wildfires .
Getty images
https://www.usfa.fema.gov/wui/outreach/
Officials: Talk openly with children about drugs and alcohol dangers to prevent them experimenting with it
The U.S. median monthly overdose deaths among individuals ages 10 to 19 years old increased 109% from 2019 to 2021, according to the Centers for Disease Prevention and Control.
Parents are advised to make homes as safe as possible by securing medication, safely disposing of medications, and consider obtaining Narcan and training on when and how to use it if there are opioids or opioid users in the child’s life.
Several tools are available to parents and guardians to educate themselves and talk openly with their children about drugs and alcohol. Parents, caregivers, and educators can use the Talk2KidsAboutDrugs toolkit when talking to teens about substance use and addiction risks. The toolkit offers fact sheets, educational materials, and more at www.helpisherede.com/talk-2-kids-about-drugs

#MyReasonWhyDE is a social media platform where teens share their reason to remain drug free.
If you or a loved one is struggling with addiction in Delaware, call the Department of Health and Social Services’ 24/7 Crisis Hotline to be connected to treatment and recovery options.
• In New Castle County, call 1-800-652-2929.
• In Kent and Sussex counties, call 1-800-345-6785. For free 24/7 counseling, coaching, and support, as well as links to mental health, addiction, and crisis services, call the Delaware Hope Line at 1-833-9-HOPEDE or 1-833-946-7333
For treatment and recovery services in Delaware or nearby states, visit HelpIsHereDE.com.
DPH publishes 2023 diabetes report
Prevention, early diagnosis, and management of diabetes can prevent and reduce poor outcomes including heart disease, stroke, kidney disease, lower limb amputations, blindness, and death. Individuals with diabetes can manage their condition through healthy lifestyle behaviors and medication adherence to control blood glucose levels.
While the five-year age-adjusted mortality rate for diabetes continues to decline in Delaware, there are concerning disparities by race. According to The Impact of Diabetes in Delaware, 2023 report, the five-year age-adjusted mortality rate for diabetes among non-Hispanic Blacks (34.5 deaths per 100,000 population) is twice that of non-Hispanic Whites (17.2 deaths per 100,000 population).
The report, prepared for the Delaware General Assembly, is published by the Delaware Department of Health and Social Services, Division of Public Health and Division of Medicaid & Medical Assistance; and the Delaware Department of Human Resources, Statewide Benefits Office Click here to read the agencies’ seven recommendations.

According to DPH’s Diabetes and Heart Disease Prevention and Control Program, 24.6% of Delaware adults have either diabetes or prediabetes.
Prediabetes and diabetes cost Delaware $1.1 billion annually – $818 million in direct medical expenses and $293 million in indirect costs. On average, medical expenditures for a person with diabetes are 2.3 times higher than for a person without diabetes.
In Fiscal Year 2022, diabetes was the costliest clinical condition by episodes of care among the State’s 13,123 Group Health Insurance Plan members with diabetes. The FY22 total allowed amount for diabetes was $85.3 million, a nearly $9 million increase over FY21.
In FY22, Delaware Medicaid Managed Care Organizations directly reimbursed providers $49 million for diabetes-related care. Fee-for-service claims for diabetesrelated care among Delaware Medicaid clients totaled an additional $2.6 million.
28 Delaware Journal of Public Health - August 2023 The DPH Bulletin – July 2023 Page 2 of 3
Getty images
Walk or pedal multiple trails to explore the state
Delaware offers numerous trails for pedestrians, cyclists, dog walkers, and families to stay active outdoors.
The Delaware Department of Transportation (DelDOT) provided this summary of projects to expand the state’s bicycle network:
• DelDOT recently completed the two-way cycle track in Newark which allows cyclists to travel safely in both directions on Delaware Avenue in a separated bike lane.
• When the Capital City Trail loop is completed in Kent County, it will be an approximately 15-mile loop around Camden and Dover. The section from South State Street to Lordship Lane near Camden was recently completed. The remaining connection will be completed as part of the East Camden Bypass project.

• The section of Dover’s Senator Bikeway between Mifflin Road and Dover High School is anticipated to begin construction in September
• The popular Georgetown to Lewes Trail follows the rail bed of the former Delaware Coast Line Railroad. When complete, the trail will connect Georgetown, Lewes, and Cape Henlopen State Park, as well as Rehoboth Beach by way of the 5.8-mile Junction & Breakwater Trail. Two stretches of the Georgetown to Lewes Trail are complete: seven miles between Gills Neck Road and Fisher Road in the Cool Spring area; and a three-quarter mile leg between the Georgetown Little League Park and Airport Road in Georgetown. The segment between Fisher Road and State Road in Georgetown is in the design phase. DelDOT received a federal RAISE grant to construct the remaining six miles of the trail. For more information about biking in Delaware, visit deldot.gov/programs/bike/biking_in_delaware and the Delaware Greenways' Interactive Map to Trails: https://delawaregreenways.org/trail-library/
Meet the U.S. physical activity recommendations to improve health

The Physical Activity Guidelines for Americans, 2nd edition recommends regular physical activity for ages 3 and older to maintain health and decrease the risk for high blood pressure, high cholesterol, diabetes, cancer, overweight/obesity, arthritis, and depression. Key recommendations are:
• “Preschool-aged children (ages 3 through 5 years) should be physically active throughout the day to enhance growth and development. Adult caregivers of preschool-aged children should encourage active play that includes a variety of activity types.”
• “Children and adolescents ages 6 through 17 years should do 60 minutes (one hour) or more of moderate-to-vigorous physical activity daily and include aerobic, muscle-strengthening, and bonestrengthening activity.”
• “Adults should do at least 150 minutes (two hours and 30 minutes) to 300 minutes (five hours) a week of moderate-intensity, or 75 minutes (one hour and 15 minutes) to 150 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Adults should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on two or more days a week.”
Older adults who cannot do 150 minutes of moderate-intensity aerobic activity a week because of chronic conditions “should be as physically active as their abilities and conditions allow.” Every week, “older adults should do multicomponent physical activity that includes balance training as well as aerobic and musclestrengthening activities.” Being physically active may reduce falls, allowing older adults to continue to live independently in their own homes.
The guide includes specialized recommendations for those with osteoarthritis, type 2 diabetes, hypertension, adult cancer survivors, and those recovering from hip fractures, and who are pregnant.
29 The DPH Bulletin – July 2023 Page 3 of 3
Photo: Daniel Paschall
Getty images
Update on Neurointerventional Therapy for the Treatment of Acute Cerebral Ischemia
Sudhakar Satti, M.D.
Associate Chief, Neurointerventional Surgery, ChristianaCare
Thinesh Sivapatham, M.D.
Associate Director, Comprehensive Stroke Program, ChristianaCare
ABSTRACT
Mechanical thrombectomy (MT) is a minimally invasive, fluoroscopically guided procedure to remove clots from the arteries in the head and neck. The procedure can be performed very quickly and effectively, with low complication rates, as techniques and technology have advanced in recent years. MT is among the most efficacious procedures performed today, with a very low number needed to treat (NNT) to impact outcomes. Expanded indications for MT include patients with large core infarcts, extended time windows from stroke onset, more distal occlusions, and milder symptoms. Trials have shown a significant benefit of MT in terms of reduced disability in nearly every patient population studied.
PRE-TEST
1. Which of the following patients might be a candidate for mechanical thrombectomy?
a. 78 year-old man who lives in a nursing home and needs some assistance, presenting as a wake-up stroke (last known normal > 12 hours ago) with NIH Stroke Scale (NIHSS)1 15 including right gaze deviation, slurred speech, and left sided weakness. Head CT shows a large right middle cerebral artery (MCA) territory infarct involving more than half the MCA territory, and computed tomography angiography (CTA) shows large vessel occlusion (LVO) in proximal right middle cerebral artery (MCA, M1 segment).
b. 71 year-old woman who lives independently, last known normal six hours ago, presenting with moderate to severe aphasia but normal strength in all extremities, and low NIHSS < 6. Head CT negative, CTA shows a distal left MCA (M3 segment) occlusion.
c. 91 year-old woman who lives independently, last known normal time unknown, presenting with NIHSS 20 including left gaze deviation, aphasia, and right sided weakness. Head CT shows small left MCA territory infarct and CTA shows left intracranial internal carotid artery occlusion (LVO).
d. None of the above.
e. All of the above.
2. What treatment options are available for this patient?
81 year-old woman, last known normal 16 hours ago, presents to your hospital with right gaze deviation and left sided weakness, NIHSS 14. Head CT negative, CTA shows right MCA M1 occlusion (LVO).
MECHANICAL THROMBECTOMY
Mechanical thrombectomy (MT) is a minimally invasive procedure to remove clots from the arteries in the head and neck, performed through a small 2-3 mm incision (usually in the groin, wrist, or occasionally neck) that allows access to the arterial system. The procedure can be performed under local anesthesia, conscious sedation, or general anesthesia depending on the patient’s clinical status and co-morbidities. A series of catheters are advanced into the brain using live x-ray (fluoroscopy) and subsequent devices specially designed to remove clots are used. The procedure has a technical success rate approaching 90%, with complication rates comparable to the administration of IV thrombolytics.2 Limitations of the procedure include the need for highly trained physicians (neurointerventional surgeons), dedicated endovascular suites/ equipment, and well-coordinated systems of care to minimize time from symptom onset to time of clot removal.
MT for acute ischemic stroke in the setting of large vessel occlusion is among the most efficacious surgery/intervention performed today. The number needed to treat (NNT) for one patient to have reduced disability is as low as 2, with NNT as low as 2.8 for functional independence at 90 days.3 When compared to other common procedures such as percutaneous coronary intervention for STEMI (NNT 23 to save a life),4 the very low NNT for MT indicates incredible procedural efficacy with a major impact on functional outcomes.
Stroke survivors represent the number one cause of long-term disability in the United States. Mechanical thrombectomy results in a significant cost benefit to the health care system by improving functional outcomes in the most severe strokes, thereby reducing the number of patients requiring long term care. Clinical outcome in ischemic stroke patients is measured using the modified Rankin Scale (ranging from mRS 0 = no disability to mRS 6 = dead). The benchmark outcome endpoint in stroke research and clinical trials has been functional independence at 90 days (mRS 0-2). Fifty percent of patients who undergo MT for large vessel occlusion stroke will have significant early neurological recovery at 24 hours, and nearly 50% will have functional independence
30 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.007
at 90 days (mRS 0-2)2 including the ability to perform all their activities of daily living (self-care/driving), and may be able to return to work.
A major paradigm shift in patient selection is an understanding that most patients that undergo MT have improvement in their functional status when compared to medical management alone without higher rates of complications. The indications for mechanical thrombectomy continue to expand and these trends include:
1. Patients presenting in a more delayed fashion from symptom onset, including wake-up strokes (no time restrictions for MT using advanced imaging techniques such as perfusion imaging; important to remember that rapid/earlier treatment is always favorable)5,6;
2. Patients presenting with larger infarcts on initial CT imaging (large core infarction)7;

3. Patients with pre-existing disability (mRS > 3) or life expectancy less than six months (cancer/ hospice);
4. Patients with milder stroke with disabling symptoms (low presenting NIHSS; trials ongoing)6;
5. Patients with smaller or more distal clots (trials ongoing).6
Evolving techniques and technology are allowing shorter procedure times (often less than 30 minutes), more complete clot removal, and higher rates of single pass efficacy which result in safer, more cost-effective procedures with lower complication rates. Patient outcomes from MT are optimized at hospitals certified as Thrombectomy Capable Stroke Centers or Comprehensive Stroke Centers (the highest level of stroke center certification) by The Joint Commission or other accrediting bodies. Facilities certified as Acute Stroke Ready Hospitals or Primary Stroke Centers are capable of acute evaluation, imaging, and treatment of ischemic stroke patients, including administering IV thrombolytics (and some Primary Stroke Centers may be capable of performing MT).
A major barrier to patients receiving MT is delayed presentation to the specialized centers capable of performing the procedure. Several critical factors may affect the pathway of the patient to the endovascular suite:
1. Delayed recognition that the patient is having a stroke by the patient/family/witness;
2. Delays in activation of emergency medical system (EMS) and transport to the closest stroke center;
3. Delays in transferring patients from a hospital without capabilities to perform MT to one that can (referred to as door-in/door-out time).
Patients and health care providers in Delaware are fortunate to have a state-wide Stroke System with formalized cooperation between the Delaware Department of Public Health, all hospitals throughout the state, EMS services, rehabilitation centers, and other agencies. The state’s Stroke System works closely together to improve stroke care including access to MT for all patients throughout Delaware.
POST-TEST
1. Which of the following patients might be a candidate for mechanical thrombectomy?
e. All of the above.
Expanding indications for MT allow access to the procedure for a broader group of patients with acute ischemic stroke, including those with large core infarcts or baseline functional deficits as with patient A, patients with milder but disabling deficits or more distal occlusions as with patient B, and in more extended time windows including unknown onset times as in patients A and C. We have no age or time cut-off for MT but rather use clinical and imaging information to make decisions regarding the procedure.
2. What treatment options are available for this patient?
This patient is outside the standard time window for IV thrombolytics. She is, however, a candidate for MT. She was transferred to our center and underwent successful MT (Figure 1). Her symptoms had nearly completely resolved upon discharge (NIHSS 1).
31
Figure 1. Before and After Images of a Successful Mechanical Thrombectomy
KEY POINTS
• MT is a minimally invasive, fluoroscopically guided procedure to remove clots from the arteries in the head and neck, which can be performed very quickly and effectively with low complication rates as techniques and technology have advanced in recent years.
• MT is among the most efficacious procedures performed today, with a very low NNT of 2.6 for one patient to have reduced disability.
• Indications for MT are expanding, including those patients with large core infarcts, extended time windows, more distal occlusions, and milder symptoms. Trials have shown a significant benefit in terms of reduced disability in nearly every patient population studied, with ongoing trials expected to broaden the indications even further.
Dr. Satti may be contacted at ssatti@christianacare.org
REFERENCES
1. National Institute of Neurological Disorders and Stroke. (2023, Jun). NIH Stroke Scale.
https://www.ninds.nih.gov/sites/default/files/documents/NIH_Stroke_ Scale_508C.pdf
2. Goyal, M., Menon, B. K., van Zwam, W. H., Dippel, D. W. J., Mitchell, P. J., Demchuk, A. M., . . . Jovin, T. G., & the HERMES collaborators. (2016, April 23). Endovascular thrombectomy after large-vessel ischaemic stroke: A metaanalysis of individual patient data from five randomised trials. Lancet, 387(10029), 1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
3 Martinez-Gutierrez, J. C., Leslie-Mazwi, T., Chandra, R. V., Ong, K. L., Nogueira, R. G., Goyal, M., Hirsch, J. A. (2019, December). Number needed to treat: A primer for neurointerventionalists. Interv Neuroradiol, 25(6), 613–618. https://doi.org/10.1177/1591019919858733
4. Chakrabarti, A. K., Gibson, C. M., & Pinto, D. S. (2012, November). Optimal selection of STEMI treatment strategies in the current era: Benefit of transferring STEMI patients for PCI compared with administration of onsite fibrinolytic therapy. Current Opinion in Cardiology, 27(6), 651–654 https://doi.org/10.1097/HCO.0b013e3283587c69
5 Snelling, B., Mccarthy, D. J., Chen, S., Sur, S., Elwardany, O., Sheinberg, D. L., Starke, R. M. (2019, Apr-Jun). Extended window for stroke thrombectomy. Journal of Neurosciences in Rural Practice, 10(2), 294–300.
https://doi.org/10.4103/jnrp.jnrp_365_18

6. Mokin, M., Ansari, S. A., McTaggart, R. A., Bulsara, K. R., Goyal, M., Chen, M., & Fraser, J. F., & the Society of NeuroInterventional Surgery. (2019, March). Indications for thrombectomy in acute ischemic stroke from emergent large vessel occlusion (ELVO): Report of the SNIS Standards and Guidelines Committee. Journal of Neurointerventional Surgery, 11(3), 215–220.
https://doi.org/10.1136/neurintsurg-2018-014640
7. Sarraj, A., Hassan, A. E., Abraham, M. G., Ortega-Gutierrez, S., Kasner, S. E., Hussain, M. S., . . . Albers, G. W., & the SELECT2 Investigators. (2023, April 6). Trial of endovascular thrombectomy for large ischemic strokes. The New England Journal of Medicine, 388(14), 1259–1271
https://doi.org/10.1056/NEJMoa2214403
32 Delaware Journal of Public Health - August 2023
STROKE SUMMIT
Heart disease is the number one cause of death in the U.S., claiming more lives than all forms of cancer combined. Stroke is the number five cause of death in the U.S., and the number three cause of death here in Delaware.
The American Heart Association/American Stroke Association statewide Stroke Summit will feature a series of presentations to educate and inform local residents and healthcare professionals on the risk factors of stroke, the warning signs of stroke, the latest in prevention, research initiatives under way and so much more. Healthcare professionals will earn continuing education credits.
Chair of the Event:
DECEMBER 2, 2023
9:00 AM – 1:00 PM
HYATT PLACE
DEWEY BEACH
1301 COASTAL HWY
DEWEY BEACH, DE
David Tam, MD

President & CEO – Beebe Healthcare

Host of the Event:
E. Thomas Harvey, III

Chairman & CEO – Harvey, Hanna & Associates
AHA Delaware Board of Directors Chair
Presenting Sponsor:

33
Delaware
SAVE THE DATE
Nursing Care of Delaware’s Stroke Patients
Reina W. McAndrew M.S., A.P.R.N., F.N.P.-B.C., S.C.R.N. and Mary Ciechanowski M.S.N., A.P.R.N., A.C.N.S.-B.C., C.C.R.N.-K. Stroke Program Coordinators, Comprehensive, Primary and Acute Stroke Ready Centers, ChristianaCare
ABSTRACT
This article will highlight essential nursing care in each aspect of the continuum of stroke care. Nursing interventions will be covered from primary stroke prevention through the transitions needed for healthy return to the community and secondary stroke prevention.
INTRODUCTION
With nearly 800,000 strokes occurring annually in the United States,1 every nurse—regardless of their role—has the potential to experience caring for a stroke patient somewhere along the patient’s stroke journey. The American Heart Association (AHA) describes stroke as “a devastating disease with significant personal, family and health system impacts.”2 Stroke is a leading cause of long-term disability in the US. Between 2018 and 2019 the United States’ stroke-related costs were more than $56 billion dollars.1 Nurses play a pivotal role in the care of acute stroke patients and prevention of future stroke.
This article will highlight essential nursing care in each aspect of the continuum of stroke care. Nursing interventions will be covered from primary stroke prevention through the transitions needed for healthy return to the community and secondary stroke prevention. In addition, nursing advocacy opportunities for the “right care, at the right time, in the right setting” will be highlighted.3 Nurses are integral to effective education and communication within each aspect of stroke care. To ensure safe transitions, it is important to understand each aspect of the stroke care continuum.
PREVENTION
Stroke prevention is an essential component of nursing stroke care. Modifiable stroke risk factors include hypertension, diabetes, smoking, hyperlipidemia, cardiovascular disease, atrial fibrillation, hypercoagulopathy, carotid stenosis, oral contraceptive use, obesity, and drug and alcohol abuse. Nonmodifiable stroke risk factors include age 55 or older, family history of stroke, previous stroke, or transient ischemic attack (TIA), and sickle cell disease.4
Individuals in the State of Delaware have higher rates of hyperlipidemia, drug/alcohol use, and smoking than the national average. Nurses can work to educate their patients on how to reduce their risk of stroke through understanding the various ways of reducing cholesterol; as well as reducing or eliminating drug, tobacco, and alcohol use. These risk factors could be addressed at every patient contact in Delaware.
According to the Centers for Disease Control and Prevention (CDC) stroke facts website, only 38% of people knew to call 911 when they recognized the major symptoms of stroke.1 There is less disability leading to more independence three months after a stroke in patients who arrive at the emergency department (ED) within three hours of symptom onset than those who access care later. Delaware nurses could prevent significant disability from stroke via community education on stroke recognition, and by
instruction to activate the emergency medical system (EMS) at the first sign or symptom of a stroke.1
Advocacy
The American Heart Association (AHA) suggests that stroke systems of care should work to ensure stroke patients receive appropriate treatment as fast as possible. Nurses can participate in Delaware’s Stroke System of Care Stroke Committee’s public virtual meetings to ensure patients get to the right location for the right treatment at the right time. Information regarding these meetings can be found https://publicmeetings.delaware.gov/#/ meeting/75647
RECOGNITION
Early recognition of stroke is critical, as treatments for acute ischemic and hemorrhagic strokes are time dependent. For ischemic strokes, restoration of blood flow and oxygen to brain tissue at-risk for permanent damage can be achieved via intravenous thrombolytic medications or mechanical thrombectomy. The damage to the area of at-risk tissue (the penumbra) can be minimized with acute treatments. Early detection is essential to make treatment with intravenous thrombolytics or mechanical thrombectomy possible.
Nurses working triage in EDs receive regular education on stroke recognition. But any nurse in any location could potentially find themselves witnessing the onset of stroke. Sometimes it is recognized when a patient in the specialist’s office cannot get their words out; other times it is recognized when a patient comes into or calls their primary care provider’s (PCP’s) office with double vision. Stroke could even be recognized when a patient has a drooping face coming out of anesthesia after a procedure.
Being familiar with signs and symptoms of stroke will help you recognize stroke and respond appropriately. BE-FAST is an acronym for stroke recognition indicating Balance, Eyes, Face, Arm, Speech, and Time. Is the patient’s balance off? Watch for sudden loss of balance. Any change in vision? Sudden blurred or double vision or loss of vision in one or both eyes? Is one side of their face drooping? Ask the person to smile. Is an arm weak? Ask them to raise both arms. Is their speech impaired? Ask them to repeat a simple phrase.
In addition to these signs and symptoms, hemorrhagic strokes can present with the worst headache of the patient’s life, nausea and vomiting, photophobia (light sensitivity), and nuchal rigidity (neck stiffness). When any of these symptoms are recognized, it is time to call 911 or activate your hospital’s in-house stroke response system.
34 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.008
Advocacy
Nurses can participate in community education for recognition of stroke as a 911-worthy emergency. Sharing stroke education across social media pages is a simple action with potentially broad benefits. Shareable links can be found on the Delaware Division of Public Health’s Facebook, Twitter, and Instagram pages.
ACCESSING EMERGENCY CARE
To obtain lifesaving stroke treatment, people should call 911 to have an ambulance transport them to a hospital ED. Instructions to call 911 to get to a hospital are crucial to decrease symptom onset to treatment time because this can significantly improve patient outcomes. For this reason, nurses should advise community members not to drive someone having a stroke to the hospital, nor should they go to a medical aid unit, or make a doctor’s appointment. All these actions can contribute to significant delays leading to ineligibility for urgent treatment. For hospitalized patients who display signs and symptoms of stroke, one Delaware hospital has developed the acronym “STROKE” to guide bedside nurses to ready patients for evaluation for emergent stroke treatment eligibility.
• Symptoms – what stroke symptoms are noted?
• Timing – what is the time the patient was last seen as “normal”?
• Ready for CT scan– is the patient ready to move (i.e. sling is under the patient, there is a clear path in the room, an oxygen tank is prepped and ready)?
• Obtain – have the patient’s vital signs and blood sugar been taken? Is 20 G IV prepped?
• Know your patient – what is the patient’s code status, past medical history, reason for visit, recent pain/ sedating medication?
• Eat – Keep patient NPO until the CT scan is complete and after a stroke swallow screen can be completed
EMERGENT CARE
Nurses provide emergent stroke care in multiple venues such as the ED, interventional radiology suite, and intensive care units. Through standardized stroke evaluation processes, nurses can improve treatment decisions and care delivery times, thereby improving outcomes for stroke patients.
When someone arrives at a hospital ED with new stroke signs and symptoms, the first questions asked are “when did the symptoms start? When was the patient last seen as normal?” This information is imperative to guide what happens next. The healthcare team needs to make decisions on whether this potential stroke patient is eligible for either of the two main emergent stroke treatments available.
The first treatment option is an intravenous medication known as a thrombolytic which works to dissolve a clot blocking blood flow. The maximum time window to receive thrombolytic treatment is 4.5 hours since the patient was last seen as normal. The second treatment is a specialized procedure known as a thrombectomy, where the clot is removed. The maximum time window to be eligible for the thrombectomy procedure is 24 hours from last seen normal in most cases. Because the time window is not the only criteria for urgent treatment, the healthcare team must have expertise in identifying eligible patients.4
Once a patient meets certain criteria, the stroke evaluation process starts with nurses and physicians collaborating with other team members to quickly obtain critical information needed for decision making regarding emergent treatment. This rapid process includes obtaining information on patient history, home medication list, blood tests and—most importantly—a CT scan of the brain. Since “time is brain,” the quicker the eligible patient receives stroke treatment, the more brain cells are saved.
Hospitals use data metrics to monitor outcomes and determine how quickly treatment is provided. Nurses play a vital role in these data metrics, especially door-to-needle (time of ED arrival to time of thrombolytic delivery) and door-to-puncture (time of ED arrival to initial thrombectomy skin puncture).
The ED nurse has many responsibilities during the stroke evaluation process, including identifying potential stroke patients at the triage desk, multiple clinical assessments, transporting the patient safely and quickly to CT scanner and the thrombectomy lab, obtaining blood for lab tests, and administering all medications including the thrombolytic to those who are eligible. In addition, the ED nurse collaborates with the physician and other team members on critical information such as vital signs, blood pressures, neurological assessments, as well as keeping the family informed. Nurses are also key to the in-hospital stroke evaluation process for admitted patients who show signs of an acute stroke.
Once the stroke evaluation process has been completed in the ED, the patient will be admitted to the hospital. The ED nurse provides a comprehensive report with important clinical information to the admission unit nurse team to ensure a seamless transition, as well as a positive outcome.
ACUTE CARE (HOSPITAL STAY)
Hospital care is essential in cases of acute stroke, and stroke trained nurses have a prominent role in contributing to patient outcomes during acute hospitalization. Nurses at all levels have a hand in the creation of interdisciplinary, internal, evidence-based policies, and protocols, as well as putting those stroke protocols into practice at the bedside.
Best practices or standards of care include a stroke swallow screen assessment before any oral intake, neurologic assessments as ordered, and blood pressure and glucose control as ordered. Other important assessments nurses should monitor are deep vein thrombosis risk, fall risk, hydration, nutrition, mobilization, and pressure ulcer risk. Nurses trained in these interventions are extremely important for identifying and preventing post-stroke complications.
Once admitted to the hospital, stroke patients’ lives are dependent on expert nurses monitoring for and identifying signs and symptoms of dangerous post-stroke complications including hemorrhagic transformation, brain swelling, brain herniation, seizure, pneumonia, bowel and bladder problems, depression, and falls. Some of the early signs and symptoms of these complications are headaches, nausea and vomiting, confusion, decreased level of arousal, restlessness, speech changes, visual changes, and motor weakness. Late signs and symptoms include pupillary changes, hemiplegia, unresponsiveness, abnormal posturing, and changes in respiratory patterns.
35
Stroke Centers
Thrombolytic therapy is the standard of care for acute ischemic stroke, and any ED can provide this treatment. The Joint Commission (TJC) has several levels of stroke center certification for acute care facilities. All adult acute care hospitals in Delaware, except for the Veteran’s Administration, have been certified by TJC as Stroke Centers. Certified stroke centers balance the required medical care necessary to achieve good outcomes with discharging the patient as quickly and safely as possible. There are currently six Primary Stroke Centers, one Comprehensive Stroke Center and one Acute Stroke Ready Hospital designation in the State of Delaware.
Primary Stroke Centers and Acute Stroke Ready Centers administer thrombolytics, while Comprehensive Stroke Centers administer thrombolytics and also perform thrombectomies and engage in complex hemorrhagic stroke care. All Delaware hospitals have protocols in place to transfer patients to the appropriate stroke center depending on specific patient criteria. With each designation, there are stringent eligibility criteria, as well as strict standards and core measures each hospital is required to meet. Nurses have a great deal of responsibility in achieving a majority of these stroke core measures, all of which contribute to better patient outcomes. Some of the core measures and standards specific to patients during hospital admission include:
• An NIH Stroke Scale (a stroke severity scale) is completed within 12 hours of arrival for patients who do not undergo emergent stroke therapy. For those undergoing acute therapies, NIHSS is obtained prior to treatment.
• Prophylaxis against venous thromboembolism is acquired by end of hospital day two for both ischemic and hemorrhagic stroke patients.
• Ischemic stroke patients are administered antithrombotic therapy by the end of hospital day two.
• Ischemic or hemorrhagic stroke patients are assessed for rehabilitation service needs.
• Patient and family stroke education: ischemic or hemorrhagic stroke patients or their caregivers are provided written educational materials during the hospital stay addressing the activation of EMS, the need for follow-up after discharge, medications prescribed at discharge, personal risk factors for stroke, and warning signs and symptoms of stroke.
• Ischemic stroke patients are prescribed antithrombotic therapy at hospital discharge.
• Ischemic stroke patients with atrial fibrillation/flutter are prescribed anticoagulation therapy at hospital discharge.
• Ischemic stroke patients are prescribed statin medication at hospital discharge.
There are also additional Comprehensive Stroke Center measures that focus on complex stroke patients such as those who receive thrombolytic and thrombectomy urgent treatments, as well as hemorrhagic stroke patients.
Advocacy
Nurses can advocate for designated stroke units, as the benefits conveyed from these units are well documented.
POST-ACUTE CARE
Patients and their families often seek the opinions of acute care nurses regarding which post-acute care setting would be best for them. Therefore, understanding the post-acute care delivery system is a vital component of the acute care nurse’s knowledge base.
The post-acute stroke care spectrum includes Inpatient Rehabilitation Facilities (IRF), Skilled Nursing Facilities (SNF), discharge to home with home health therapies, and discharge to home self-care. On average, a little more than 52% of stroke patients are discharged to facilities, with approximately 24% going to IRFs and 27% going to SNFs.3
IRFs require stroke patients to participate in 15 hours of skilled therapy per week. They are staffed by registered nurses 24 hours a day, many of whom are certified in rehabilitation nursing specialty practice. IRFs also require that stroke patients are likely to be discharged to the community.
SNFs do not have specific skilled therapy requirements and do not require 24-hour registered nurse staffing. Both types of inpatient facilities work on improvement in mobility, self-care, and cognition which can lead to lower hospital readmission rates. The AHA/American Stroke Association recommends care at the IRF level.3
For more information, nurses can access the association of rehabilitation nurses’ detailed descriptions of post-acute care settings: https://rehabnurse.org/uploads/membership/ARN_Care_ Transitions-Levels_of_Care.pdf. Additional information can also be found at The Centers for Medicare and Medicaid website, where facilities can be compared to assist patients and families in their decision: https://www.medicare.gov/care-compare/
TRANSITION TO HOME
Transitioning from an inpatient setting to home is typically when family caregivers must assume the caregiving role. This transition is a particularly vulnerable time in the stroke patient’s care continuum. Therefore, the caregiver should be assessed for the skills, capacity, and resources to provide care their loved one’s needs. Recent research showed that caregiver assessment tools could be used to create tailored care plans and interventions resulting in improved health and decreased strain of the patient’s home caregiver.3
Measures of successful home discharge and stroke recovery have not been clearly defined, but avoiding complications that can lead to hospital readmission is a goal shared by patients, families, and inpatient facilities alike. Hindrances to home discharge safety include patient comorbidities, cognitive deficits, medication regimens, as well as fatigue. Difficulty with access to and management of clinic and therapy appointments also contributes to home discharge complications.
There are several nursing interventions that may prevent hospital readmission: post-discharge phone calls, medication reconciliation, clinic or home visits, education on the signs and symptoms of stroke, and helping patients access primary care
36 Delaware Journal of Public Health - August 2023
that contributed to the stroke and, vitally, reduce risk of stroke recurrence. Some of these medications, like brand name anticoagulants, can be quite expensive. Ensuring financial coverage, which may include managing prior authorizations, is essential.
Community Resources
Whereas care coordination is a more structured process, usually involving coordination with health care providers and with the patient’s insurance, social workers also connect patients and their families with support groups, educational resources, and social assistance programs to promote a successful transition back to their community. The Delaware Stroke Initiative has employed both in person and remote support groups.7 To help address needs like housing, food, transportation, and other such essential requirements, Delaware’s 2-1-1 is a free confidential service that connects people in the State of Delaware with health and human services to support individuals and families in need.8
Social Determinants of Health
As the guide for national health promotion and disease prevention under the U.S. Department of Health and Social Services, Healthy People 2030 promotes a society in which all people can achieve their full potential for health and well-being across the lifespan.9 A powerful tool in building this vision is identifying and addressing the Social Determinants of Health, conditions where people are born, live, learn, work, play, and age that affect a wide range of health, functioning, and quality of life outcomes and risks.10 Inherent in the role and function of a social worker, as charged by the principles of service and social justice in the National Association of Social Worker’s Code of Ethics, the social worker – as member of a stroke survivor’s care team – must identify the impact of non-medical issues on a stroke patient’s progression of care. Factors like housing, transportation, access to nutritious foods and exercise, as well as a plethora of non-medical factors may contribute to causing a primary or recurrent stroke. While an intimidating task seemingly beyond the abilities of one medical social worker in a healthcare setting, Healthy People 2030 has a strong emphasis on data driven research and collaborative partnerships. Both acute care and the outpatient setting have medical codes specific to social determinants of health. As part of the care team, social workers should be purposeful not only in addressing patient specific issues to the best of their professional abilities, but also in ensuring accurate documentation of these determinants.
Vulnerable Populations
In healthcare, the designation of vulnerable population is simultaneously broad and specific. Broadly, it refers to individuals who have poor access to healthcare and experience poor outcomes as the result of factors such as age, geographic location, language, gender or sexual orientation, chronic illness or disability, race, and economic status. Sometimes, depending on a host of interplaying factors, specific populations are more vulnerable than others, such as persons in congregate care settings during the COVID pandemic.
Due to the elevated risk of disability and mortality, particularly among individuals with a history of stroke, social workers have a crucial responsibility to diligently identify individuals at risk of not receiving preventive care. One of the most vulnerable populations is the uninsured. Assessment and stabilization of all persons in an emergency medical situation, regardless
of insurance coverage or ability to pay, is safeguarded by the federal Emergency Medical Treatment & Labor Act (EMTALA). For many stroke patients, stabilization is just the beginning. An uninsured person may not have access to much needed post hospital care, like medications and rehabilitative services. A well-informed social worker should readily be aware of healthcare clinics and financial assistance programs, and facilitate completion of applications and making referrals.
Another vulnerable population is the socially isolated. As recently articulated by the U.S. Surgeon General, loneliness is associated with a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death.11 The AHA provides a sharper focus of the impact of loneliness on stroke, reporting that socially isolated adults with three or fewer social contacts per month may have a 40% increased risk of recurrent stroke or heart attack.12 Discharge planning back to the community – particularly if the person is impacted by stroke deficits – can be challenging. Loneliness and social isolation can be well hidden, so a purposeful conversation is worthwhile. For a formal assessment, the Lubben Social Network Scale is a brief instrument that gauges social isolation in older adults by measuring perceived social support received by family and friends.13
Of note, technological literacy has become a recent stressor for patients in managing their health. Technologies supporting care coordination and patient engagement can serve as a bridge, rather than a barrier, only when barriers are directly remedied. Issues include lack of internet access, lack of a phone, lack of an appropriate device, cost concerns, lack of training for the individuals and their family members on how to use the tools, and language barrier issues.
Stroke care is not only best provided by a multidisciplinary team, but also across a continuum of care. Stroke care usually begins in the community with 911 and first responders and ideally ends in the community, as the stroke survivor transitions back to their home.
SOCIAL WORK DURING ACUTE HOSPITAL CARE OF A STROKE PATIENT
This phase of care, beginning with the arrival of the ambulance and proceeding through the Emergency Department and continued hospitalization, is the busiest, most stressful, and uncertain phase for a stroke patient and their loved ones. The medical team is focused on accurate diagnosis, treatment, and stabilization. During this stabilize and treat phase, the hospital social worker focuses on family engagement, coordinating family meetings with the medical team, and addressing needs and concerns as brought up by the patient and their families.
The discharge planning process happens concurrent to stabilize and treat. While “discharge planning starts at the door” is a standard for hospitals, it is an overwhelming thought for a patient and their family to even think about during such a crisis. The hospital social worker, sometimes with a nurse care management partner, is tasked with educating patients and their families on its necessity. Discharge plans for life changing conditions like stroke often take time as they have a multitude of variables.
From the hospital, the ASA strongly recommends the Inpatient Rehabilitation Facility (IRF) level of care for stroke survivors who can manage three hours of therapy daily.14 Other options for care
39
include skilled nursing facilities (SNFs), appropriate for those whose nursing needs are more significant than rehabilitation needs and patients can only tolerate an hour daily of therapies. Long term acute care (LTAC) is specifically for stroke survivors with serious medical conditions that require ongoing care but no longer require intensive care or extensive diagnostic procedures. For stroke survivors leaving acute care with minimal to no deficits, homecare is an option, which can provide skilled nursing, physical, occupational and speech therapies, and social work. Some stroke survivors can be managed safely with outpatient follow up. In these cases, it is imperative that the discharge planner, often a social worker, ensure follow up appointments as recommended by the care team, usually neurology, cardiology, and primary care. Of equal importance is ensuring the stroke survivor has access to prescribed medications.
SOCIAL WORK DURING POST-ACUTE FACILITY CARE OF A STROKE PATIENT
Stroke deficits can be pervasive, impacting a multitude of functions: gross motor skills, fine motor skills, speech and language, cognition, vision, and emotions. Appropriate, quality rehabilitation with specially trained therapists is necessary for the best possible recovery. Rehab therapies usually begin in the hospital setting once physicians have cleared the patient medically. It is vital that a stroke survivor with deficits transition to the next level of rehabilitative care as soon as possible. As hospital level of care is ideally brief and focused on medical stabilization, hospital therapy sessions are comparatively brief and focused on assessment of the stroke survivor’s deficits and subsequent discharge needs.
The ASA estimates that 10% of people fully recover from a stroke, 25% have only minor impairments and 40% have moderate impairments that are manageable with some special care. The sooner a stroke survivor starts a therapy program, the more likely they are to regain impacted abilities and skills.14
In the IRF level of care, therapists in collaboration with a physician specially trained in rehabilitative medicine provide comprehensive interventions. A stroke survivor’s IRF care team is focused on the prevention of secondary complications, treatment to reduce neurological deficits, and compensation to adapt to disabilities that may continue over an indefinite time. The IRF social worker’s role and function is similar to the acute hospital social worker, with heightened focus on return to the community and post-facility adjustment. The IRF care team relies heavily on social work to facilitate a safe discharge to home, the preferred discharge goal after extensive rehabilitation is completed.
Stroke survivors who step down from the hospital to a SNF usually have skilled nursing needs that take precedence over rehabilitation needs. Likely, they are unable to tolerate three hours of daily therapy, which is often related to previous level of functioning, extensiveness of the stroke, or the interplay of the stroke with comorbidities. Social workers in the SNF level of care carry a breadth of responsibilities. They facilitate the admission process, assist in creating a comprehensive plan of care, perform needs assessments, and plan for discharge. A SNF social worker will manage discharge plans to IRF, to the home, or transition a patient to long term care in a nursing home.
Stroke survivors who discharge from the hospital to the LTAC setting have serious medical conditions that require ongoing care, but no longer require intensive care or extensive diagnostic procedures. They may then transition to IRF, SNF or even home.
The focus of stroke care and medical care in general is to restore a person’s health and wellbeing. Some strokes are so profound that they cause irreparable damage. Hospice can be the right support for certain stroke patients. The hospital social worker can facilitate goals of care conversations and ensure referrals are made to the agency that can best care for a patient and their family at this most critical point. Hospice social workers then continue to offer support, whether it is counseling or resource finding.
DISCHARGE PLANNING FROM FACILITY LEVEL OF CARE
As levels of medical care that treat stroke, hospitals, IRFs, SNFs and LTACs have the common thread of being 24-hour care facilities with medical supervision and access to highly trained healthcare professionals. Discharge planning from each level of care, whether it is to another 24- hour care facility or to home, mandates effective needs assessments. Discharge planning tools guide the discharge planner and their team in well-informed decision making about the stroke survivor’s needs, and how to provide the most appropriate care possible.
There are several discharge planning models to guide social workers and their fellow clinicians, all with the shared goal of transitioning the patient out of facility care safely and effectively.
IDEAL (Include, Discuss, Educate, Assess, Listen) focuses on engaging patients and family members. RED (Re-Engineered Discharge) focuses on actions the hospital undertakes during and after the hospital stay to ensure a smooth and effective transition at discharge, making follow up appointments, identifying discharge medications and planning how patients can obtain them. The Agency for the Healthcare Research and Quality, under the U.S. Department of Health and Human Services, has toolkits for both initiatives.15,16 Better Outcomes for Older Adults through Safe Transitions (BOOST), emphasizes teach back and capturing discharge information on a readable one-page document.17 An integrated and pragmatic approach that is informed by research and evidence from sources like the above three approaches can help guide a comprehensive discharge plan individualized to the patient.
SOCIAL WORK DURING THE OUTPATIENT PHASE OF STROKE PATIENTS
At this point in the recovery process, social workers are focused on the stroke survivor’s adjustment back to their home and community, arguably the most important transition. Depending on the severity of the stroke, pervasiveness of any deficits, and impact of medical comorbidities, it could last weeks to months after a stroke survivor arrives home. For others, it can be a couple of days, as may be case with a TIA. In the initial three months after a stroke, the risk of stroke is 15 times higher than the general population. Furthermore, the ASA estimates that 23% of strokes are recurrent. Clearly, attention to this transition is crucial.
In the outpatient setting, the stroke survivor may access a social worker through a home care agency who is also providing skilled nursing and therapy services. Social work may also be available
40 Delaware Journal of Public Health - August 2023
if the primary care physician or other involved provider is part of an accountable care organization (ACO). An ACO care coordinator will reach out to a stroke survivor to ensure they are aware of the supports offered by the ACO team. Social work is also available if the patient is undergoing cancer treatment or getting hemodialysis.
Generally, the outpatient social worker will build on the successful discharge planning from previous levels of care. If there are issues with availability of prescribed medications, durable medical equipment, or expected healthcare services, a social worker is helpful in navigating these issues to resolution. Social workers will provide both education and counselling for the patient and their families to assist them in processing the realities of the stroke event and its aftermath. The social worker can also focus on social supports such as finding social self-help groups within the community. The outpatient social worker uses their own critical thinking, input from the medical care team, and feedback from the stroke survivor to identify and address, as best possible, barriers to the stroke survivor’s stability within their own community. Of perhaps even greater value is the work an outpatient social worker does that contributes to stroke prevention – access to medications, screenings, and medical transportation, to name a few.
CONCLUSION
Strokes are one of the most stressful, life changing things a person will ever experience. No one plans for them. Compassionate patient centered care goes a long way to alleviate that stress and get the patient on their road to recovery. Social workers can be helpful at all stages of patient stroke recovery and are a vital resource to the care team and to the patient. Ms. McDermott may be contacted at amcdermott@che-east.org
REFERENCES
1. National Association of Social Workers. (n.d.). About social workers. https://www.socialworkers.org/News/Facts/Social-Workers
2. American Stroke Association. (n.d.). Professionals. https://www.stroke.org/en/professionals
3. Delaware Stroke Resources. (n.d.). Stroke education. https://delawarestrokeresources.org/?page_id=398
4. Delaware Academy of Medicine/Delaware Public Health Association. (2022). 2022 Scholz stroke education conference. https://delamed.org/education/educational-series/conferences/2022scholz-stroke-education-conference/
5. Towfighi, A., Ovbiagele, B., El Husseini, N., Hackett, M. L., Jorge, R. E., Kissela, B. M., . . . Williams, L. S., & the American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research. (2017, February). Poststroke depression: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 48(2), e30–e43.
https://doi.org/10.1161/STR.0000000000000113
6 American Stroke Association. (2018, Nov). Pseudobulbar affect (PBA).
https://www.stroke.org/en/about-stroke/effects-of-stroke/emotionaleffects-of-stroke/pseudobulbar-affect
7 Delaware Stroke Resources. (n.d.). Delaware support groups. https://delawarestrokeresources.org/?page_id=337
8. 2-1-1 Delaware. (n.d.). Help starts here. https://delaware211.org/
9 United States Department of Health and Human Services (n.d.). Healthy people 2030: Building a healthier future for all. https://health.gov/healthypeople
10 United States Department of Health and Human Services (n.d.). Social determinants of health.
https://health.gov/healthypeople/priority-areas/social-determinants-health
11. Office of the U.S. Surgeon General. (2023). Our epidemic of loneliness and isolation: The U.S. Surgeon General’s Advisory on the healing effects of social connection and community.
https://www.hhs.gov/sites/default/files/surgeon-general-socialconnection-advisory.pdf
12 Cené, C. W., Beckie, T. M., Sims, M., Suglia, S. F., Aggarwal, B., Moise, N., McCullough, L. D., & the American Heart Association Social Determinants of Health Committee of the Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research; Prevention Science Committee of the Council on Epidemiology and Prevention and Council on Cardiovascular and Stroke Nursing; Council on Arteriosclerosis, Thrombosis and Vascular Biology; and Stroke Council. (2022, August 16). Effects of objective and perceived social isolation on cardiovascular and brain health: A scientific statement from the American Heart Association. Journal of the American Heart Association, 11(16), e026493. https://doi.org/10.1161/JAHA.122.026493
13. Brandeis University. (n.d.). Lubben social network scale. https://www.brandeis.edu/roybal/docs/LSNS_website_PDF.pdf
14. Winstein, C. J., Stein, J., Arena, R., Bates, B., Cherney, L. R., Cramer, S. C., . . . Zorowitz, R. D., & the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. (2016, June). Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 47(6), e98–e169. https://doi.org/10.1161/STR.0000000000000098
15. Agency for Healthcare Research and Quality. (2017, Dec). Care transitions from hospital to home: IDEAL discharge planning.
https://www.ahrq.gov/patient-safety/patients-families/engagingfamilies/ strategy4/index.html
16 Agency for Healthcare Research and Quality. (2023, Apr). Reengineered discharge (RED) toolkit.
https://www.ahrq.gov/patient-safety/settings/hospital/red/toolkit/index.html
17 Coffey, C., Greenwald, J., Budnitz, T., & Williams, M. V. (2013). Project BOOST implementation guide, 2nd Ed. Society of Hospital Medicine.
https://www.hospitalmedicine.org/globalassets/professionaldevelopment/professional-dev-pdf/boost-guide-second-edition.pdf
41
From the Delaware Division of Public Health August 202

Be up to date with immunizations
Delawareans can be protected from many diseases by staying up to date with their immunizations, beginning by visiting their health care provider. August is National Immunization Awareness Month, an observance that highlights the importance of routine vaccination for people of all ages
As parents and guardians prepare to send children back to school, the Division of Public Health (DPH) advises to get updated immunization records from the Delaware Immunization Program or the health care provider. When children’s routine vaccinations are current, they stay healthy, in school, and ready to learn. First-year college students living in residential housing and individuals with HIV and other conditions need to be up to date, especially with the Meningococcal vaccine.
Since Coronavirus 2019 (COVID-19) is still with us, it is important to get vaccinated with the new composition of the COVID-19 vaccine in the fall. The new composition of the COVID-19 vaccine is to counter the currently circulating variants Watch for news about this vaccine.
To avoid influenza (“the flu”) and its potentially severe complications, all eligible Delawareans need to be immunized with the flu vaccine every year. The U.S. Centers for Disease Control and Prevention recommends getting flu vaccinations before the end of October for the best protection as influenza activity increases.
Visit de.gov/immunizations for vaccine schedules or take the Adult or Childhood Vaccine Quiz at https://www.cdc.gov/vaccines/events/niam/index.html
To contact the Delaware Immunization Program, call 1-800-282-8672 weekdays between 8:00 a.m. and 4:30 p.m.

Family SHADE names grant awardees

Three organizations are each receiving $25,000 through the Statewide Family SHADE (Support Healthcare Alliance Delaware) Mini-Grant Program The Parent Information Center of Delaware (PIC) manages the mini-grant program, made possible by the Delaware Department of Health and Social Services, Division of Public Health’s Maternal and Child Health program.
The 2023-2024 mini grant recipients are:
• The Children's Beach House, to expand its Youth Development Program, which gives children opportunities to develop close and supportive relationships with peers and caring adult role models, so they feel safe, loved, and at home in the world. The year-round program offers support and activities for children ages 7 to 18 who have a diagnosed speech, language, hearing, or communicative delay or disability, have an Individual Education Plan, and come from underresourced homes.
• Down Syndrome Association of Delaware, to work alongside the families of over 150 youth who are younger than 17 and have Down syndrome. Families will be referred to the Down syndrome Program at Nemours, which helps families of children with Down syndrome create medical homes by connecting them with specialists and professionals who work collaboratively with parents and caregivers.
• Teach Zen Incorporated, to improve the emotional well-being of early childhood educators and children ages 3 to 5 of low-income families who are enrolled in early childhood education programs Social Emotional Learning and selfregulation techniques will be taught to them



42 Delaware Journal of Public Health - August 2023
Nemours Children’s Health offers free dog safety program
In 2022, 1,135 dog bites were reported in Delaware, according to the Division of Public Health. Many bites go unreported.
During the warmer months, Nemours Children’s Hospital in Wilmington treats on average one dog bite patient daily, according to their Trauma Program’s Injury Prevention Coordinator, Jennifer McCue, RRT, BSEd, CPST.
How to avoid dog bites
Many children who suffer dog bites know the biting dog. Supervision is the best way to prevent dog bites. Never leave a child unattended with a dog, even the family dog. Teach children how to properly interact with dogs:
• Do not approach dogs who show their teeth, are barking or growling, or who are sick or stressed. Dogs show stress by yawning, licking their lips, and showing the whites of their eyes.
• Stay away from dogs when they are playing with a toy or another dog, and when they are eating, sleeping, in their crate, hiding, or nursing puppies
• Leave a dog alone if its owner is not there or if the dog is behind a fence or tied up in a yard – even if you know the dog
• Ask the dog owner for permission to pet the dog. Not all dogs like to be petted.

Jennifer McCue of Nemours
Children’s Health, right, created a dog safety program for kids, a video, and a tip card. Facility dog Ali and handler Kelsey Cebula sometimes join her at inperson trainings Submitted photo.

Dog bites can be devastating and disfiguring to children, who suffer bites to the head and neck because of their shorter stature. When trauma and plastic surgeons requested dog bite prevention materials, McCue created a dog safety program for kids, a video, and a tip card in English and Spanish. Filmed by Nemours, the video teaches children ages 4 to 7 years and older how to properly act around dogs It is presented as a story with kidfriendly illustrations
Nemours offers the video at no cost at these links:
• English: https://youtu.be/tiDdDxjsHCg
• Spanish: https://youtu.be/nYwpq9uoLrA
McCue presents her free dog safety program to children in person or virtually within Nemours’ service area: Delaware, southeast Pennsylvania, northern Maryland, and southern New Jersey In person, she reads huge story cards and leads a game Nemours’ facility dog, Ali, sometimes joins her Kids receive a certificate, tip card, bookmark, color-changing pencil, and dog pencil eraser.
Scan this QR Code for the dog safety video.

To request more information or schedule a free program, contact McCue at 302-651-6733 or Jennifer.McCue@nemours.org
For additional dog prevention tips, visit the Delaware Office of Animal Welfare
• If it is okay to pet the dog, stand quietly to its side and do not stare into its eyes. Make a closed fist and slowly reach it out for the dog to sniff. Let the dog come to you.
• Pet the dog on the side of its neck, chest, and body – never on the top of its head or on its tail Always pet a dog in the direction that its fur grows.
• Avoid hugging or kissing the dog.
• Do not put your face close to the dog.
• Do not pet service dogs, which wear special vests or harnesses when they are working
• If chased or attacked, stay still, cross your arms across your chest, and look at the ground so the dog gets bored and leaves
If a person or dog gets bitten by a dog or was exposed to its blood or bodily fluids (such as saliva), immediately contact Delaware Animal Services at 302-255-4646.
43 The DPH Bulletin – August 2023 Page 2 of 2
Courtesy of Nemours
Lessons on Health Literacy and Communication in Post-Stroke Rehabilitation: A Primer and Proposal
Christine V. Cook, M.A., C.C.C.-S.L.P. and Rebecca Hunting Pompon, Ph.D. University of Delaware
ABSTRACT
Health literacy, or the ability to find, understand, and use information to make well-informed health decisions, has been linked to post-stroke rehabilitation outcomes. Importantly, barriers to health literacy stem from stroke survivor characteristics, clinician practices, institutional norms, as well as systemic variables. These barriers impact recovery and rehabilitation outcomes. To address these obstacles, clinicians can learn from the evidence-based practices used by speech-language pathologists in their work with stroke survivors with aphasia, a language impairment that can follow stroke. These methods to overcome communication barriers are appropriate and recommended for patients and family members regardless of stroke impairment, and include a transdisciplinary care model, multimodal approaches to patient education, along with consistent engagement with patients and their care partners. These strategies may be adopted for both personal and organizational health literacy efforts and help optimize the rehabilitation and recovery outcomes of stroke survivors with and without aphasia.
Health literacy is a multidimensional concept characterized as the ability to access, understand, appraise, and apply health information.1 The Office of Disease Prevention and Health Promotion’s (ODPHP) Healthy People 2030 initiative2 identified two types of health literacy: personal health literacy, which relates to an individual’s ability to engage with health information, and organizational health literacy, which describes how health systems equitably enable individuals to make well-informed health decisions. These definitions require both the individual making healthcare decisions and the organization providing that care to co-create an effective dialogue regarding health status. As a Social Determinant of Health, health literacy is a risk factor identified under the social and community domain. Individuals with lower health literacy skills have worse health and poorer health outcomes3 and ineffective organizational health literacy can negatively impact the health of the communities they serve.2 These effects are only compounded when organizations with low health literacy serve individuals with low health literacy.
Health literacy rates are a critical consideration in stroke prevention, management, and rehabilitation. According to the American Heart Association’s “Get with the Guidelines” initiative for stroke management, acute stroke survivors must receive education on personal risk factors for stroke, warning signs of a stroke, activation of their emergency medical system, the need for follow-up after discharge, and their prescribed medications and treatments, all before they are discharged from acute care.4 However, Sanders and colleagues identified that 59% of acute stroke survivors have inadequate or marginal health literacy.5 On average, this group retained only half of the stoke education provided to them and several respondents could not name any of their personal risk factors at discharge. Critically, this study excluded 70 of the 189 participants screened for significant cognitive deficits and receptive or global aphasia. This suggests that a much greater proportion of stroke survivors than previously reported have inadequate health literacy. Low rates of health literacy place stroke survivors, and in particular, individuals with aphasia, in an extremely vulnerable situation for preventable poorer health outcomes after stroke.
Flink and colleagues recently studied the relationship between health literacy and stroke survivor outcomes for depression, mobility, perceived stroke recovery, and perceived ability to participate in activities of daily living (ADL) 12-months poststroke.6 They found that higher relative health literacy ratings were linked with lower relative rates of post-stroke depression as well as improved mobility, and higher relative perceptions of recovery and participation in ADL, irrespective of age, sex, and education background. This study adds to the body of research that underscores the association between the health literacy of stroke survivors and optimal recovery outcomes.7–9
To make a meaningful impact on the health literacy landscape of stroke survivors, it is important to identify the specific skills involved in health literacy tasks, as well as the measures and classifications used in this domain. Accessing health information describes the patient’s ability to obtain healthcare information and resources (e.g., information shared by their clinician, pamphlet, website), as well as a patient’s ability to receive those materials in a way that promotes understanding. For example, health information should be provided in multiple languages and modalities to meet the unique needs of each learner. Comprehension occurs when the learner understands information that is presented to them in writing, shared verbally, or through a combination of communication modalities. To support health education comprehension, the American Medical Association recommends that materials be written at a 6th-8th grade reading level.10 Appraising health information requires an individual to decide if the information is reliable and valid and how it might relate to their unique health circumstances. Finally, individuals are asked to synthesize and apply the information obtained through these sequential steps in a meaningful way to make well-informed health decisions. Depending on the source, additional domains in this model can include numeracy, or an understanding of measurements used in healthcare, and media literacy.
44 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.010
The US Department of Education and the National Center for Education Statistics conducted the National Assessment of Adult Literacy (NAAL), in which respondents were given ratings of below basic, basic, intermediate, and proficient in their print health literacy and their numeracy. Table 1 provides examples of the skills which accompanied each level of health literacy in this survey.
Table 1. Adapted from the National Assessment of Adult Literacy (NAAL) report,11 U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics, 2003 National Assessment of Adult Literacy.
process and its jargon (e.g., aphasia or hemiparesis), health literacy for these topics may improve. The recovery prognosis for the language and cognitive sub skills involved in health literacy is especially interesting when examined through the lens of aphasia, a language disorder which can occur after a stroke. Speech-Language Pathologists have been engaging in this work for decades and can provide insights into meaningful health literacy gains for stroke survivors with and without aphasia.
A PRIMER AND PROPOSAL FOR STROKE REHABILITATION CLINICIANS
Health Literacy
Level Print Health Literacy Numeracy
Below basic Locating easily identifiable information in short documents and charts.
Identifying numbers and performing concrete and regular math related to healthcare (e.g., how often should someone have a certain healthcare test).
Effective health literacy is critical to stroke recovery and rehabilitative success, so how can clinicians support these skills, especially given the complexity of health literacy and its multifaceted solutions? In general, these strategies fall into the who and the how of health literacy, through 1) using a transdisciplinary model of stroke intervention, 2) integrating supportive communication approaches in patient education, and 3) acknowledging each stroke survivor as an expert member of the care team.
Basic Reading and understanding basic information in short documents and charts.
Intermediate Read and understand moderately dense text and complex documents.
Using easily identifiable quantitative information and completing one-step math equations with this information.
Locate less familiar quantitative information and complete a calculation where the equation is not clearly indicated (e.g., BMI calculation).
Transdisciplinary Model of Stroke Intervention
In transdisciplinary care, healthcare providers, patients, care partners, and researchers “go beyond or transcend disciplinary boundaries” to address the needs of the individual patients and their health conditions most efficiently and effectively).13 For health literacy to be maximally effective for stroke survivors, care must be collaborative and coordinated across disciplines and beyond, actively encouraging members of the stroke team to identify and blur overlapping areas of expertise to maximize patient care and education and support high-quality patient decision-making.
Proficient Read and understand lengthy, complex, and abstract information located on multiple pieces of paper.
Locating abstract quantitative information and using it in a complex, multistep arithmetic equation. (e.g., calculating your share of health insurance costs
The Health Literacy Tool Shed (https://healthliteracy.bu.edu/all) currently provides information on 274 assessments available to measure personal health literacy. Organizational health literacy assessments are not as widely available; however, this landscape is changing.12 Two commonly used tools to assess personal health literacy are the Short Assessment of Health Literacy (SAHL) and the Rapid Assessment of Health Literacy in Adult Medicine- Short Form (REALM-SF). These brief assessments measure print and oral health literacy, respectively, and identify patients at risk for low health literacy. Results from the REALM-SF also suggest what levels of supports might be successful. These assessments are quick and easy to administer; however, this cursory view comes at a cost. These tools do not robustly examine the sensory, cognitive, and linguistic processes required to engage in the health literacy process. Additionally, for these ratings to be valid for stroke survivors, they must be administered at multiple time points in stroke recovery. As a stroke survivor becomes more familiar with the rehabilitation
Patient education is within the scope of practice for most, if not all, healthcare providers. In a transdisciplinary model, no one team member bears the full responsibility of patient education. This approach is particularly important when the team is working with an individual with aphasia, but many other patients and their families require measures to support health literacy. For example, Chen and colleagues examined the experiences of first-time stroke survivors and their families as they transitioned between levels of care following their stroke event.14 Although participants appreciated the role rehabilitation nurses played in care coordination and stroke education, they reported not understanding much about their stroke and rehabilitation plan and expressed concern for a lack of care continuity in the transition between acute care to rehabilitation settings. A coordinated, transdisciplinary approach to stroke management and personal health literacy supports patients’ understanding of and engagement in the stroke recovery process.
Speech-language pathologists (SLPs), as experts in communication, are a central part of a stroke transdisciplinary team. SLPs can identify strategies to communicate essential recommendations to stroke survivors. These strategies include, but are not limited to, assessing of language and cognitive skills, identifying communication abilities and challenges, and providing specific, multi-modal communication techniques to maximize patient-clinician information exchange. For example, if an individual with aphasia is unable to understand complex spoken language, but they can read short sentences and key words quickly
45
and accurately, this strength can be leveraged to support the patient in meaningful participation in their recovery. Importantly, stroke survivors without aphasia may also benefit from this type of support. For example, patients (and family members) may be distressed about their health status as well as overwhelmed by the unfamiliar acute care setting, with its startling ambient noise (e.g., alarms, announcements, monitors) and frequent distractions (e.g., team members coming and going). Speaking in (respectful, nonpatronizing) short sentences, writing key words, and summarizing key points can help patients and care partners attend to and comprehend the information shared in a distracting setting. Once the patient’s optimal modalities of communication are identified, SLPs will communicate these findings with the transdisciplinary stroke team, recommend opportunities to practice strategy use, and optimize educational materials – in collaboration with other members of the care team – to support adherence to discharge recommendations. Overall, the transdisciplinary care team’s collaboration combined with the integrated communication expertise of the SLP can move stroke survivors closer to effective self-management of their recovery of post stroke.
Supportive Communication Approaches for Patient Education
Healthcare providers should receive direct instruction on communication techniques that can enhance health literacy for all patients. The FRAME model for patient communication and education was developed by Baylor and colleagues and implemented for medical students interacting with stroke survivors with aphasia and other communication disorders.15,16 During this model’s development, students watched a short, preparatory video followed by a 2-hour training. This seminar resulted in a statistically significant increase in medical students’ confidence and efficacy when working with patients with varying communication skills and styles. Specifically, the FRAME model encourages healthcare providers to take the following steps when communicating with patients:
1). Familiarize yourself with how your patient communicates BEFORE starting the interaction. This includes obtaining or preparing communication supports before your discussion with the patient. For example, a provider might read a team or SLP note about communication strengths and challenges and grab a dry erase marker and wipe board before heading in to talk to a patient and provide written key words.
2) Reduce your rate of speech to support your communication partners. It can be challenging to work in a fast-paced setting and commit to a slower rate of speech; however, this strategy improves the patient’s comprehension of your education, ultimately decreasing their need for information repetition in the future.
3) Assist the patient with communication. Have supportive communication materials on hand, such as previously mentioned wipe board and marker, a page with Yes / No written to use for pointed responses, and readiness to use gestures to support your verbal message. In moments of communication breakdowns, simply relay “I’m sorry, I don’t understand” then try a new strategy to facilitate communication. It is also helpful to verbally acknowledge what you did understand by using short paraphrases or summaries of patient’s utterances.
4) Mix your communication methods to support effective communication. Write one or two key words to orient the patient and care partners to the topic of the conversation (e.g., “going home”). Provide a brief written summary of plain language points (guidance provided in the next section) to ensure that information is salient and accessible.
5) Engage your patient to respect their autonomy. While stroke care providers educate patients daily about stroke rehabilitation and recovery, the patient is the expert of their life and experiences, and their perspective is essential. Speak directly with the patient, when at all possible, to ensure that the patient feels acknowledged, included, and worthy of respect during all interactions.
The FRAME model provides a foundation for effective communication exchanges. In addition to the basic approach in FRAME, speech-language pathologists employ evidence-based strategies to support spoken and written education for stroke survivors with and without aphasia.
Spoken/Conversational Presentation of Patient Information and Education
Most of the time, clinicians share information verbally with their patients and there are a few key concepts which can maximize the impact of the health education they provide.
Consider HOW You Communicate
Communicating with patients and care partners often requires clinicians to use shorter and simpler sentences, as mentioned previously. Clinicians should also pause periodically to allow for information processing and patient questions. Although using jargon may have ensured good grades on qualifying examinations, minimizing, or eliminating jargon and providing relatable explanations can foster understanding with patients. It is also critical to consider the patient’s basic sensory needs for aided communication. Are hearing aids and/or glasses needed? Are they on the patient and turned on? Do they need to be cleaned or require new batteries? When left unaddressed, these factors can have a significant impact on the patient’s ability to learn.
Facilitate Adequate Health Literacy
Literature shows that learners appreciate multiple repetitions of essential information (e.g., medication directions, follow up visits, exercise directions). Repeated information can be phrased differently to support comprehension and the learning style of your patient. Additionally, consider providing multiple opportunities for the patient to ask questions and/or using a respectful, non-patronizing “teach back” method to facilitate patient comprehension. When using “teach back,” it can help to have the clinician take responsibility for use of medical jargon unfamiliar to the patient. “Teach back” has been successful when the clinician has used language that resonates with the patient and the patient indicates full comprehension of the relayed information. If there are lapses in the education, the onus is on the clinician to make the repair.
Written Presentation of Patient Information and Education
Most organizations provide written educational material such as pamphlets, brochures, websites, and handouts to reinforce information shared verbally with the patient. Studies show that many of these documents do not meet the literacy levels of the general population and even specific materials
46 Delaware Journal of Public Health - August 2023
designed for individuals with aphasia may not adequately support comprehension.17 Azios and colleagues found that many educational materials for stroke survivors with aphasia required 13 to 16 years of formal education to read and understand.18 To improve accessibility of this information, they suggest collaborating with speech-language pathologists to employ effective communication supports for stroke survivors with aphasia and their care partners. Rose and colleagues demonstrated that both individuals with and without aphasia after stroke had improved comprehension of brochures and handouts when written language strategies were in place, such as highlighting keywords and adding picture supports.19 Moreover, Herbert, et al. reported that font size, concept presentation, and graphics have the potential to significantly improve written material comprehension.20 Recently, Saylor and colleagues examined how well stroke survivors with and without aphasia understand a standard pharmacy medication handout compared to an aphasia-friendly version with features described above.21 Their results indicated that both participant groups demonstrated improved comprehension, supporting the idea that aphasiafriendly education materials are beneficial for a broader audience.
Highlighted recommendations to optimize written health information for stroke survivors with and without aphasia are outlined here19,22–24:
Reading Level
All printed health education material should be consistent with a 5th or 6th grade reading level,17 considered slightly below the national average reading level of 7th-8th grade. To achieve a 5th or 6th grade reading level, printed education should feature simple words and short sentences to limit the amount of text on the page. Sentences should have no more than 15 words each and just as with spoken language, medical jargon should be avoided. Simplified vocabulary and syntax in titles and headings are also helpful. A few online readability tools are available to calculate reading level.
Virtual resources, such as informational websites, have even more facets to consider, such as the readability, validity, and userfriendliness of the site.25 To measure the readability of a website, Flesch-Kincaid Reading Ease and Grade Level measurements can be calculated (online tools are available), while the SPAT (Site, Publisher, Audience, and Timeliness) and SAM (Suitability of Materials) indices can support the development of stroke survivor friendly web-based resources.
Use of Images/Graphics
Research demonstrates that age-appropriate graphics and pictures strongly support written language comprehension. Graphics should be selected from a professional photo library and the content should be unambiguous, minimizing unnecessary background details. Each picture should feature short captions to describe the content. Ideally, printed education should be on a white background with a contrasting color background and white lettering setting the title of the educational handout apart.20
Other Visual Presentation Considerations
Patients prefer the use of large and standard san serif fonts.20 For example, a title can be printed in Arial Black in 24-point, while content sentences can be written in Arial 14-point font.
Highlighting (bold, italicize) important terms and information
can draw attention to key content, and blank white space on a page facilitates comprehension and space for writing down questions and clarifying points.
Recent innovations to support health literacy, such as the use of virtual reality in clinical education of stroke survivors,26 apps for medication management adapted to aphasia-friendly standards,27 pre-visit digital checklists and tools to support informed discussions related to chronic health management,28 and short video-based education modules29 have also incorporated many of the recommendations for aphasia-friendly communication and optimal health literacy.
Cultural considerations are included by some as an important facet of health literacy initiatives. Of note, Appalasamy and colleagues created culturally and linguistically inclusive videos that featured vignettes of stroke survivors speaking several languages and dialects to provide short education about stroke management in their own words.30 Importantly, when stroke survivors are presented with auditory education, supplemented by written keywords, they can comprehend with increased accuracy and speed.31 The guidelines and considerations described above for written educational materials can bolster an organizations’ efforts to create accessible health information and bridge the health literacy gap for stroke survivors; however, there is no substitute for personal interactions with stroke survivors and their care partners.
Stroke Survivors: Expert Members of the Care Team Individuals with aphasia, when asked about their post stroke experiences with clinical providers, reported their desire to be an active part of their medical care and decisions.32 Furthermore, during times of communication breakdowns, stroke survivors and care partners appreciated physicians who attempt to communicate differently or navigate the breakdown, as opposed to ignoring unsuccessful communication or communicating only with the care partner.33 When communication was directed only to family members, some participants believed that their involvement was not beneficial despite their best efforts. Stroke survivors and their care partners also acknowledged that physicians often appeared to try their best to communicate; however, ineffective communication can damage a provider-patient relationship and therefore optimal stroke recovery. Bottomline, clinicians must work to establish a trusting partnership with each patient and support stroke survivors to be their own best advocates. This effort starts by observing the needs of the patient and adjusting the supportive communication approach accordingly.
It is also important for clinicians to remember that stroke recovery is not linear. For example, most individuals with aphasia continue to see gains in their language impairments – even 20 or more years following the initial stroke event. Therefore, members of the care team need to dynamically adjust their communication approach depending on the communication abilities of the patient at the present time.34 Furthermore, aphasia is an impairment that can vary somewhat throughout each day. Clinicians may witness significant shifts in an individual’s ability to understand or respond to health information, and these shifts relate to factors such as level of fatigue, stress, or environmental distraction. Each of these factors also may impact stroke survivors without aphasia as well; therefore, the clinician’s time and care to ensure comprehension is never wasted.
47
FUTURE DIRECTIONS
Although this article focused on the importance of health literacy in stroke recovery, future directions should include stroke prevention-focused health literacy. In the U.S., the annual economic burden of stroke is estimated at 49.8 billion dollars,35 and the economic burden of living with aphasia is estimated to be over 15.8 million dollars.36 Since individuals with poor health literacy are at greater risk to experience cardiovascular events,8 expanded systemic efforts to educate both stroke survivors and the public about modifiable stroke risks is critical. Speech-language pathologists are uniquely qualified to address approaches to improving health literacy (e.g., accessing, understanding, appraising, and applying health information), and as communication experts, SLPs are important collaborators in the development of meaningful and accessible healthcare education – but have been underutilized in this role to date. Imagine the human and financial capital saved by implementing an inexpensive and targeted prevention approach centered around health literacy -- it is certainly a proposal worth considering.
CONCLUSION
Stroke survivors, including individuals with aphasia, have an increased risk for low levels of health literacy and associated poor health outcomes. A transdisciplinary health team that integrates the communication expertise of the speech-language pathologist can support both personal and organizational health literacy efforts to improve patient-provider communication related to stroke prevention, management, and recovery. In addition, all members of the transdisciplinary team can dynamically apply multimodal supportive communication approaches to improve patient comprehension, engagement, and independent decision making. Many of the approaches described in this paper can benefit not just individuals with aphasia but many other stroke survivors and their families. Finally, there is no substitute for deliberate and direct communication with stroke survivors and their care partners as expert members of the care team. Small adjustments in the clinician’s communicative approach can support stroke survivors as they access, comprehend, appraise, and apply essential health information to make well informed decisions about their care and recovery after a stroke.
Ms. Cook may be contacted at cvcook@udel.edu
REFERENCES
1. Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H., & the (HLS-EU) Consortium Health Literacy Project European. (2012, January 25). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80.
https://doi.org/10.1186/1471-2458-12-80
2 Office of Disease Prevention and Health Promotion. (n.d.). Health literacy. Healthy People 2030. U.S. Department of Health and Human Services. https://health.gov/healthypeople/priority-areas/social-determinantshealth/literature-summaries/health-literacy
3 Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011, July 19). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155(2), 97–107
https://doi.org/10.7326/0003-4819-155-2-201107190-00005
4 American Heart Association. (2003). Get with the guidelines. https://www.heart.org/en/professional/quality-improvement/get-withthe-guidelines
5. Sanders, K., Schnepel, L., Smotherman, C., Livingood, W., Dodani, S., Antonios, N., . . . Silliman, S. (2014, April 10). Assessing the impact of health literacy on education retention of stroke patients. Preventing Chronic Disease, 11(11), 130259. https://doi.org/10.5888/pcd11.130259
6 Flink, M., Lindblom, S., von Koch, L., Carlsson, A. C., & Ytterberg, C. (2023, February 21). Health literacy is associated with less depression symptoms, higher perceived recovery, higher perceived participation, and walking ability one year after stroke - a cross-sectional study. Topics in Stroke Rehabilitation, 21, 1–7 https://doi.org/10.1080/10749357.2023.2178133
7. Appleton, S., Biermann, S., Hamilton-Bruce, A., Piantadosi, C., Tucker, G., Koblar, S., & Adams, R. (2015, April). Functional health literacy is significantly associated with risk factors for stroke in a population sample. Int J Stroke, 10(3), E23. https://doi.org/10.1111/ijs.12425
8 Magnani, J. W., Mujahid, M. S., Aronow, H. D., Cené, C. W., Dickson, V. V., Havranek, E., Willey, J. Z., & the American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Peripheral Vascular Disease; Council on Quality of Care and Outcomes Research; and Stroke Council. (2018, July 10). Health literacy and cardiovascular disease: Fundamental relevance to primary and secondary prevention. A scientific statement from the American Heart Association. Circulation, 138(2), e48–e74. https://doi.org/10.1161/CIR.0000000000000579
9. Hahn, E. A., Magasi, S. R., Carlozzi, N. E., Tulsky, D. S., Wong, A., Garcia, S. F., Heinemann, A. W. (2017, June 14). Health and functional literacy in physical rehabilitation patients. Health Literacy Research and Practice, 1(2), e71–e85 https://doi.org/10.3928/24748307-20170427-02
10 Barry, D. (2007). Health literacy and patient safety: help patients understand. Manual for clinicians (2nd ed.). American Medical Association Foundation.
11. Kutner, M., Greenberg, E., Jin, Y., & Paulsen, C. (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483
12 Bremer, D., Klockmann, I., Jaß, L., Härter, M., von dem Knesebeck, O., & Lüdecke, D. (2021, July 6). Which criteria characterize a health literate health care organization? - a scoping review on organizational health literacy. BMC Health Services Research, 21(1), 664 https://doi.org/10.1186/s12913-021-06604-z
13. Newhouse, R. P., & Spring, B. (2010, Nov-Dec). Interdisciplinary evidence-based practice: Moving from silos to synergy. Nursing Outlook, 58(6), 309–317 https://doi.org/10.1016/j.outlook.2010.09.001
14 Chen, L., Xiao, L. D., & De Bellis, A. (2016, January). Firsttime stroke survivors and caregivers’ perceptions of being engaged in rehabilitation. Journal of Advanced Nursing, 72(1), 73–84 https://doi.org/10.1111/jan.12819
48 Delaware Journal of Public Health - August 2023
15 Baylor, C., Burns, M., McDonough, K., Mach, H., & Yorkston, K. (2019, February 21). Teaching medical students skills for effective communication with patients who have communication disorders. Am J Speech Lang Pathol, 28(1), 155–164 https://doi.org/10.1044/2018_AJSLP-18-0130
16 Mach, H., Baylor, C., Burns, M., & Yorkston, K. (2022, January). Training students from rehabilitation professions on communicating with patients with communication disorders. PM R, 14(1), 58–67.
https://doi.org/10.1002/pmrj.12580
17. Doak, L. G., Doak, C. C., & Meade, C. D. (1996, September). Strategies to improve cancer education materials. Oncology
Nursing Forum, 23(8), 1305–1312
18 Azios, J. H., Bellon-Harn, M., Dockens, A. L., & Manchaiah, V. (2019, February). Quality and readability of Englishlanguage internet information for aphasia. Int J Speech Lang Pathol, 21(1), 1–9.
https://doi.org/10.1080/17549507.2017.1362034
19. Rose, T., Worrall, L., & McKenna, K. (2003). The effectiveness of aphasia-friendly principles for printed health education materials for people with aphasia following stroke
Aphasiology, 17(10), 947–963
https://doi.org/10.1080/02687030344000319
20 Herbert, R., Gregory, E., & Haw, C. (2019). Collaborative design of accessible information with people with aphasia. Aphasiology, 33(12), 1504–1530.
https://doi.org/10.1080/02687038.2018.1546822
21. Saylor, A., Wallace, S., Brown, E., & Schreiber, J. (2022). Aphasia-friendly medication instructions: Effects on comprehension in persons with and without aphasia. Aphasiology, 36, 251–267
https://doi.org/10.1080/02687038.2021.1873907
22. Rose, T. A., Worrall, L. E., Hickson, L. M., & Hoffmann, T. C. (2012, February). Guiding principles for printed education materials: Design preferences of people with aphasia. Int J Speech Lang Pathol, 14(1), 11–23
https://doi.org/10.3109/17549507.2011.631583
23 Brennan, A., Worrall, L., & McKenna, K. (2005). The relationship between specific features of aphasia friendly written material and comprehension of written material for people with aphasia: An exploratory study. Aphasiology, 19(8), 693–711
https://doi.org/10.1080/02687030444000958
24 Hoffmann, T., & McKenna, K. (2006, March). Analysis of stroke patients’ and carers’ reading ability and the content and design of written materials: Recommendations for improving written stroke information. Patient Education and Counseling, 60(3), 286–293
https://doi.org/10.1016/j.pec.2005.06.020
25 Abou-Diab, S., Moser, D., & Atcherson, S. (2019). Evaluation of the readability, validity, and user-friendliness of written web-based patient education materials for aphasia. Aphasiology, 33, 187–199.
https://doi.org/10.1080/02687038.2018.1458069
26. Balsam, P., Borodzicz, S., Malesa, K., Puchta, D., Tymińska, A., Ozierański, K., Opolski, G. (2019). OCULUS study: Virtual reality-based education in daily clinical practice. Cardiology Journal, 26(3), 260–264
https://doi.org/10.5603/CJ.a2017.0154
27 Rai, T., Morton, K., Roman, C., Doogue, R., Rice, C., Williams, M., Hinton, L. (2021, April). Optimizing a digital intervention for managing blood pressure in stroke patients using a diverse sample: Integrating the person-based approach and patient and public involvement. Health Expect, 24(2), 327–340.
https://doi.org/10.1111/hex.13173
28. Kjörk, E. K., Sunnerhagen, K. S., Lundgren-Nilsson, Å., Andersson, A. K., & Carlsson, G. (2022, June 3). Development of a digital tool for people with long-term conditions using stroke as a case example: Participatory design approach. JMIR Human Factors, 9(2), e35478.
https://doi.org/10.2196/35478
29. Denny, M. C., Vahidy, F., Vu, K. Y., Sharrief, A. Z., & Savitz, S. I. (2017, March 23). Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS One, 12(3), e0171952
https://doi.org/10.1371/journal.pone.0171952
30 Appalasamy, J. R., Joseph, J. P., Seeta Ramaiah, S., Md Zain, A. Z., Quek, K. F., & Tha, K. K. (2020, July 10). Video narratives intervention among stroke survivors: Feasibility and acceptability study of a randomized controlled trial. JMIR Aging, 3(2), e17182.
https://doi.org/10.2196/17182
31 Knollman-Porter, K., Wallace, S. E., Brown, J. A., Hux, K., Hoagland, B. L., & Ruff, D. R. (2019, August 9). Effects of written, auditory and combined modalities on comprehension by People with Aphasia. Am J Speech Lang Pathol, 28(3), 1206–1221.
https://doi.org/10.1044/2019_AJSLP-19-0013
32 Burns, M., Baylor, C., Dudgeon, B., Starks, H., & Yorkston, K. (2015). Asking the stakeholders: perspectives of individuals with aphasia, their family members, and physicians regarding communication in medical interactions Am J Speech Lang Pathol, 24, 341–357.
https://doi.org/10.1044/2015_AJSLP-14-0051
33. Hoffman, J. M., Yorkston, K. M., Shumway-Cook, A., Ciol, M. A., Dudgeon, B. J., & Chan, L. (2005, August). Effect of communication disability on satisfaction with health care: A survey of medicare beneficiaries. American Journal of SpeechLanguage Pathology, 14(3), 221–228.
https://doi.org/10.1044/1058-0360(2005/022)
34. Kjellén, E., Laakso, K., & Henriksson, I. (2017, September). Aphasia and literacy-the insider’s perspective. Int J Lang Commun Disord, 52(5), 573–584
https://doi.org/10.1111/1460-6984.12302
35 Virani, S. S., Alonso, A., Aparicio, H. J., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Tsao, C. W., & the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2021, February 23). Heart disease and stroke statistics-2021 update: A report from the American Heart Association. Circulation, 143(8), e254–e743.
https://doi.org/10.1161/CIR.0000000000000950
36. Jacobs, M., Evans, E., & Ellis, C. (2023). Determinants of healthcare expenditures among PWA: Importance of race, sex, residence and aphasia type. Aphasiology, 37(1), 25–38
https://doi.org/10.1080/02687038.2021.1985426
49
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
HEALTH MATTERS
MAY/JUNE 2023
MAY/JUNE 2023
MAY/JUNE 2023
Studying the effect of pesticides on Thai farmers and their families…p. 5
Studying the effect of pesticides on Thai farmers and their families…p. 5
Studying the effect of pesticides on Thai farmers and their families…p. 5
Studying the effect of pesticides on Thai farmers and their families…p. 5
Paying it forward: Fogarty Fellows & Scholars at 20
Paying it forward: Fogarty Fellows & Scholars at 20
By Judy Coan-Stevens
Paying it forward: Fogarty Fellows & Scholars at 20
Paying it forward: Fogarty Fellows & Scholars at 20
By Judy Coan-Stevens
By Judy Coan-Stevens
To mark the 20th Anniversary of its flagship Global Health Fellows and Scholars program, now known as LAUNCH, Fogarty hosted a commemorative event on the NIH campus and a retrospective panel at the 2023 CUGH conference in April. At both events, the former fellows and scholars emphasized the importance of mentorship to the LAUNCH program and how the connections they made in their “Fogarty year” have sustained them through their career journeys.
To mark the 20th Anniversary of its flagship Global Health Fellows and Scholars program, now known as LAUNCH, Fogarty hosted a commemorative event on the NIH campus and a retrospective panel at the 2023 CUGH conference in April. At both events, the former fellows and scholars emphasized the importance of mentorship to the LAUNCH program and how the connections they made in their “Fogarty year” have sustained them through their career journeys.
By Judy Coan-Stevens
To mark the 20th Anniversary of its flagship Global Health Fellows and Scholars program, now known as LAUNCH, Fogarty hosted a commemorative event on the NIH campus and a retrospective panel at the 2023 CUGH conference in April. At both events, the former fellows and scholars emphasized the importance of mentorship to the LAUNCH program and how the connections they made in their “Fogarty year” have sustained them through their career journeys.
To mark the 20th Anniversary of its flagship Global Health Fellows and Scholars program, now known as LAUNCH, Fogarty hosted a commemorative event on the NIH campus and a retrospective panel at the 2023 CUGH conference in April. At both events, the former fellows and scholars emphasized the importance of mentorship to the LAUNCH program and how the connections they made in their “Fogarty year” have sustained them through their career journeys.




The commemoration kicked off with a half-day event on the main NIH campus featuring a keynote by former Fogarty Director Roger Glass, two panels of alumni co-moderated by NIH leaders, and concluding thoughts and remarks by Sten Vermund of the Yale School of Public Health and Acting Fogarty Director Peter Kilmarx.
The commemoration kicked off with a half-day event on the main NIH campus featuring a keynote by former Fogarty Director Roger Glass, two panels of alumni co-moderated by NIH leaders, and concluding thoughts and remarks by Sten Vermund of the Yale School Public Health and Acting Fogarty Director Peter Kilmarx.
The commemoration kicked off with a half-day event on the main NIH campus featuring a keynote by former Fogarty Director Roger Glass, two panels of alumni co-moderated by NIH leaders, and concluding thoughts and remarks by Sten Vermund of the Yale School of Public Health and Acting Fogarty Director Peter Kilmarx.
The commemoration kicked off with a half-day event on the main NIH campus featuring a keynote by former Fogarty Director Roger Glass, two panels of alumni co-moderated by NIH leaders, and concluding thoughts and remarks by Sten Vermund of the Yale School of Public Health and Acting Fogarty Director Peter Kilmarx.




Eight more program alumni were featured on a panel at CUGH 2023 moderated by Roger Glass. The panel also included the presentation of a recent program review led by Fogarty’s Celia Wolfman Katz. From the survey she and her team conducted it was clear “mentorship is the backbone of this program.” Nearly 90% of respondents stated that their mentors played a significant role in their career trajectory. Alumni panelists at both events noted the impact mentors had during their time with the program and beyond.
Eight more program alumni were featured on a panel at CUGH 2023 moderated by Roger Glass. The panel also included the presentation of a recent program review led by Fogarty’s Celia Wolfman Katz. From the survey she and her team conducted it was clear “mentorship is the backbone of this program.” Nearly 90% of respondents stated that their mentors played a significant role in their career trajectory. Alumni panelists at both events noted the impact mentors had during their time with the program and beyond.
Eight more program alumni were featured on a panel at CUGH 2023 moderated by Roger Glass. The panel also included the presentation of a recent program review led by Fogarty’s Celia Wolfman Katz. From the survey she and her team conducted it was clear “mentorship is the backbone of this program.” Nearly 90% of respondents stated that their mentors played a significant role in their career trajectory. Alumni panelists at both events noted the impact mentors had during their time with the program and beyond.
Eight more program alumni were featured on a panel at CUGH 2023 moderated by Roger Glass. The panel also included the presentation of a recent program review led by Fogarty’s Celia Wolfman Katz. From the survey she and her team conducted it was clear “mentorship is the backbone of this program.” Nearly 90% of respondents stated that their mentors played a significant role in their career trajectory. Alumni panelists at both events noted the impact mentors had during their time with the program and beyond.
Dr. Anubha Agarwal, a 2017 fellow and assistant professor and co-director of the Program in Global Cardiovascular Health at Washington University, noted that because of the support from her Fogarty mentorship team, “The leap from the Fogarty fellowship to a career development award was very contiguous.”
Dr. Anubha Agarwal, a 2017 fellow and assistant professor and co-director of the Program in Global Cardiovascular Health at Washington University, noted that because of the support from her Fogarty mentorship team, “The leap from the Fogarty fellowship to a career development award was very contiguous.”
Dr. Anubha Agarwal, a 2017 fellow and assistant professor and co-director of the Program in Global Cardiovascular Health at Washington University, noted that because of the support from her Fogarty mentorship team, “The leap from the Fogarty fellowship to a career development award was very contiguous.”
Dr. Anubha Agarwal, a 2017 fellow and assistant professor and co-director of the Program in Global Cardiovascular Health at Washington University, noted that because of the support from her Fogarty mentorship team, “The leap from the Fogarty fellowship to a career development award was very contiguous.”
Dr. Roxanna Garcia, a 2019 neurology fellow, who is currently an assistant professor at Northwestern University, reiterated the need to sustain those relationships to continue
Dr. Roxanna Garcia, a 2019 neurology fellow, who is currently an assistant professor at Northwestern University, reiterated the need to sustain those relationships to continue
Dr. Roxanna Garcia, a 2019 neurology fellow, who is currently an assistant professor at Northwestern University, reiterated the need to sustain those relationships to continue
Dr. Roxanna Garcia, a 2019 neurology fellow, who is currently an assistant professor at Northwestern University, reiterated the need to sustain those relationships to continue




receiving support. It’s what 2021 nursing fellow Ivan Segawa called “lifelong mentorship”—mentorship beyond the “transactional” mentorship that’s often limited to one project or fellowship.
receiving support. It’s what 2021 nursing fellow Ivan Segawa called “lifelong mentorship”—mentorship beyond the “transactional” mentorship that’s often limited to one project or fellowship.
receiving support. It’s what 2021 nursing fellow Ivan Segawa called “lifelong mentorship”—mentorship beyond the “transactional” mentorship that’s often limited to one project or fellowship.
receiving support. It’s what 2021 nursing fellow Ivan Segawa called “lifelong mentorship”—mentorship beyond the “transactional” mentorship that’s often limited to one project or fellowship.
Dr. Nauzley Abedini, a 2012 scholar, said, “I think one of the key factors in the evolution of my career was having mentors from the very beginning who have been dedicated to my professional growth.” But sometimes you need to differentiate between a “project manager” and a “mentor,” per Dr. Richard van Zyl-Smit, a South African pulmonologist and 2009 fellow: “the project manager is there to get the project done, and the mentor is there to look after you.”
Dr. Nauzley Abedini, a 2012 scholar, said, “I think one of the key factors in the evolution of my career was having mentors from the very beginning who have been dedicated to my professional growth.” But sometimes you need to differentiate between a “project manager” and a “mentor,” per Dr. Richard van Zyl-Smit, a South African pulmonologist and 2009 fellow: “the project manager is there to get the project done, and the mentor is there to look after you.”
Dr. Nauzley Abedini, a 2012 scholar, said, “I think one of the key factors in the evolution of my career was having mentors from the very beginning who have been dedicated to my professional growth.” But sometimes you need to differentiate between a “project manager” and a “mentor,” per Dr. Richard van Zyl-Smit, a South African pulmonologist and 2009 fellow: “the project manager is there to get the project done, and the mentor is there to look after you.”
Dr. Nauzley Abedini, a 2012 scholar, said, “I think one of the key factors in the evolution of my career was having mentors from the very beginning who have been dedicated to my professional growth.” But sometimes you need to differentiate between a “project manager” and a “mentor,” per Dr. Richard van Zyl-Smit, a South African pulmonologist and 2009 fellow: “the project manager is there to get the project done, and the mentor is there to look after you.”
Many alumni are now mentors themselves, including moderator Dr. Satish Gopal, a 2012 fellow who went on to mentor many subsequent cohorts of Fogarty fellows. 2015 fellow Dr. Christine Sekaggya-Wiltshire of Uganda has mentored dozens of Fogarty fellows since her training, building a network in part through her mentees. “The research skills that you get from a program like Fogarty enables you to mentor anyone in any field.”
Many alumni are now mentors themselves, including moderator Dr. Satish Gopal, a 2012 fellow who went on to mentor many subsequent cohorts of Fogarty fellows. 2015 fellow Dr. Christine Sekaggya-Wiltshire of Uganda has mentored dozens of Fogarty fellows since her training, building a network in part through her mentees. “The research skills that you get from a program like Fogarty enables you to mentor anyone in any field.”
Many alumni are now mentors themselves, including moderator Dr. Satish Gopal, a 2012 fellow who went on to mentor many subsequent cohorts of Fogarty fellows. 2015 fellow Dr. Christine Sekaggya-Wiltshire of Uganda has mentored dozens of Fogarty fellows since her training, building a network in part through her mentees. “The research skills that you get from a program like Fogarty enables you to mentor anyone in any field.”
Many alumni are now mentors themselves, including moderator Dr. Satish Gopal, a 2012 fellow who went on to mentor many subsequent cohorts of Fogarty fellows. 2015 fellow Dr. Christine Sekaggya-Wiltshire of Uganda has mentored dozens of Fogarty fellows since her training, building a network in part through her mentees. “The research skills that you get from a program like Fogarty enables you to mentor anyone in any field.”
CUGH returns, in real life
• Reimagining global health in the 21st century
environmental impact
• At the intersection of climate, nutrition & health
• Reducing eye surgery’s environmental impact
Read more on pages 6 – 9
Read more on pages 6 – 9
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS MAY/JUNE 2023 CUGH returns, in real life • Reimagining global health in the 21st century • At the intersection of climate, nutrition & health • Reducing eye surgery’s environmental impact Read more on pages 6 – 9 GLOBAL
Alumni present at the closing panel of the Fogarty Global Health Fellows & Scholars/ LAUNCH 20th Anniversary event in April. Fogarty International Center
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue
FOCUS
LAUNCH 20th Anniversary event in April.
Fogarty International Center
www.fic.nih.gov FOGARTY
•
INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS
INTERNATIONAL CENTER
NATIONAL
CUGH returns, in real life • Reimagining global health in the 21st century • At the intersection of climate, nutrition & health • Reducing eye surgery’s environmental impact Read more on pages 6 – 9
Alumni present at the closing panel of the Fogarty Global Health Fellows & Scholars/ LAUNCH 20th Anniversary event in April. Fogarty International Center
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS
CUGH returns, in real life
Reimagining global health in the 21st century
At the intersection of climate, nutrition & health
Reducing eye surgery’s
•
•
•
Alumni present at the closing panel of the Fogarty Global Health Fellows & Scholars/ LAUNCH 20th Anniversary event in April. Fogarty International Center
54 Read More on pages 55-58 50 Delaware Journal of Public Health - August 2023
Delivering hope and health care in Haiti
 By Mariah Felipe
By Mariah Felipe
When he first volunteered in Haiti during the 2010 cholera outbreak, Dr. Eric Nelson noted that his team was seeing more and more patients with avoidable dehydration whose symptoms had worsened during the overnight hours when access to medical care was unavailable. Haunted by this, Nelson, a former Fogarty Fellow who studied cholera transmission in Bangladesh, shifted his studies after completing his residency at Stanford. He moved away from the research bench towards new disciplines that allowed him to learn new approaches to addressing the logistical challenges of expanding health care access.
In 2014, an NIH Early Independence award enabled him to delve deeper into this implementation science research, ultimately leading to the creation of MotoMeds—a pediatric telemedicine and medication delivery service designed to prevent emergent illnesses from transitioning into emergencies.




Supported by Nelson’s lab at the University of Florida, MotoMeds serves children 10 and under in Haiti. From 6 p.m. every evening to 5 a.m. the following day, a call center is staffed by nurses and nurse practitioners who answer the calls of concerned parents and caretakers, with pools of motorcycle drivers on standby to transport medications or nurses. On-call physicians provide oversight for complicated cases or cases outside of the guidelines.
All of this is possible due to partnerships with the local communities and NGOs in the region that assist with needs like communication services and hiring qualified health professionals and drivers from within the country. By doing this, MotoMeds has created a mechanism to help the communities they serve while providing employment opportunities. “These opportunities enable the staff to provide for their family’s needs and grow professionally,” said Nelson, highlighting that many of the nurses were able to pursue nurse practitioner training through their engagement with MotoMeds.
The drivers are another critical resource according to Molly Klarman, Project Director for MotoMeds Haiti. “Their granular sense of the existing road networks allows them to navigate without maps or GPS, or a formal address system, using landmarks to get to patients.” Furthermore, the drivers often assist in treating mild cases by sharing video
tutorials on a tablet, illustrating how to correctly prepare and take the medication—an additional step MotoMeds hopes will improve treatment adherence for patients.
While MotoMeds has specific metrics and benchmarks they use to measure progress, like getting to a household in under two hours or looking at the rates of guideline adherence, Nelson says, “There is a more human aspect to the program which comes through in our qualitative research.”
MotoMeds surveys families, drivers, nurses, and doctors to get their feedback and help characterize the impact from a more human perspective. So far, they have found that one of the most important things MotoMeds has provided the community is hope.
“These are populations where no one has ever answered their call for help and MotoMeds is doing that,” said Nelson. ”Often, the families cry when we pick up the phone and talk with them. Hope is really the single most important thing that we deliver.”
MotoMeds hopes to establish an NGO to oversee its future operations and partner with other countries confronted by health care access challenges. The idea is that the program would be adaptable to the needs and preferences of partner countries while maintaining a research infrastructure, similar to the current setup in Haiti. Nelson stressed, “We want the operations to be fully managed by the partner country, with our support, and position the research in an equitable way.”
MAY/JUNE 2023 2
A MotoMeds driver outside of the call center in Gressier, Haiti. Drivers are a critical resource: "They can navigate without maps or GPS to get to patients."
Photo courtesy of MotoMeds
51
Facing undiagnosed diabetes in Africa
By Susan Scutti
Sub-Saharan Africa has the highest percentage of people living with undiagnosed type 2 diabetes in the world, according to the International Diabetes Federation (IDF). An estimated 54% of Africans who are living with diabetes do not know they have the illness, which is characterized by poor regulation of blood glucose (sugar) that is used by the body’s cells for energy. Too much circulating glucose leads to diabetes and its possible complications, including heart disease, renal failure, blindness, neuropathy, and lower extremity amputations.
Diagnosing diabetes in Africa is problematic due to costs and lack of access to resources. Additionally, Africans may have a different phenotype of the disease—type 2 diabetes is common in non-obese Africans—which leads to atypical biomarkers and diverging diagnostic standards. Dr. Jean de Dieu Gatete described a new strategy for diagnosing the disease, which could be of specific value to Africa, in his recent graduation speech.
Gatete is the seventh fellow in the NIMHD-NIDDKRwandan Health Program, led by Dr. Anne E. Sumner of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). It is anticipated that Gatete, who is scheduled to return to Rwanda in July 2023, could conduct similar research there, ultimately changing the trajectory, severity, and prevalence of undiagnosed diabetes in that nation.
Accessible, inexpensive solution
The best, most reliable test for diabetes, the oral glucose tolerance test (OGTT), measures how the body reacts to a solution with high glucose content called “glucola,” explained Gatete. It begins with a blood draw from a patient who’s fasted for eight hours, followed by measurement of blood glucose levels; after the patient drinks glucola, another blood draw takes place two hours later to check glucose levels. When high levels of blood sugar are seen, the patient has diabetes (or, if levels are not so high, pre-diabetes). Glucola costs $8 a bottle, prohibitively expensive in many places in subSaharan Africa according to Gatete.
Seeking a glucola alternative, the NIMHD-NIDDKRwandan Health team first tried substituting Ceres Juice, a South African brand, but found it did not identically affect blood glucose levels so could not be used for diagnosis. Next, the team mixed water and
pastry sugar (also known as confectioner’s or powdered sugar) and found a solid match to the performance of glucola. And the cost of the sugar needed for the test is less than a dollar.
To validate this work, a pastry sugar tolerance test (PSTT), which enrolls African immigrants in the U.S., is underway, said Gatete. The plan is for Gatete and others to conduct the same research in Africa. For Rwanda, a nation similar in size to the state of Maryland with a population of 14 million, the use of PSTT as a diabetes diagnostic should be within economic reach.
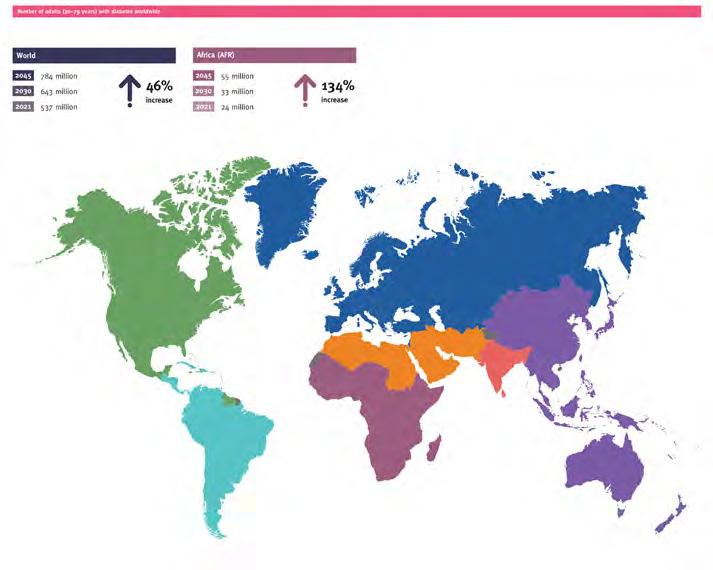
Achievement through partnership
Following Gatete’s presentation, which was part of the National Institute on Minority Health and Health Disparities (NIMHD) Seminar Series, Dr. Eliseo J. PérezStable, director of NIMHD, noted that the research is “very practical. It could impact literally hundreds of thousands of people in Africa.” Yet he raised a key question: Once diagnosed, what do you do?
Dr. Tomlin Paul, a dean at University of Global Health Equity (UGHE) in Rwanda, echoed the concerns of Pérez-Stable. He stated, “diabetes is most devastating for LMICs as approximately 80% of the 463 million adults worldwide with diabetes live in low- and middle-income countries.” Yet only one in 10 people living with diabetes receives treatment recommended by WHO guidelines, he said. “Dr. Gatete’s research initiative is of great service to the cause.”
Image courtesy of International Diabetes Federation
While the International Diabetes Federation projects a 46% increase in diabetes worldwide over the next two decades, it expects prevalence in Africa to increase by 134%.
3 MAY/JUNE 2023 Number of adults (20-79) with diabetes worldwide Diabetes around the world I 2021
52 Delaware Journal of Public Health - August 2023
PROFILE
Improving heart failure care in Southern India
Improving heart failure care in Southern India
Dr. Anubha Agarwal emigrated from India to the United States with her family when she was about 5 years old. As many immigrant families do, she spent much of her childhood going back and forth, visiting her family in India. During those trips, Agarwal realized the stark differences between the two countries. “Witnessing the inequities between the countries and within each country, I wanted to solve them. Later, I realized that I wanted to do that as a physician,” she said.
Dr. Anubha Agarwal emigrated from India to the United States with her family when she was about 5 years old. As many immigrant families do, she spent much of her childhood going back and forth, visiting her family in India. During those trips, Agarwal realized the stark differences between the two countries. “Witnessing the inequities between the countries and within each country, I wanted to solve them. Later, I realized that I wanted to do that as a physician,” she said.
During medical school, Agarwal was quickly drawn to cardiology as a specialty but felt unsure how to integrate that into her goal of solving health inequities in India. This changed once she began working with Dr. Gerald Bloomfield, one of Fogarty’s first-ever cardiology fellows, as part of AMPATH, a partnership between Moi University, Moi Teaching and Referral Hospital, Indiana University, and the Kenyan government. With Bloomfield’s mentorship and guidance, she decided to apply for a Fogarty fellowship.
During medical school, Agarwal was quickly drawn to cardiology as a specialty but felt unsure how to integrate that into her goal of solving health inequities in India. This changed once she began working with Dr. Gerald Bloomfield, one of Fogarty’s first-ever cardiology fellows, as part of AMPATH, a partnership between Moi University, Moi Teaching and Referral Hospital, Indiana University, and the Kenyan government. With Bloomfield’s mentorship and guidance, she decided to apply for a Fogarty fellowship.
The overarching goal of Agarwal’s Fogarty year was to answer the question: How can we improve heart failure care in South India? She worked in the state of Kerala, where her first step was to conduct a systematic review of existing heart failure intervention programs. While many improvement programs existed, all had been studied and refined in high-income countries, making it a challenge to understand how they might work in low-income settings. Agarwal and her colleagues then took that data and conducted qualitative interviews with physicians, nurses, patients, and pharmacists, asking them what they think needed to be done to improve heart failure care. From there, they designed their quality improvement intervention and tested it amongst 1,400 heart patients in Kerala over six months.
The overarching goal of Agarwal’s Fogarty year was to answer the question: How can we improve heart failure care in South India? She worked in the state of Kerala, where her first step was to conduct a systematic review of existing heart failure intervention programs. While many improvement programs existed, all had been studied and refined in high-income countries, making it a challenge to understand how they might work in low-income settings. Agarwal and her colleagues then took that data and conducted qualitative interviews with physicians, nurses, patients, and pharmacists, asking them what they think needed to be done to improve heart failure care. From there, they designed their quality improvement intervention and tested it amongst 1,400 heart patients in Kerala over six months.
Anubha Agarwal , PhD
Fogarty Fellow: 2017-2018
Fogarty Fellow: 2017-2018
U.S. institution: Northwestern University
U.S. institution: Northwestern University
Foreign institution: Indian National Centre for Disease Control
Research topic: Global burden of cardiovascular disease
Foreign institution: Indian National Centre for Disease Control Research topic: Global burden of cardiovascular disease
this related project are a direct extension of her Fogarty experience. Dr. Mark Huffman, a professor of medicine and co-director of Washington University's Global Health Center, is her primary mentor—and, like Bloomfield, is another of Fogarty’s first cardiology fellows. Dr. Dorairaj Prabhakaran, vice president and director of the Centre for Control of Chronic Conditions at the Public Health Foundation of India, will also serve as her mentor as he did previously during her fellowship.
this related project are a direct extension of her Fogarty experience. Dr. Mark Huffman, a professor of medicine and co-director of Washington University's Global Health Center, is her primary mentor—and, like Bloomfield, is another of Fogarty’s first cardiology fellows. Dr. Dorairaj Prabhakaran, vice president and director of the Centre for Control of Chronic Conditions at the Public Health Foundation of India, will also serve as her mentor as he did previously during her fellowship.
“My Fogarty fellowship was foundational to what I will spend the next five years of my life working on,” said Agarwal. “My Fogarty year was the most impactful year of my life, both personally and professionally.”
“My Fogarty fellowship was foundational to what I will spend the next five years of my life working on,” said Agarwal. “My Fogarty year was the most impactful year of my life, both personally and professionally.”
Today, Agarwal is working at Washington University in St. Louis as an assistant professor and co-director of their global cardiovascular health program. She spends about a quarter of her time working with patients; the rest is spent on research related to her project in Kerala. “I have progressed significantly since my Fogarty year due to phenomenal mentorship,” said Agarwal. “Now, when I think about my leadership priorities, mentorship is at the forefront.”
Today, Agarwal is working at Washington University in St. Louis as an assistant professor and co-director of their global cardiovascular health program. She spends about a quarter of her time working with patients; the rest is spent on research related to her project in Kerala. “I have progressed significantly since my Fogarty year due to phenomenal mentorship,” said Agarwal. “Now, when I think about my leadership priorities, mentorship is at the forefront.”
This marked the end of her Fogarty project, but the work on a heart program tailored for Kerala continues.
This marked the end of her Fogarty project, but the work on a heart program tailored for Kerala continues.
Using her Fogarty data, Agarwal applied for and was awarded a Pathway to Independence grant from the National Heart, Blood, and Lung Institute. With this grant, she and her team will work again in Kerala evaluating a polypill that combines four different classes of medications into one pill for patients with heart failure. Her mentors on
Using her Fogarty data, Agarwal applied for and was awarded a Pathway to Independence grant from the National Heart, Blood, and Lung Institute. With this grant, she and her team will work again in Kerala evaluating a polypill that combines four different classes of medications into one pill for patients with heart failure. Her mentors on
Agarwal is committed to her new project, global health, and her growing family, which have all come together at once. During her first stint in Kerala, Agarwal met her husband, who already lived in India. The new couple, along with their recently born child, plan to split their time between Kerala and the U.S. in the coming years.
Agarwal is committed to her new project, global health, and her growing family, which have all come together at once. During her first stint in Kerala, Agarwal met her husband, who already lived in India. The new couple, along with their recently born child, plan to split their time between Kerala and the U.S. in the coming years.
Agarwal’s advice to those considering a Fogarty fellowship: Take the risk. “It can be difficult to take a year off for your study when you are on the physician track in the U.S., but you never know where it can take you.”
Agarwal’s advice to those considering a Fogarty fellowship: Take the risk. “It can be difficult to take a year off for your study when you are on the physician track in the U.S., but you never know where it can take you.”


4
Anubha Agarwal , PhD
PROFILE
4
53
PORNPIMOL KONGTIP, PHD
Dr. Pornpimol Kongtip has served as a faculty member at Mahidol University, Thailand, for over 20 years where she chairs the Ph.D. program in occupational health and safety. Kongtip earned a Ph.D. in occupational health from McGill University, Canada, and an MS in biochemistry from Chulalongkorn University, Thailand. Her research focuses on occupational and environmental exposure assessment and biological monitoring in the general population and in workers in Thailand, with special emphasis on agriculture.

Tell us about the GEO Health Hub project. The project, which ends in July 2023, is a collaboration between Mahidol University in Thailand and University of Massachusetts Lowell in the U.S.
The focus has been to examine if pesticides alter the endocrine system, including thyroid hormone levels and cortisol levels, as well as their impact on metabolic biomarkers associated with metabolic syndrome and chronic disorders such as cardiovascular disease, diabetes, and stroke. Our research has shown that conventional (pesticide-using) farmers have significantly higher BMI, waist circumference, percentage of body fat, and total cholesterol compared to organic farmers, even after accounting for potential confounders, such as tobacco and alcohol use. Number of pesticide spray days was associated with an increasing disruption of the hypothalamic-pituitary-adrenal (HPA) axis and depression of the cortisol rhythm in Thai farmers. Pesticide-using farmers have higher thyroid hormone levels than organic farmers, and an increase in cumulative days of spraying is associated with higher levels of certain thyroid hormones.
Overall, the Hub has produced 20 peer-reviewed papers. We’ve expanded the research capacity at Mahidol to include pesticide biomarker analysis and trained our university staff, the staff of other universities, and some employees from the Ministry of Public Health. We’d planned to bring in biomarker research trainees from Vietnam, Laos, and Indonesia but with the pandemic we were limited to providing online-only training. All of these outreach efforts have increased research capabilities in Southeast Asia.
What challenges have you faced as a scientist?


Getting permission from different companies to do research on workers’ exposures to different types of chemicals inside their facilities can be difficult. Many companies don’t want you to know about major exposures or to identify health risks associated with work done in their facilities. I started looking at pesticide exposure
among rice farmers in 2007 and found that farmers were happy to work with us. I eventually began to study organophosphate (a group of chemical pesticides) exposures in pregnant women, and now I’ve conducted research in all areas of agricultural health.
One of the most rewarding aspects of our work is that, after four years of discussions, Thailand finally banned the use of the herbicide paraquat and the insecticide chlorpyrifos starting in June 2020, while limiting use of another herbicide, glyphosate. It’s difficult to get involved in politics and talk to the media, but we realized that it was important to educate politicians and the community about the risks of pesticides.
What should future research agendas include?
Industrial accident rates in Thailand are high compared to other countries, so that is an area of concern. We are also facing increasing air pollution especially during the winter. In the past we used to think that India had a serious air pollution problem, but these days Thailand is approaching that same level—above the safe limit. The Thailand agricultural sector employs over 30% of the workforce, so widespread and poorly managed use of pesticides presents a potential risk to farmers and their families but also to the general public. If farmers do not apply pesticides at the recommended rates, food residue levels (the amount of pesticide remaining in or on foods) can be quite high. All of these problems are dynamic and need to be studied.
My current research focuses on durian. People want to eat durian all year round so farmers, who want higher incomes, are making that happen. Unfortunately, pesticides must be used so durian can be grown off-season and exported.
Thailand is in a better position than other countries in our region because of our universal health coverage, which started about 10 years ago. Over time our health system has improved and now the government gives more support than initially. Still, we need to improve these systems for informal and low-income workers.
A&Q 5 54 Delaware Journal of Public Health - August 2023
FOCUS
Reimagining global health in the 21st century
By Judy Coan-Stevens
Reimagining global health in the 21st century


Over a decade ago, the Consortium of Universities for Global Health (CUGH) executive board set out to find a consensus definition of global health. Their 2009 Lancet paper, “Towards a common definition of global health,” set some parameters around what it meant. Fourteen years later, at the 2023 CUGH conference, Dr. Judith Wasserheit, Fogarty advisory board member and one of the Lancet paper authors, noted “tectonic shifts” since then, not least of which is the COVID-19 pandemic. In her introduction to the plenary session, “Reimagining global health in the 21st century,” Wasserheit noted, “While there have been advances and improvements, many communities have been left behind, and discussions about equity and decolonization have gained much more traction in recent years.”
By Judy Coan-Stevens
Over a decade ago, the Consortium of Universities for Global Health (CUGH) executive board set out to find a consensus definition of global health. Their 2009 Lancet paper, “Towards a common definition of global health,” set some parameters around what it meant. Fourteen years later, at the 2023 CUGH conference, Dr. Judith Wasserheit, Fogarty advisory board member and one of the Lancet paper authors, noted “tectonic shifts” since then, not least of which is the COVID-19 pandemic. In her introduction to the plenary session, “Reimagining global health in the 21st century,” Wasserheit noted, “While there have been advances and improvements, many communities have been left behind, and discussions about equity and decolonization have gained much more traction in recent years.”


The session was co-moderated by Wasserheit, fellow Fogarty board member Dr. Maureen Lichtveld, and Acting Fogarty Director Dr. Peter Kilmarx. The panelists were Dr. Ala Alwan, former director of WHO Eastern Mediterranean Region and former Iraqi Minister of Health; Dr. Tahmeed Ahmed, executive director of icddr,b, Bangladesh; Dr. Patricia García, former dean of Universidad Peruana Cayetano Heredia and former Minister of Health, Peru; and Dr. Melissa Salm, postdoctoral fellow at the Center for International Security & Cooperation, Stanford University.
The session was co-moderated by Wasserheit, fellow Fogarty board member Dr. Maureen Lichtveld, and Acting Fogarty Director Dr. Peter Kilmarx. The panelists were Dr. Ala Alwan, former director of WHO Eastern Mediterranean Region and former Iraqi Minister of Health; Dr. Tahmeed Ahmed, executive director of icddr,b, Bangladesh; Dr. Patricia García, former dean of Universidad Peruana Cayetano Heredia and former Minister of Health, Peru; and Dr. Melissa Salm, postdoctoral fellow at the Center for International Security & Cooperation, Stanford University.
The panelists offered their thoughts on how the definition has changed over the last two decades. Salm commented that, “Health is so much more than the absence of disease.” She asked the audience to consider a One Health approach that, “decenters the human in global health as animal, environmental, and human health are all factors to be
The panelists offered their thoughts on how the definition has changed over the last two decades. Salm commented that, “Health is so much more than the absence of disease.” She asked the audience to consider a One Health approach that, “decenters the human in global health as animal, environmental, and human health are all factors to be
considered.” The panelists had diverging definitions when asked what makes something a global health issue. Ahmed and Alwan agreed that the burden should be substantial and transcend boundaries, while García believes global health means sharing cooperative ways of solving problems across countries. Salm added, “Global health is a model that interconnects global entities to respond to emergencies.” The panelists also discussed the potential of artificial intelligence and machine learning to solve global health problems, but emphasized the need for these technologies to be designed by and for local communities.
considered.” The panelists had diverging definitions when asked what makes something a global health issue. Ahmed and Alwan agreed that the burden should be substantial and transcend boundaries, while García believes global health means sharing cooperative ways of solving problems across countries. Salm added, “Global health is a model that interconnects global entities to respond to emergencies.” The panelists also discussed the potential of artificial intelligence and machine learning to solve global health problems, but emphasized the need for these technologies to be designed by and for local communities.
Regarding what changes are needed in the field, Ahmed offered that institutions should move from theoretical to practical, field-based work, and Alwan stressed “I would like to see more implementation science research taking place within ministries of health.” García suggested standing up more regional health agencies, like Africa CDC, to shift global health practice out of high-income countries.
Regarding what changes are needed in the field, Ahmed offered that institutions should move from theoretical to practical, field-based work, and Alwan stressed “I would like to see more implementation science research taking place within ministries of health.” García suggested standing up more regional health agencies, like Africa CDC, to shift global health practice out of high-income countries.
Lichtveld closed the discussion by saying, “We must engage, collaborate, and invest, address asymmetries of power, and ask ourselves if global health is just an organizational model and if emergency preparedness, implementation science, and One Health are essential to global health. We must remember that global health is linked to government and governance, and finally, we must address who will be responsible for global health in the future.”
Lichtveld closed the discussion by saying, “We must engage, collaborate, and invest, address asymmetries of power, and ask ourselves if global health is just an organizational model and if emergency preparedness, implementation science, and One Health are essential to global health. We must remember that global health is linked to government and governance, and finally, we must address who will be responsible for global health in the future.”
The discussion is continuing, and panel members plan to write a paper or series of papers on the topic in the coming months.
The discussion is continuing, and panel members plan to write a paper or series of papers on the topic in the coming months.
and panelists at a CUGH 2023 plenary session (pictured) aimed to define global health in today's context.
Moderators
Fogarty International Center
FOCUS
Moderators and panelists at a CUGH 2023 plenary session (pictured) aimed to define global health in today's context.
Fogarty International Center
55
At the intersection of climate, nutrition & health
 By Mariah Felipe
By Mariah Felipe
Keeping with CUGH's theme of “Global Health at a Crossroads: Equity, Climate Change, and Microbial Threats,” Fogarty and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) organized a session focused on the impact of climate change on nutrition and health. Featuring experts from academia and government, the session aimed to investigate the intersection of global warming, diet, and wellness and their effects on equitable, sustainable, and resilient responses to emerging public health issues.
Dr. William Dietz, director of the Sumner M. Redstone Global Center for Prevention and Wellness at George Washington University’s Milken Institute School of Public Health, opened the discussion by highlighting the “syndemic” of obesity, malnutrition, and climate change, which he defines as three pandemics interacting at biological and biosocial levels having adverse impacts on each other. He noted, “While the U.S. is currently number two in the emission of greenhouse gases globally, the effects are mostly felt in low- and middle-income countries (LMICs). That fact gives the U.S. a special responsibility for reversing this syndemic.”
But the impact can be felt here too. NIH Climate Scholar Dr. Lauren Clay, an associate professor and department chair at the University of Maryland Baltimore County, discussed the effect natural disasters, as a result of climate change, have had on crop yields, health, and nutrition in the U.S. She reasoned, “the U.S. must engage in a global conversation about these issues.”
Diet also plays a crucial role in preventing climate change, and maintaining human and planetary health, according to data from the Global Burden of Disease project highlighted by Dr. Jessica Fanzo. “We are at a crisis moment concerning the food system and climate change,” said the Bloomberg Distinguished Professor of Global Food and Agricultural Policy and Ethics at Johns Hopkins University. Diet is one of the most significant contributors to mortality and morbidity around the world, and our current food systems contribute significantly to greenhouse gases.
Planetary warming and changes to crop yields lead to heat stress and malnutrition, creating a double burden on maternal and child health, per Dr. Kartik Shankar,
professor of pediatrics and nutrition at the University of Colorado School of Medicine. He showcased how increasing global temperatures not only affect access to nutritious foods but can also impact development in the womb, referring to studies in which women who carried their pregnancies through the summer months or in overall higher temperatures tended to have children with lower birth weights. He noted, “Improving nutrition may prevent the effects of heat stress for expectant mothers.”
Interventions—like farm diversification and conservation efforts such as community seed banks—are helpful, but there is still a need for scalability in adopting these practices globally, according to Dr. Beatrice Ekesa. In her talk, Ekesa, a nutrition scientist at Alliance Bioversity International & CIAT in Uganda, focused on the importance of preserving agrobiodiversity to optimize food production, enhance soil health, and reduce the use of fertilizers or pesticides in crop production. She also highlighted the decrease in the diversity of crops over the years. For example, sweet corn had more than 307 varieties at commercial seed houses in 1903; 80 years later the number of varieties had shrunk to just 12.
Dr. Meera Shekar, the global lead for health, nutrition, and population at the World Bank, discussed how her organization addresses these challenges, including supply- and demand-side interventions, analytics, policy dialogues, and investments in various sectors. She suggested that “taxation policies like those we have seen around the world on sugar-sweetened beverages might be a viable option for reducing beef consumption and ultra-processed foods which contribute the most to overall food emissions.”
7 FOCUS ON CUGH - REIMAGINING GLOBAL HEALTH 7 Image courtesy of RAFTI-USA
7
56 Delaware Journal of Public Health - August 2023
Crop diversity has greatly decreased in the last century. Preserving agrobiodiversity helps meet the challenges of climate change and nutrition insecurity.
Reducing the environmental impact of eye surgery
Reducing the environmental impact of eye surgery
The climate crisis may increase the risks for many eye diseases, such as cataract and infections, due to increased UV radiation, drought, weather extremes, and infectious diseases, according to the International Agency for the Prevention of Blindness. If global warming intensifies, it is likely that the number of people living with blindness—currently about 43 million—and the number of those with moderate to severe visual impairment—about 295 million—will rise. Much of this increasing disability will occur in low- and middle-income countries, where populations generally have less access to ophthalmic care to prevent or reverse eye disease.
The climate crisis may increase the risks for many eye diseases, such as cataract and infections, due to increased UV radiation, drought, weather extremes, and infectious diseases, according to the International Agency for the Prevention of Blindness. If global warming intensifies, it is likely that the number of people living with blindness—currently about 43 million—and the number of those with moderate to severe visual impairment—about 295 million—will rise. Much of this increasing disability will occur in low- and middle-income countries, where populations generally have less access to ophthalmic care to prevent or reverse eye disease.
At a recent CUGH session, Dr. David F. Chang, ophthalmologist from the University of California, San Francisco, warned the WHO has declared climate change the single greatest threat to human health. He also pointed out the concerning irony that the health care sector is responsible for 4.4% of all global greenhouse gas emissions, of which 71% arise from the manufacture, use, and disposal of medical supplies. Operating rooms account for a major share of health care’s carbon footprint through the generation and disposal of enormous amounts of surgical waste.
At a recent CUGH session, Dr. David F. Chang, ophthalmologist from the University of California, San Francisco, warned the WHO has declared climate change the single greatest threat to human health. He also pointed out the concerning irony that the health care sector is responsible for 4.4% of all global greenhouse gas emissions, of which 71% arise from the manufacture, use, and disposal of medical supplies. Operating rooms account for a major share of health care’s carbon footprint through the generation and disposal of enormous amounts of surgical waste.
Follow the LMICs
Follow the LMICs
As a specialty, ophthalmology has the highest volume of surgeries in medicine. This prompted Chang to co-found EyeSustain, a global consortium of 40 ophthalmology societies. “We believe there is a pressing need to reduce the environmental impact of cataract and other eye surgeries, which are increasing in volume as our population ages,” Chang said. “Because we have the highest surgical volumes, ophthalmology has a unique opportunity—and an obligation—to make our highest volume procedures more sustainable.”
As a specialty, ophthalmology has the highest volume of surgeries in medicine. This prompted Chang to co-found EyeSustain, a global consortium of 40 ophthalmology societies. “We believe there is a pressing need to reduce the environmental impact of cataract and other eye surgeries, which are increasing in volume as our population ages,” Chang said. “Because we have the highest surgical volumes, ophthalmology has a unique opportunity—and an obligation—to make our highest volume procedures more sustainable.”
Operating room regulations, meant to protect patients, dictate the use of non-reusable supplies, resulting in a large amount of waste.
supplies, resulting in a large amount of waste.

For both guidance and inspiration, Chang turns to southern India’s Aravind Eye Care System. Founded in 1976, Aravind encompasses 14 eye hospitals in Southern India. Collectively, they perform the highest volume of cataract surgery in the world and half of their patients receive care either free of charge or at a heavily subsidized rate.
For both guidance and inspiration, Chang turns to southern India’s Aravind Eye Care System. Founded in 1976, Aravind encompasses 14 eye hospitals in Southern India. Collectively, they perform the highest volume of cataract surgery in the world and half of their patients receive care either free of charge or at a heavily subsidized rate.
Aravind pursues its mission of eliminating needless blindness by providing large-volume, high-quality and affordable care. “If you want to learn how to be more efficient and sustainable, you can look to low- and middle-income countries, because they already are most efficient—they don’t have the luxury of wasting money or resources,” said Chang.
Aravind pursues its mission of eliminating needless blindness by providing large-volume, high-quality and affordable care. “If you want to learn how to be more efficient and sustainable, you can look to low- and middle-income countries, because they already are most efficient—they don’t have the luxury of wasting money or resources,” said Chang.
Evidence-based procedures
To maximize cost effectiveness of care, every Aravind hospital routinely reuses surgical gowns, gloves, irrigation bottles, tubing, metal blades, and both topical and intraocular drugs, Chang noted in a recent editorial published in the Journal of Cataract & Refractive Surgery. Aravind hospitals also simultaneously prepare and operate on multiple patients (none required to wear hospital gowns) within the same operating room.
Evidence-based procedures
To maximize cost effectiveness of care, every Aravind hospital routinely reuses surgical gowns, gloves, irrigation bottles, tubing, metal blades, and both topical and intraocular drugs, Chang noted in a recent editorial published in the Journal of Cataract & Refractive Surgery. Aravind hospitals also simultaneously prepare and operate on multiple patients (none required to wear hospital gowns) within the same operating room.
One study found that carbon emissions generated by one phacoemulsification (a procedure used to remove the natural lens of the eye during cataract surgery) at an Aravind center are approximately 1/20 of those generated by the same procedure in the United Kingdom. Each of Aravind’s practices (other than topical drug reuse) is a forbidden infection control violation in the U.S., noted Chang. Aravind’s postoperative endophthalmitis (POE) rate, then, should be much higher than in the U.S. where most supplies are discarded after single use to prevent infection.
One study found that carbon emissions generated by one phacoemulsification (a procedure used to remove the natural lens of the eye during cataract surgery) at an Aravind center are approximately 1/20 of those generated by the same procedure in the United Kingdom. Each of Aravind’s practices (other than topical drug reuse) is a forbidden infection control violation in the U.S., noted Chang. Aravind’s postoperative endophthalmitis (POE) rate, then, should be much higher than in the U.S. where most supplies are discarded after single use to prevent infection.
“In fact, it is not,” noted Chang. The POE rate for 2 million consecutive Aravind cataract surgeries between 2011 and 2018 was 0.04%. Comparatively, the American Academy of Ophthalmology’s Intelligent Research in Sight (IRIS) registry reported an identical 0.04% POE rate for 8.5 million consecutive cataract surgeries performed in the U.S. during an overlapping period.
“In fact, it is not,” noted Chang. The POE rate for 2 million consecutive Aravind cataract surgeries between 2011 and 2018 was 0.04%. Comparatively, the American Academy of Ophthalmology’s Intelligent Research in Sight (IRIS) registry reported an identical 0.04% POE rate for 8.5 million consecutive cataract surgeries performed in the U.S. during an overlapping period.
Chang explained that cataract surgery is a relatively clean procedure with a low risk for microbial aerosolization and cross-contamination. “The Aravind data suggest that mandating single use of so many supplies and drugs is not necessary but generates a huge amount of needless waste and carbon emissions.”
Chang explained that cataract surgery is a relatively clean procedure with a low risk for microbial aerosolization and cross-contamination. “The Aravind data suggest that mandating single use of so many supplies and drugs is not necessary but generates a huge amount of needless waste and carbon emissions.”
FOCUS ON CUGH - REIMAGINING GLOBAL HEALTH
Photo courtesy of EyeSustain
Operating room regulations, meant to protect patients, dictate the use of non-reusable
FOCUS ON CUGH - REIMAGINING GLOBAL HEALTH
Photo courtesy of EyeSustain
57
Mental health, climate change, equitable collaboration
Mental health, climate change, equitable collaboration
By Susan Scutti
By Susan Scutti
The many traditions of the annual Consortium of Universities for Global Health (CUGH) conference include presenting a rich array of virtual satellite sessions to the public. This year’s agenda encompassed examinations of machine intelligence, road traffic crashes, rising mistrust of public health, cancer research, crisis preparedness, and blindness. Two sessions of note focused on mental health as a noncommunicable disease (NCD) in the context of Caribbean and the way universities can support equity in global health collaborations.
The many traditions of the annual Consortium of Universities for Global Health (CUGH) conference include presenting a rich array of virtual satellite sessions to the public. This year’s agenda encompassed examinations of machine intelligence, road traffic crashes, rising mistrust of public health, cancer research, crisis preparedness, and blindness. Two sessions of note focused on mental health as a noncommunicable disease (NCD) in the context of Caribbean and the way universities can support equity in global health collaborations.
Post-colonial mental health
Though similar in many ways, the 26 islands of the Caribbean diverge in terms of resources; the World Bank classifies Antigua’s economy as high-income, Jamaica’s as upper middle-income, and Haiti’s as lower middle-income. Recent changes, including the COVID-19 pandemic, decriminalization of marijuana, and climate change-related weather events, have fueled a rise in mental health issues across the region. This wellness deficit, which encompasses neurological and substance use disorders, often worsens the outcomes of other NCDs, such as diabetes and cardiovascular disease, warranting urgent attention.
Post-colonial mental health
Though similar in many ways, the 26 islands of the Caribbean diverge in terms of resources; the World Bank classifies Antigua’s economy as high-income, Jamaica’s as upper middle-income, and Haiti’s as lower middle-income. Recent changes, including the COVID-19 pandemic, decriminalization of marijuana, and climate change-related weather events, have fueled a rise in mental health issues across the region. This wellness deficit, which encompasses neurological and substance use disorders, often worsens the outcomes of other NCDs, such as diabetes and cardiovascular disease, warranting urgent attention.
Caribbean researchers addressed these interlinked issues in a session, “Mental Health: A solution for reducing NCDs in the Caribbean,” organized by the American University of Antigua College of Medicine.
Caribbean researchers addressed these interlinked issues in a session, “Mental Health: A solution for reducing NCDs in the Caribbean,” organized by the American University of Antigua College of Medicine.

Their central theme was the rising burden of NCDs (including mental health disorders) faced by the region. Presenters emphasized the necessity of recognizing trauma as a driver of NCDs along with understanding how alcohol, tobacco, and cannabis contribute to preventable chronic disease and disability.
Their central theme was the rising burden of NCDs (including mental health disorders) faced by the region. Presenters emphasized the necessity of recognizing trauma as a driver of NCDs along with understanding how alcohol, tobacco, and cannabis contribute to preventable chronic disease and disability.
Capacity exchange
described how the medical students and surgeons in Rwanda taught her “realities on the ground” and innovations unknown in the U.S. “If I worked in a rural area in the U.S., I could use these methods,” she said.
described how the medical students and surgeons in Rwanda taught her “realities on the ground” and innovations unknown in the U.S. “If I worked in a rural area in the U.S., I could use these methods,” she said.
Equality of funding
Vanderbilt University’s Dr. Quentin Eichbaum would like to see the cake divided more equitably. He identified an issue that frequently troubles global health partnerships: many high-income country collaborators choose to work at only the big name LMIC institutions rather than at lesser-known institutions that might benefit more from partnerships. “There are about 130 new medical schools in Africa at various stages of development… but NIH/ CDC/Fogarty have consistently been risk-averse and preferred to develop partnerships at and fund wellestablished institutions.”
Equality of funding
Vanderbilt University’s Dr. Quentin Eichbaum would like to see the cake divided more equitably. He identified an issue that frequently troubles global health partnerships: many high-income country collaborators choose to work at only the big name LMIC institutions rather than at lesser-known institutions that might benefit more from partnerships. “There are about 130 new medical schools in Africa at various stages of development… but NIH/ CDC/Fogarty have consistently been risk-averse and preferred to develop partnerships at and fund wellestablished institutions.”
Capacity exchange
Seeking to identify administrative and policy changes that would support equity in global health research collaborations, Harvard Medical School organized the satellite session, “Transforming Universities for Equity and Impact in Global Health.” Moderated by Dr. Kathryn Chu of Stellenbosch University, a rousing panel discussion spilled over into the chat and led to a collective reckoning around the concept of equitable collaboration.
Seeking to identify administrative and policy changes that would support equity in global health research collaborations, Harvard Medical School organized the satellite session, “Transforming Universities for Equity and Impact in Global Health.” Moderated by Dr. Kathryn Chu of Stellenbosch University, a rousing panel discussion spilled over into the chat and led to a collective reckoning around the concept of equitable collaboration.
Dr. Dana Thomson of Harvard Medical School questioned the term “capacity building,” noting that it is often assumed to mean a transfer of knowledge from high-resource to lower-resource nations. “This reinforces an inequitable narrative,” she said and suggested “capacity exchange” as a more accurate descriptor of global health partnerships. Dr. Rashi Jhunjhunwala, also at Harvard Medical School,
Dr. Dana Thomson of Harvard Medical School questioned the term “capacity building,” noting that it is often assumed to mean a transfer of knowledge from high-resource to lower-resource nations. “This reinforces an inequitable narrative,” she said and suggested “capacity exchange” as a more accurate descriptor of global health partnerships. Dr. Rashi Jhunjhunwala, also at Harvard Medical School,
Stanford’s Dr. Michele Barry suggested advocating for increased allocation of grant funds for indirect costs to the Global South while also twinning, or pairing, wellfunded partner institutions with less well-known institutions whenever a research grant is awarded. Eichbaum agreed that twinning could help, but added that sharing funds among the institutions (and not just offering “advice”) would be crucial for these strategies to work.
Stanford’s Dr. Michele Barry suggested advocating for increased allocation of grant funds for indirect costs to the Global South while also twinning, or pairing, wellfunded partner institutions with less well-known institutions whenever a research grant is awarded. Eichbaum agreed that twinning could help, but added that sharing funds among the institutions (and not just offering “advice”) would be crucial for these strategies to work.
Summarizing the session, University of Pittsburgh’s Dr. Maureen Lichtveld, a Fogarty board member, shared that, as a member of promotions committees and a peer reviewer, she, herself, has valued or devalued other researchers along hierarchical lines—downgrading the comments of academics based in LMICs (or in lesserknown universities in high income countries) and failing to give proper due to authorship that is neither first nor last. “I’ve been on those committees, so I know that we are the ones who don’t value certain experiences,” she said.
Summarizing the session, University of Pittsburgh’s Dr. Maureen Lichtveld, a Fogarty board member, shared that, as a member of promotions committees and a peer reviewer, she, herself, has valued or devalued other researchers along hierarchical lines—downgrading the comments of academics based in LMICs (or in lesserknown universities in high income countries) and failing to give proper due to authorship that is neither first nor last. “I’ve been on those committees, so I know that we are the ones who don’t value certain experiences,” she said.
9 FOCUS ON CUGH - REIMAGINING GLOBAL HEALTH
9 FOCUS ON CUGH - REIMAGINING GLOBAL HEALTH
Ad campaign from the Healthy Caribbean Coalition. Courtesy of Healthy Caribbean Coalition
58 Delaware Journal of Public Health - August 2023
Ad campaign from the Healthy Caribbean Coalition. Courtesy of Healthy Caribbean Coalition
DIRECTOR’S COLUMN
By Dr. Peter Kilmarx, Acting Director, Fogarty International Center

Promoting diversity, equity, and inclusion beyond borders
The Fogarty International Center is deeply committed to improving health outcomes and reducing health disparities around the world. One way we can achieve this goal is by training individuals from populations who are underrepresented as health researchers.
I’m pleased to share Fogarty’s recent Notice of Special Interest (NOSI) for Administrative Supplements to Fogarty Training Grants to Promote Diversity, Equity, and Inclusion (DEI) which aims to do just that. With these supplements, we intend to support existing research training programs in their efforts to provide a foundation in research design, methods, and analytic techniques to a diverse set of trainees.
For example, members of certain ethnolinguistic and indigenous populations in low- and middle-income countries (LMICs) are often among the most vulnerable, facing significant barriers to accessing high-quality health care and suffering from a disproportionate burden of disease. Members of these and other such marginalized communities are also often underrepresented in the health research workforce, which can limit our understanding of their unique health needs and prevent us from developing interventions to address their specific health challenges. Health research training can play a critical role in addressing these disparities by empowering individuals from underserved populations with the skills and knowledge they need to conduct high-quality research. By training and supporting these researchers, we can help elevate their perspectives so that their experiences are valued, and the health needs of all populations are addressed.
As a Peace Corps volunteer, I learned many proverbs in Tshiluba, one of the regional languages in the Democratic Republic of the Congo. One of my favorites is “Bidi bikengela kulala mu nzubu wa muntu mukuabo bua kumanya mvula udi ulota muaba kayi,” which is to say, “You have to sleep in another person’s house to know where the roof lets the rain in.” It is the members of these marginalized populations who know what the most important health problems are in their communities, and with the right training, are uniquely equipped to find the most effective, locally appropriate, and sustainable solutions.
With the skills and knowledge needed to conduct research provided by these supplements, these individuals will be well placed to help their communities identify and address their own health challenges and not rely solely on outside experts, who often lack contextual knowledge. This can also help build trust, promote understanding between researchers and communities, and address the power imbalances that often exist between researchers from high-income countries and the communities they study.
It is of course up to our grantees and their partners to apply for such funding, as well as to define underrepresented populations in the countries in which they work. It may be members of specific ethnolinguistic groups, socioeconomically disadvantaged populations, underserved rural populations, groups with disabilities, immigrants and displaced populations, or sexual and gender minorities, among others.
We hope that this initiative will lead to tangible improvements in health equity and further build sustainable local capacity for conducting research where it is needed most. Imagine the impact over a generation of helping establish new and diverse research leaders around the world!
We also hope to learn from them new approaches and techniques that may be shared widely to decrease health disparities, including here in the United States.

This initiative is made possible by increased funding for health disparities research in Fogarty’s congressional appropriation for fiscal year 2023. I thank Dr. Flora Katz, Director of our Division of International Training and Research, for her commitment to this issue, and our extramural program officers and grants management staff who will support and administer this initiative in addition to their current workloads.
Health research training is a powerful tool for promoting research and health equity, social justice, and improving health outcomes in LMICs, particularly for individuals from populations who are underrepresented as health researchers. We can only benefit from harnessing the talent, experiences, and perspectives from a more inclusive and diverse global health research workforce in our collective efforts to achieve greater health equity for all. We at Fogarty remain committed to supporting health research training programs around the world, and we look forward to continuing to work with our NIH and global partners.
59
HEALTH Briefs Global PEOPLE
HEALTH Briefs Global PEOPLE
WHO gives lifetime achievement awards
WHO gives lifetime achievement awards
WHO gives lifetime achievement awards
WHO awarded two lifetime achievement awards during the Seventy-sixth World Health Assembly. Professor Jean-Jacques Muyembe-Tamfum of the Democratic Republic of the Congo was recognized for his innovation, leadership and ground-breaking contributions to the management and treatment of diseases such as Ebola virus disease.
WHO awarded two lifetime achievement awards during the Seventy-sixth World Health Assembly. Professor Jean-Jacques Muyembe-Tamfum of the Democratic Republic of the Congo was recognized for his innovation, leadership and ground-breaking contributions to the management and treatment of diseases such as Ebola virus disease.
WHO awarded two lifetime achievement awards during the Seventy-sixth World Health Assembly. Professor Jean-Jacques Muyembe-Tamfum of the Democratic Republic of the Congo was recognized for his innovation, leadership and ground-breaking contributions to the management and treatment of diseases such as Ebola virus disease.



Professor Peter Piot of Belgium was recognized for his extraordinary leadership in the response to the HIV/AIDS epidemic including his vital role in launching major global health initiatives such as UNAIDS, the Global Fund, and others that have improved health outcomes around the world.
Professor Peter Piot of Belgium was recognized for his extraordinary leadership in the response to the HIV/AIDS epidemic including his vital role in launching major global health initiatives such as UNAIDS, the Global Fund, and others that have improved health outcomes around the world.
Professor Peter Piot of Belgium was recognized for his extraordinary leadership in the response to the HIV/AIDS epidemic including his vital role in launching major global health initiatives such as UNAIDS, the Global Fund, and others that have improved health outcomes around the world.



Gairdner honors Belizan
Gairdner honors Belizan
Gairdner honors Belizan
Dr. Jose Belizan was awarded the 2023 Canada Gairdner Global Health Award for the development of innovative, evidence-based and low-cost interventions in maternal and child health. Belizan was co-director of the Fogarty International Clinical Research Fellows site in Argentina.
Dr. Jose Belizan was awarded the 2023 Canada Gairdner Global Health Award for the development of innovative, evidence-based and low-cost interventions in maternal and child health. Belizan was co-director of the Fogarty International Clinical Research Fellows site in Argentina.
Dr. Jose Belizan was awarded the 2023 Canada Gairdner Global Health Award for the development of innovative, evidence-based and low-cost interventions in maternal and child health. Belizan was co-director of the Fogarty International Clinical Research Fellows site in Argentina.
McIff named deputy of HHS Global Affairs
McIff named deputy of HHS Global Affairs
McIff named deputy of HHS Global Affairs
Colin McIff was appointed as Deputy Assistant Secretary of the Office of Global Affairs (OGA), HHS. He previously served as OGA deputy director, director of the Europe office of the FDA, HHS representative to the European Union, and health attaché at the U.S. Mission to the United Nations in Geneva.
Colin McIff was appointed as Deputy Assistant Secretary of the Office of Global Affairs (OGA), HHS. He previously served as OGA deputy director, director of the Europe office of the FDA, HHS representative to the European Union, and health attaché at the U.S. Mission to the United Nations in Geneva.
Colin McIff was appointed as Deputy Assistant Secretary of the Office of Global Affairs (OGA), HHS. He previously served as OGA deputy director, director of the Europe office of the FDA, HHS representative to the European Union, and health attaché at the U.S. Mission to the United Nations in Geneva.



Belkaid to lead Pasteur Institute
Belkaid to lead Pasteur Institute
Belkaid to lead Pasteur Institute






Dr. Yasmine Belkaid has been appointed president of the Institut Pasteur where she received her Ph.D. Scientific director of the NIH Center for Human Immunology, Inflammation, and Autoimmunity, Belkaid is widely recognized for her expertise in the study of immune responses at mucosal surfaces. Her role as president will begin in January 2024.
Dr. Yasmine Belkaid has been appointed president of the Institut Pasteur where she received her Ph.D. Scientific director of the NIH Center for Human Immunology, Inflammation, and Autoimmunity, Belkaid is widely recognized for her expertise in the study of immune responses at mucosal surfaces. Her role as president will begin in January 2024.
Dr. Yasmine Belkaid has been appointed president of the Institut Pasteur where she received her Ph.D. Scientific director of the NIH Center for Human Immunology, Inflammation, and Autoimmunity, Belkaid is widely recognized for her expertise in the study of immune responses at mucosal surfaces. Her role as president will begin in January 2024.
NHGRI releases human "pangenome"
NHGRI releases human "pangenome"
NHGRI releases human "pangenome"
Researchers from the NHGRI-funded Human Pangenome Reference Consortium released a new collection of reference human genome sequences that captures substantially more diversity from different human populations than what was previously available. The new “pangenome" reference aims to include the genome sequences of 350 people by mid-2024.
Researchers from the NHGRI-funded Human Pangenome Reference Consortium released a new collection of reference human genome sequences that captures substantially more diversity from different human populations than what was previously available. The new “pangenome" reference aims to include the genome sequences of 350 people by mid-2024.
Researchers from the NHGRI-funded Human Pangenome Reference Consortium released a new collection of reference human genome sequences that captures substantially more diversity from different human populations than what was previously available. The new “pangenome" reference aims to include the genome sequences of 350 people by mid-2024.
USAID to support climate resilience
USAID to support climate resilience
USAID to support climate resilience
USAID announced $1M in assistance to cities across Latin America and the Caribbean to help build resilience to the impacts of climate change during the inaugural Cities Summit of the Americas. Funding will support the development of city-level plans that foster integration of migrants, reduce disaster risk, and strengthen climate resilience across the region.
USAID announced $1M in assistance to cities across Latin America and the Caribbean to help build resilience to the impacts of climate change during the inaugural Cities Summit of the Americas. Funding will support the development of city-level plans that foster integration of migrants, reduce disaster risk, and strengthen climate resilience across the region.
USAID announced $1M in assistance to cities across Latin America and the Caribbean to help build resilience to the impacts of climate change during the inaugural Cities Summit of the Americas. Funding will support the development of city-level plans that foster integration of migrants, reduce disaster risk, and strengthen climate resilience across the region.
WHO launches health inequality data repository
WHO launches health inequality data repository
WHO launches health inequality data repository
Hailing it as the “largest global collection of disaggregated data about health and determinants of health," the WHO released its Health Inequality Data Repository in April. The repository aims to make datasets from a variety of publicly available data sources more readily available for analysis.
Hailing it as the “largest global collection of disaggregated data about health and determinants of health," the WHO released its Health Inequality Data Repository in April. The repository aims to make datasets from a variety of publicly available data sources more readily available for analysis.
Hailing it as the “largest global collection of disaggregated data about health and determinants of health," the WHO released its Health Inequality Data Repository in April. The repository aims to make datasets from a variety of publicly available data sources more readily available for analysis.
G-FINDER reviews devices to treat postpartum hemorrhage
G-FINDER reviews devices to treat postpartum hemorrhage
G-FINDER reviews devices to treat postpartum hemorrhage
The report provides a snapshot of the R&D landscape for devices in use or investigated for treatment of postpartum hemorrhage (PPH) . PPH is the leading cause of maternal mortality worldwide according to WHO. The report aims to shed light on possible low-tech approaches to reducing deaths due to PPH.
The report provides a snapshot of the R&D landscape for devices in use or investigated for treatment of postpartum hemorrhage (PPH) . PPH is the leading cause of maternal mortality worldwide according to WHO. The report aims to shed light on possible low-tech approaches to reducing deaths due to PPH.
The report provides a snapshot of the R&D landscape for devices in use or investigated for treatment of postpartum hemorrhage (PPH) . PPH is the leading cause of maternal mortality worldwide according to WHO. The report aims to shed light on possible low-tech approaches to reducing deaths due to PPH.
Academies publish proceedings on implementation science
Academies publish proceedings on implementation science
Academies publish proceedings on implementation science
The National Academies Global Forum on Innovation in Health Professional Education published the proceedings of their 2022 workshop series on the use and application of implementation science in health professions education. Workshops centered on the potential use of implementation science in the classroom and clinical practice.
The National Academies Global Forum on Innovation in Health Professional Education published the proceedings of their 2022 workshop series on the use and application of implementation science in health professions education. Workshops centered on the potential use of implementation science in the classroom and clinical practice.
The National Academies Global Forum on Innovation in Health Professional Education published the proceedings of their 2022 workshop series on the use and application of implementation science in health professions education. Workshops centered on the potential use of implementation science in the classroom and clinical practice.
HEALTH Briefs Global PEOPLE 11
11
11
60 Delaware Journal of Public Health - August 2023
Funding Opportunity Announcement Deadline
Chronic, Noncommunicable Diseases and Disorders Research Training
Global Infectious Diseases (GID)
Details
Aug 3, 2023
Fogarty HIV Research Training http://bit.ly/NIHGlobalHIV Aug 22, 2023
G11 Clinical Trials Not Allowed D71 Clinical Trials Not Allowed
For more information, visit www.fic.nih.gov/funding
Global Health Matters
May/June 2023
Volume 22, No. 3 ISSN: 1938-5935
Fogarty International Center National Institutes of Health Department of Health and Human Services
Communications director: Andrey Kuzmichev Andrey.Kuzmichev@nih.gov
Managing editor: Judy Coan-Stevens Judith.Coan-Stevens@nih.gov
Writer/editor: Mariah Felipe Mariah.Felipe@nih.gov
Writer/editor: Susan Scutti Susan.Scutti@nih.gov
Digital analyst: Merrijoy Vicente Merrijoy.Vicente@nih.gov
Designer: Carla Conway
All text produced in Global Health Matters is in the public domain and may be reprinted. Please credit Fogarty International Center. Images must be cleared for use with the individual source, as indicated.
Scan and read this issue online

Journal highlights mental health of children & teens in sub-Saharan Africa

High rates of poverty, violence, and inadequate health systems escalate rates of mental illness in sub-Saharan Africa (SSA). A special supplement in the Journal of Adolescent Health addresses the special behavioral health needs of children and teens in this region.
The publication presents research spanning the disciplines of social work, medicine, public health, community health, and family development.
“Serious consideration needs to be given to context-specific influences within SSA, such as mental health-related stigma, skepticism of professional responses, the large number of children and adolescents affected by HIV/AIDS, and the lack of family economic opportunities,” said Dr. Fred Ssewamala of the Brown School, Washington University in St. Louis.
He is a founding director of the International Center for Child Health and Development (ICHAD) and co-director of SMART
Africa Centers. The two organizations hosted the 5th Annual Conference on Child Behavioral Health in Sub-Saharan Africa and issued a call for abstracts focusing on advances in SSA behavioral health. Manuscripts developed from some of these abstracts appear in the supplement.
SUBSCRIBE: www.fic.nih.gov/subscribe
“South to South Collaboration to Strengthen Child and Adolescent Mental Health in Sub-Saharan Africa” was edited by Manasi Jumar of Aga Khan University. The National Institute of Mental Health supported its publication.
MAY/JUNE 2023
Photo courtesy of Allison DiVincenzo, USAID
A teen stays in a women's shelter in Zimbabwe.
http://bit.ly/NCDtrain Jul 13, 2023
http://bit.ly/GID-FIC
61
Evaluation & Treatment of Psychological Effects of Stroke
Nancy Devereux Ph.D.
Clinical Neuropsychologist, ChristianaCare; Delaware Stroke System of Care Subcommittee
Ashley M. Berns Psy.D. ChristianaCare Behavioral Health Department
ABSTRACT
Strokes are a common medical condition in the United States, including in Delaware. An under-recognized effect of stroke is the impact on mood that often occurs. Many individuals develop depression, anxiety, PTSD, and other psychological sequelae. These disorders can significantly affect their lives and their relationships. The emotional effects of stroke pose a public health problem for our residents, leading to devastating decreases in the quality of life for the patient and the family. These challenges negatively impact the community due to the associated healthcare and economic burdens. The population of the State of Delaware is growing, and the proportion of senior residents, who are also at greater risk for strokes, is also increasing. Strokes will remain an ongoing important clinical concern for our healthcare providers. Emotional changes after a stroke will occur in many Delaware residents who suffer a stroke. The emotional sequelae of stroke are under-treated. It is critical for healthcare professionals to be trained to recognize, assess, and treat the psychological disorders that can result from having a stroke. This article provides an overview of the major psychological effects of stroke, recommended assessment tools, promising treatment trends, and directions for further research. Improving our ability to detect and treat these difficult emotional challenges can facilitate effective treatment and prevention strategies and increase quality of life for stroke survivors, their loved ones, and their communities.
INTRODUCTION
Strokes are unfortunately common across the world. Approximately 12.2 million new strokes occur globally per year.1 In the United States, an estimated 795,000 people suffer a stroke annually.2 In the state of Delaware, 3,139 strokes were recorded in 2022.3 Delaware’s population was estimated at 1,018,392 in mid20224; this suggests that the state’s per capita rate of strokes was about 0.31%.
Survivors of stroke face enormous health, emotional, social, and economic impacts. These effects are experienced at the personal, family, and community levels. Significant complications of stroke include the psychological ramifications that often develop. Post-stroke mood disorders are prevalent yet tend to be underrecognized and under-treated. This clinical challenge was brought to the public’s eye when earlier this year a U.S. senator from our neighboring state of Pennsylvania, John Fetterman, sought hospitalization for his post-stroke depression. He also had a prior history of depression.
Mood disorders apart from stroke are also common around the globe. Approximately 280 million people worldwide live with depression.5 In the United States, it is estimated that 21 million adults aged 18 or older have experienced depression, which is about 8.4% of the adult population.6 One study indicated that, according to standard diagnostic criteria, the twelve-month and lifetime prevalence of major depressive disorder are 10.4% and 20.6% respectively.7
Not surprisingly, stroke is one of the most disabling medical conditions in the US.8 Marked changes in functional and psychosocial functioning are not only experienced by patients
with stroke. Psychiatric disorders can lead to disabling conditions as well. Depression is the leading cause of disability in the United States.9 When stroke and mood disorders are co-occurring, they often generate significant personal and public health consequences. Numerous studies over the past few decades have indicated that post-stroke psychological sequelae can be varied as well as pervasive.10,11 Psychological effects of stroke include depression, anxiety, post-traumatic stress disorder (PTSD), mania, psychosis, irritability, and apathy, among other emotional and behavioral conditions.12 This review will focus on the first three more commonly observed post-stroke psychological sequelae.
POST STROKE DEPRESSION
The most thoroughly researched emotional issue following stroke is depression (PSD). A large body of studies over several decades indicates that roughly 1/3 of individuals sustaining a stroke develop PSD within a year to five years post-onset.13 These individuals have higher rates of healthcare utilization, poorer functional outcomes, reduced quality of life (QOL), and higher mortality.14,15 The depression these patients suffer is not simply due to having a serious medical condition; for example, when compared with patients suffering myocardial infarctions, those with PSD experience higher rates of mood disorders, particularly depression.16,17 While the one-third prevalence rate for PSD is well-supported across studies, some studies have reported lower rates ranging from 15.8% to 21%, depending on setting and time since stroke.18,19 Higher rates have also been reported, and the cumulative incidence of PSD may be as high as 55%.20 The varying rates of depression after stroke are due to combined factors, mostly related to methodology. For example, there is a
62 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.011
lack of standardization of assessment instruments, leading to inconsistent criteria and cut-off scores. Subject inclusion and exclusion criteria are also variable such that “minor depression” and depressive adjustment disorders may or may not be included in investigations of stroke patients with depression, and aphasics and patients with hemorrhagic strokes are often excluded. Time points of assessments relative to stroke onset vary as well. Additionally, geographic region influences the selection and assessment processes. These are only a sampling of the factors that contribute to the variability in the incidence and prevalence of PSD reported across studies. Despite these limitations, it is evident that depression is more common after stroke than its incidence in the general population.10 Understanding the risk factors may assist in optimizing clinical assessment, honing treatments, and developing prevention strategies.
RISK FACTORS
Post-stroke depression is a multifactorial condition.21 There are combined psychological, social, and biological factors that play a role in its manifestation.22 Identification of risk factors is an important area of study for clinical work. The research heterogeneity noted earlier for diagnostic considerations applies to our understanding of risk factors for PSD as well. The variations in research design lead to issues concerning methodology, selection criteria, population setting, geographic location, assessment tools, cut-off scores, time since stroke, etcetera. These irregularities cause difficulty in identifying a clear and consistent set of predictors of PSD across studies. Despite this ambiguity, there are some PSD predictors that warrant comment and further study. These risk factors include (though are not limited to) the following:
Genetic
Studies suggest that there are many genes associated with poststroke depression.21,23,24 These genes include the serotonin transporter gene (SERT) polymorphisms, 5-HTTLPR and STin2 VNTR.21 Apolipoprotein E (ApoE) and methylenetetrahydrofolate reductase (MTHFR) appear to be associated with a higher risk of major depressive disorder following a stroke, and research continues into the identification of genetic contributions to risk for post-stroke depression.
Age
A systematic review, which included 23 studies and 18,374 participants, found that most studies concluded that older age was not associated with an increased risk of depression following a stroke.21 One review indicated that age of stroke at less than 70 years was predictive of PSD, but limited sample size was a drawback.25 Given the mixed research findings, age remains an ambiguous risk factor.
Sex
Research across the decades has yielded mixed results in relation to gender and susceptibility for post-stroke depression.21 A large body of evidence had suggested that females were more likely to develop depression post-stroke than males.16,25 There are also some research findings casting doubt that a specific gender increases the risk of depression following a stroke.22,26
Stroke Severity
A number of studies have demonstrated that the severity of stroke is positively correlated with depression.21,27 However, a
recent review indicated that stroke severity was not predictive of PSD, while level of physical disability was predictive during the first-year post-stroke.28 These two constructs may be conflated in some cases, depending upon definition and assessment tools employed in the study samples. Stroke severity therefore may be a consideration for PSD, depending upon its definition and how it is measured.
Lesion Location
Research has demonstrated that the distance between the brain lesion and the frontal lobe plays an essential role in determining the severity of post-stroke depression.21 More specifically, comparisons between left prefrontal-subcortical lesions (i.e., lesion volume & location) versus right hemisphere have demonstrated that individuals with left hemisphere lesions have a higher incidence and severity of post-stroke depression. Numerous studies have questioned this trend. For example, Robinson and Jorge12 reviewed meta-analyses which did not confirm a strong association between lesion location and subsequent depression. They concluded that there may be an association of PSD with left frontal or basal ganglia lesions within two months of an initial clinical stroke. Findings from a separate review showed some support for this observation, while also indicating that both frontal and subcortical lesions regardless of laterality may be somewhat predictive of PSD.29 At this time, the relationship between lesion location and PSD is not fully understood and may be mediated by other factors.
Aphasia
Depression after stroke may be more likely when a patient has aphasia as compared to patients without language impairments.19 A study of adults with aphasia in an acute care setting indicated that the aphasic patients were seven times more likely to suffer PSD than non-aphasic patients.30
Other Factors
Research suggests that marital status, years of education, history of prior stroke and/or history of myocardial infarction, recent life stressors, poverty, and lack of social supports are associated with a higher incidence of depression following a stroke.18,21,31
ASSESSMENT
The assessment of PSD across sites and studies is highly variable in terms of methods, instruments, cut-off scores, definitions of depression and types of depression, settings, and time points of assessment. For example, brief screenings may be employed, usually administered by a clinician; a lengthier structured interview adhering to DSM-5 Diagnostic and Statistical Manual of Mental Disorders32 criteria can be conducted by a clinician; or a range of approaches in between these methods might be used for depression assessment. The methods include self-report inventories or checklists, mood scales, structured interviews, and clinician or collateral observer ratings.
The studies reviewed in the literature tend to use the following validated instruments: Hospital Anxiety and Depression Scale (HADS);33 Center for Epidemiologic Studies of Depression Scale (CESD);34 Hamilton Depression Rating Scale (HAMD or HDRS);35 Patient Health Questionnaire-9 (PHQ-9);36 Beck Depression Inventory (BDI);37 and Geriatric Depression Scale (GDS).38 The instruments vary in administration time requirements and staff involvement; therefore, practicality and
63
efficiency needs may dictate instrument selection on a busy acute inpatient or rehabilitation unit.
A few reviews of assessment instruments (Table 1) employed with stroke survivors indicate that several types of methods may be useful. Clinician-administered structured clinical interviews and screening scales for depression showed acceptable or better results for all validation measures when used to screen for psychiatric disorders in patients with stroke in a review from 2016.39 Another review suggested that the CES-D, the HDRS and the PHQ-9 may be the best options for adequate sensitivity and specificity.40 Other studies have indicated that despite limitations, the Patient Health Questionnaire-2 (PHQ-2) may be practical for screening due to minimal time and staff demands and acceptable sensitivity.41–43 The authors agree that ideally the instruments should not be used in isolation. A follow-up evaluation utilizing more detailed assessment is recommended, such as following a positive PHQ-2 with PHQ-9, other more focused clinical instruments, and/or direct interview.
There is a potential confound with most of these instruments, in that some of the physiological symptoms of depression overlap with those of stroke. For example, sleep quality, energy level, and appetite are often diminished in hospital patients independent of presence of mood disorder. Yet these symptoms are often altered in depression and are typically included in surveying depression. To minimize the confound, and for practical clinical goals as indicated earlier, the PHQ-2 may be preferable for depression screening purposes in hospital settings.
Many of the studies addressing screening and diagnosis of poststroke depression excluded patients with aphasia. Assessment of depression in these patients can be particularly challenging. Communicative disorders can impact comprehension, not just expression. Reading, writing, spelling, and gesture can be compromised. Validity and reliability of the instruments may be tenuous when used with aphasic patients. The Visual Analogue Mood Scale (VAMS)44 has been utilized to help skirt the communication issue. Its utility may be questionable in some cases. There are concerns that it has not been found to be consistently reliable,45 while other researchers find it to be of value in assessing individuals with aphasia.46
OTHER PSYCHOLOGICAL SEQUELAE OF STROKE
In addition to depression, there are other noteworthy psychological sequelae of stroke. Though less common and less studied, these emotional effects pose potential burdens to patients, families, and the community. Anxiety and PTSD are two of the emotional consequences that are most often observed after depression in patients with strokes.
Anxiety is relatively common following a stroke. In the general population, 19.1% are estimated to have anxiety.47 After stroke, it is estimated that 20-25% of patients develop anxiety.48–50 Anxiety disorders include specific phobias, generalized anxiety disorder (GAD), panic disorder, agoraphobia, and social anxiety disorder. An adjustment disorder with anxiety may also account for the observed symptoms. Anxiety due to another medical condition (other than stroke) and substance use-induced anxiety are typically ruled out and not included in populations under study in these investigations. Post-stroke anxiety (PSA) may
tend to present as specific phobia with or without associated GAD.51 PSA is closely associated with PSD and tends to endure for longer periods when the two conditions co-occur.52,53 Prestroke depression, stroke severity, early anxiety, and dementia or cognitive impairment after stroke appear to be predictive of post-stroke anxiety.54 PSA is typically assessed by the GAD-7;55 the Beck Anxiety Inventory (BAI);56 HADS;33 and the Hamilton Anxiety Rating Scale (HAM-A).57 These instruments have not been validated for stroke populations despite their use clinically and in research with this patient group.
Post-traumatic stress disorder (PTSD) has been observed in some patients following stroke. Suffering a stroke can be perceived as a disruptive and marked traumatic life event.58 Prevalence estimates vary, generally from 10% to 31%, depending upon assessment method employed and other factors.59 One study reported that 1 in 4 stroke survivors endorsed elevated symptoms of PTSD within the first year.60 Of note, PTSD was removed from the Anxiety Disorders category in 2013 in the 5th edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders and placed in the “Trauma and Stressor-related Disorders” section.61 Post-stroke PTSD (PSPTSD) has been associated with nonadherence to medications62; a heightened degree of disability;63,64 and a higher frequency of right cerebral and brainstem lesions.65 Risk factors were not clearly specified, though there may be a greater tendency for PSPTSD to occur in women and at younger ages.58,63 Social support may confer protective resilience against development of PTSD.63 Instruments used to assess PS-PTSD include the Impact of Events Scale (IES-R);66 Primary Care-PTSD Screen (PC-PTSD);67 PCL/ PCL-5;68,69 and clinical interview utilizing DSM-5 criteria.
Depression DSM-5, HADS, CESD, HAMD/HDRS, PHQ-9, BDI Anxiety DSM-5, HADS, BAI, HAM-A PTSD DSM-5, IES-R, PCL/PCL-5
PATHOPHYSIOLOGY
The pathophysiology of post-stroke mood disorders is posited to be multi-factorial. Proposed mechanisms have been discussed in the literature for post-stroke depression more so than for other psychological sequelae. The underlying mechanisms appear to involve decreased levels of monoamines, abnormal neurotrophic response, inflammatory processes, and dysfunctional regulation of hypothalamic-pituitary-adrenal axis and glutamate-mediated excitotoxicity.70 Genetic factors may also interact with the pathophysiological processes.
PREVENTION OF POST STROKE MOOD DISORDERS
There are suggestions that multimodal therapies combined with antidepressants may mitigate against development of PSD.21,71 Studies have been mixed in terms of identifying any specific best practice primarily due to heterogeneity of the designs, instruments, time courses and populations. There is a lack of robust evidence to support the use of specific strategies to prevent PSA and PSD.72 There may be a role for developing more personalized strategies incorporating integrative interventions as improved studies are conducted.71 As mentioned earlier, social support may be a protective factor in guarding against PTSD onset.63
64 Delaware Journal of Public Health - August 2023
Table 1. Post-Stroke Psychological Assessment Tools
TREATMENT
Many individuals surviving stroke are insufficiently or ineffectively treated for psychological effects.73 Studies indicate that post-stroke depression may respond to a variety of treatments.74,75 Treatments of PSA and PS-PTSD are less well studied thus far.
Pharmacologic interventions
The bulk of research dedicated to treating mood disturbance after stroke focuses on pharmacotherapies. Frank et al.70 reviewed numerous studies addressing the effects of various antidepressants on PSD. They found that selective serotonin re-uptake inhibitors (SSRIs), selective norepinephrine re-uptake inhibitors (SNRIs), bupropion, and tricyclic antidepressants (TCAs) were effective in reducing depression scores compared with placebo or “treatment as usual.” Time course in some of the studies was associated with differential effectiveness of medication. The use of SSRI’s for treatment of PSD may improve recovery through neuroprotective mechanisms and taming of inflammation, among other actions.70
It is well-known that not all depressed patients respond to pharmacological treatments.76 Also, despite possible therapeutic response, in some cases the side effects are not well-tolerated. For example, in the studies reviewed by Frank et al.,70 both SSRIs and SNRIs were often found to produce uncomfortable physiological symptoms such as insomnia and sexual dysfunction. The risk of intracerebral bleeding as well as gastrointestinal bleeding appears to be increased as well.77,78
TCAs and Monoamine oxidase-inhibitors (MAOIs) are considered less preferred for pharmacologic treatment due to side effects such as cardiac symptoms and preferential responsivity.70
In general, studies have suggested that antidepressants may improve mood, but the evidence is mixed regarding whether antidepressants significantly facilitate participation in rehabilitation and improvement in activities of daily living (ADLs).79 Not all post-stroke patients respond well to medications.21 There is also no consensus as to the optimal pharmacologic agent, dosage, or timing of administration. For patients with PSA, a Cochrane review indicated a dearth of highquality evidence to guide medication regimens.80
The limitations posed by pharmaceuticals suggest an important role for non-pharmacologic treatments. A variety of interventions have been investigated.
Non-pharmacologic treatments
Cognitive-behavioral therapy (CBT)
Psychotherapeutic interventions, particularly CBT, have been studied in the PSD population. CBT is a psychotherapeutic approach to help individuals learn how to identify and change maladaptive thought patterns that negatively influence their behavior and emotions. This therapeutic technique, whether delivered alone or in conjunction with antidepressant medication, or in group formats, appears to decrease depression as well as anxiety symptoms that can develop after stroke.81,82 However, the evidence for CBT as a treatment for PSD may be inconclusive due to an array of qualitative and quantitative limitations inherent in the studies. Wang and colleagues82 suggest the usefulness of high quality RCTs to address this potentially beneficial treatment.
Related to CBT are treatments that appear potentially beneficial though not yet well studied. These include problem-solving oriented therapies and motivational interviewing.83,84 Observed results have been promising, but limited sample sizes and small effect sizes are problematic for broader application until better designed studies are undertaken.
Neuromodulation
Non-invasive brain stimulation is a relatively recent treatment modality that may improve mood. Neuromodulation techniques such as repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS) have recently been used to treat depression in patients without neurological disorders with beneficial outcomes.85 Recent studies with stroke patients have reportedly demonstrated positive effects.70,86 Further research in this area seems warranted.
Non-traditional therapies
Mind-body therapies, such as meditation, yoga, and tai chi, may be promising for offering relief from emotional suffering after stroke. A review of mind-body interventions suggested a trend toward beneficial psychological outcome but was not conclusive, possibly in part due to design limitations and decreased power of the studies.73 Zou and colleagues87 concluded from their analysis that yoga and tai chi are effective as “add-on” treatments to improve depression, ADLs, and mobility. Most of the studies they reviewed were conducted in China. Chan and colleagues88 found that both yoga and exercise were significantly associated with a reduction in depression symptoms over time; however, no remarkable group differences emerged. Both exercise and yoga have been associated with positive mood and possible treatment of depression in individuals without stroke.89,90 Further study of these interventions for patients with PSD and PSA may be worthwhile.
Other non-pharmacological therapies recently under study suggest positive trends, though more rigorous design and replications are needed.83,86 These interventions include life review and problem-solving therapy, music therapy, and robotassisted neurorehabilitation.
SUMMARY
The psychological effects of stroke such as depression, anxiety and post-traumatic stress disorder are associated with decreased quality of life in many domains, which often impact interpersonal relationships and participation in the community. PSD is one of the more common and better studied complications that can have devastating consequences for the survivor, family, and other interpersonal relationships. PSD is also associated with increased risk of stroke recurrence and mortality. This unfortunate complication of stroke has implications for Delaware residents. The population of Delaware is growing.91,92 Delaware’s proportion of senior residents is also increasing.93 The incidence of strokes in our state is likely to increase, with concomitant effects on emotional adjustment. Psychological sequelae of stroke such as PSD are treatable and perhaps in the not-too-distant future, also preventable. Despite the promising trends in assessment and therapies, the efforts to identify and treat emotionally afflicted patients following stroke are suboptimal across the nation.
65
Ideally, all patients with stroke should be screened for potential post-stroke depression as feasible. Screening at multiple time points over the course of a patient’s recovery appears to be practical.94 Following initial screening, re-assessment at multiple specified time points across the continuum of care (e.g., acute hospital care, rehabilitation transfer, discharge to subacute facility or home) and at follow-up physician and outpatient rehabilitation therapy visits is helpful in identifying and treating patients with psychological sequelae. The use of the PHQ-2 and PHQ-9 for this population appears to be supported in the literature. Clinician follow-up with a more detailed clinical interview for those with positive mood screens can be arranged by a stroke care team. In the State of Delaware, many of the hospitals and clinics have behavioral health professionals available who can assist with emotional adjustment or can link patients to providers in the community. Several of the hospitals also offer virtual or in-person support groups for stroke survivors and their caregivers. Ongoing research addressing post-stroke emotional sequelae is critical to optimizing the care that we clinicians provide to our patients who may be suffering from the psychological effects of strokes. It is anticipated that the findings from well-designed studies will help with prevention of these emotional disorders in addition to refining effective treatments. These developments are anticipated to benefit Delaware residents seeking care for the challenging effects of cerebrovascular disorders.
Dr. Devereux may be contacted at nancy.devereux@christianacare.org
REFERENCES
1. Institute for Health Metrics and Evaluation. (2019). 2019 global burden of disease
http://ghdx.healthdata.org/gbd-results-tool
2. Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Alonso, A., Beaton, A. Z., Bittencourt, M. S., . . . Martin, S. S. (2022, September 6). heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation, 145(8), e141–e141. https://doi.org/10.1161/CIR.0000000000001052
3. Delaware Division of Public Health. (2023). Division of Public Health, United States Census Bureau, 2023. https://www.dhss.delaware.gov/dhss/dph/hp/healthstats.html
4 United States Census Bureau. (2022). Quick facts, Delaware https://www.census.gov/quickfacts/fact/table/DE/PST045222
5. World Health Organization. (2023, March 31). Depressive disorder. https://www.who.int/news-room/fact-sheets/detail/depression
6 National Institute of Mental Health. (2021). Statistics, major depression https://www.nimh.nih.gov/health/statistics/major-depression
7. Hasin, D. S., Sarvet, A. L., Meyers, J. L., Saha, T. D., Ruan, W. J., Stohl, M., & Grant, B. F. (2018, April 1). Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry, 75(4), 336–346
https://doi.org/10.1001/jamapsychiatry.2017.4602
8. Centers for Disease Control and Prevention. (2023). Stroke facts.https://www.cdc.gov/stroke/facts.htm
9 Centers for Disease Control and Prevention. (2023). Genomics and precision health
https://www.cdc.gov/genomics/resources/diseases/mental.htm
10. Hackett, M. L., Köhler, S., O’Brien, J. T., & Mead, G. E. (2014, May). Neuropsychiatric outcomes of stroke. Lancet Neurol, 13(5), 525–534
https://doi.org/10.1016/S1474-4422(14)70016-X
11 Zhang, S., Xu, M., Liu, Z.-J., Feng, J., & Ma, Y. (2020, June 19). Neuropsychiatric issues after stroke: Clinical significance and therapeutic implications. World Journal of Psychiatry, 10(6), 125–138. https://doi.org/10.5498/wjp.v10.i6.125
12 Robinson, R. G., & Jorge, R. E. (2016, March 1). Post-stroke depression: A review. The American Journal of Psychiatry, 173(3), 221–231 https://doi.org/10.1176/appi.ajp.2015.15030363
13 Hackett, M. L., & Pickles, K. (2014, December). Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke, 9(8), 1017–1025. https://doi.org/10.1111/ijs.12357
14 Towfighi, A., Ovbiagele, B., El Husseini, N., Hackett, M. L., Jorge, R. E., Kissela, B. M., …, & Williams, L. S. (2017). Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke (1970), 48(2), e30–e43.
https://doi.org/10.1161/STR.0000000000000113
15. Kutlubaev, M. A., & Hackett, M. L. (2014, December). Part II: predictors of depression after stroke and impact of depression on stroke outcome: an updated systematic review of observational studies. Int J Stroke, 9(8), 1026–1036
https://doi.org/10.1111/ijs.12356
16 Mayman, N. A., Tuhrim, S., Jette, N., Dhamoon, M. S., & Stein, L. K. (2021, September). Sex differences in post-stroke depression in the elderly. J Stroke Cerebrovasc Dis, 30(9), 105948–105948.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105948
17 Skajaa, N., Adelborg, K., Horváth-Puhó, E., Rothman, K. J., Henderson, V. W., Thygesen, L. C., & Sørensen, H. T. (2022). Stroke and risk of mental disorders compared with matched general population and myocardial infarction comparators. Stroke (1970), 53(7), 2287–2298.
https://doi.org/10.1161/STROKEAHA.121.037740
18 Chaudhary, D., Friedenberg, I., Sharma, V., Sharma, P., Abedi, V., Zand, R., & Li, J. (2022). Predictors of post-stroke depression: a retrospective cohort study. Brain Sciences, 12(8), 993–. https://doi.org/10.3390/brainsci12080993
19 Mitchell, A. J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., & Meader, N. (2017, July). Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. General Hospital Psychiatry, 47, 48–60
https://doi.org/10.1016/j.genhosppsych.2017.04.001
20. Ayerbe, L., Ayis, S., Wolfe, C. D. A., & Rudd, A. G. (2013, January). Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. Br J Psychiatry, 202(1), 14–21
https://doi.org/10.1192/bjp.bp.111.107664
21 Guo, J., Wang, J., Sun, W., & Liu, X. (2022, March). The advances of post-stroke depression: 2021 update. Journal of Neurology, 269(3), 1236–1249
https://doi.org/10.1007/s00415-021-10597-4
22. De Ryck, A., Brouns, R., Geurden, M., Elseviers, M., De Deyn, P. P., & Engelborghs, S. (2014, September). Risk factors for poststroke depression: Identification of inconsistencies based on a systematic review. Journal of Geriatric Psychiatry and Neurology, 27(3), 147–158.
https://doi.org/10.1177/0891988714527514
66 Delaware Journal of Public Health - August 2023
23 Han, K., Lee, J., Meyer, T. J., Wang, J., Sen, S. K., Srikanta, D., Batzer, M. A. (2007, October). Alu recombination-mediated structural deletions in the chimpanzee genome. PLOS Genetics, 3(10), e184–e194.
https://doi.org/10.1371/journal.pgen.0030184
24 Hou, Z., Liu, X., Jiang, W., Hou, Z., Yin, Y., Xie, C., Yuan, Y. (2021, July 9). Effect of NEUROG3 polymorphism rs144643855 on regional spontaneous brain activity in major depressive disorder. Behavioural Brain Research, 409, 113310–113310 https://doi.org/10.1016/j.bbr.2021.113310
25 Shi, Y., Yang, D., Zeng, Y., & Wu, W. (2017, July 11). Risk factors for post-stroke depression: A meta-analysis. Frontiers in Aging Neuroscience, 9, 218–218. https://doi.org/10.3389/fnagi.2017.00218
26 Volz, M., Ladwig, S., & Werheid, K. (2021, January). Gender differences in post-stroke depression: A longitudinal analysis of prevalence, persistence and predictive value of known risk factors. Neuropsychological Rehabilitation, 31(1), 1–17. https://doi.org/10.1080/09602011.2019.1648301
27. Pan, A., Sun, Q., Okereke, O. I., Rexrode, K. M., & Hu, F. B. (2011, September 21). Depression and risk of stroke morbidity and mortality: A meta-analysis and systematic review. JAMA, 306(11), 1241–1249 https://doi.org/10.1001/jama.2011.1282
28. Ladwig, S., Werheid, K., Südmeyer, M., & Volz, M. (2023, February 13). Predictors of post-stroke depression: Validation of established risk factors and introduction of a dynamic perspective in two longitudinal studies. Frontiers in Psychiatry, 14, 1093918–1093918
https://doi.org/10.3389/fpsyt.2023.1093918
29. Wijeratne, T. & Sales, C. (2021). Understanding why poststroke depression may be the norm rather than the exception: the anatomical and neuroinflammatory correlates of poststroke depression. Journal of Clinical Medicine, 10(8), 1674–. https://doi.org/10.3390/jcm10081674
30 Zanella, C., Laures-Gore, J., Dotson, V. M., & Belagaje, S. R. (2023, July). Incidence of post-stroke depression symptoms and potential risk factors in adults with aphasia in a comprehensive stroke center. Topics in Stroke Rehabilitation, 30(5), 448–458. https://doi.org/10.1080/10749357.2022.2070363
31 Redmond, C., Bushnell, C., Duncan, P., D’Agostino, R., Jr., Ambrosius, W. T., Bishop, L., El Husseini, N. (2022, April). Association of in-hospital depression and anxiety symptoms following stroke with 3 months- depression, anxiety and functional outcome. J Clin Neurosci, 98, 133–136. https://doi.org/10.1016/j.jocn.2022.02.010
32 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders : DSM-5. (Fifth edition.). https://doi-org.proxy.lib.pacificu.edu/10.1176/appi. books.9780890425596
33 Snaith, R. P., & Zigmond, A. S. (1986, February 1). The hospital anxiety and depression scale. British Medical Journal (Clinical Research Ed.), 292(6516), 344–344. https://doi.org/10.1136/bmj.292.6516.344
34 Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
35 Hamilton, M. (1960, February). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62 https://doi.org/10.1136/jnnp.23.1.56
36 Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515
https://doi.org/10.3928/0048-5713-20020901-06
37. Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961, June). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571.
https://doi.org/10.1001/archpsyc.1961.01710120031004
38. Yesavage, J. A. (1988). Geriatric depression scale. Psychopharmacology Bulletin, 24(4), 709–711.
https://pubmed.ncbi.nlm.nih.gov/3249773
39 Ferro, J. M., Caeiro, L., & Figueira, M. L. (2016, May). Neuropsychiatric sequelae of stroke. Nature Reviews. Neurology, 12(5), 269–280
https://doi.org/10.1038/nrneurol.2016.46
40 Meader, N., Moe-Byrne, T., Llewellyn, A., & Mitchell, A. J. (2014, February). Screening for poststroke major depression: A meta-analysis of diagnostic validity studies. Journal of Neurology, Neurosurgery, and Psychiatry, 85(2), 198–206
https://doi.org/10.1136/jnnp-2012-304194
41 de Man-van Ginkel, J. M., Hafsteinsdóttir, T., Lindeman, E., Burger, H., Grobbee, D., & Schuurmans, M. (2012, March). An efficient way to detect poststroke depression by subsequent administration of a 9-item and a 2-item Patient Health Questionnaire. Stroke, 43(3), 854–856
https://doi.org/10.1161/STROKEAHA.111.640276
42. Manea, L., Gilbody, S., Hewitt, C., North, A., Plummer, F., Richardson, R., . . . McMillan, D. (2016, October). Identifying depression with the PHQ-2: A diagnostic meta-analysis. Journal of Affective Disorders, 203, 382–395.
https://doi.org/10.1016/j.jad.2016.06.003
43. Prisnie, J. C., Fiest, K. M., Coutts, S. B., Patten, S. B., Atta, C. A., Blaikie, L., . . . Jetté, N. (2016, April). Validating screening tools for depression in stroke and transient ischemic attack patients. International Journal of Psychiatry in Medicine, 51(3), 262–277. https://doi.org/10.1177/0091217416652616
44 Aitken, R. C. (1969, October). Measurement of feelings using visual analogue scales. Proceedings of the Royal Society of Medicine, 62(10), 989–993
https://doi.org/10.1177/003591576906201005
45 Berg, A., Lönnqvist, J., Palomäki, H., & Kaste, M. (2009, February). Assessment of depression after stroke: A comparison of different screening instruments. Stroke, 40(2), 523–529 https://doi.org/10.1161/STROKEAHA.108.527705
46 Barrows, P. D., & Thomas, S. A. (2018, January). Assessment of mood in aphasia following stroke: Validation of the Dynamic Visual Analogue Mood Scales (D-VAMS). Clinical Rehabilitation, 32(1), 94–102
https://doi.org/10.1177/0269215517714590
47. National Alliance on Mental Illness. (2023). Mental health by the numbers, infographics and facts sheet.
https://nami.org/About-Mental-Illness/Mental-Health-by-the-Numbers/ Infographics-Fact-Sheets
67
48 Broomfield, N. M., Quinn, T. J., Abdul-Rahim, A. H., Walters, M. R., & Evans, J. J. (2014, October 1). Depression and anxiety symptoms post-stroke/TIA: Prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurology, 14(1), 198–198. https://doi.org/10.1186/s12883-014-0198-8
49 Burton, C. A., Murray, J., Holmes, J., Astin, F., Greenwood, D., & Knapp, P. (2013, October). Frequency of anxiety after stroke: A systematic review and meta-analysis of observational studies. Int J Stroke, 8(7), 545–559. https://doi.org/10.1111/j.1747-4949.2012.00906.x
50 Knapp, P., Dunn-Roberts, A., Sahib, N., Cook, L., Astin, F., Kontou, E., & Thomas, S. A. (2020, April). Frequency of anxiety after stroke: An updated systematic review and metaanalysis of observational studies. Int J Stroke, 15(3), 244–255 https://doi.org/10.1177/1747493019896958
51. Chun, H. Y., Whiteley, W. N., Dennis, M. S., Mead, G. E., & Carson, A. J. (2018, March). Anxiety after stroke: The importance of subtyping. Stroke, 49(3), 556–564. https://doi.org/10.1161/STROKEAHA.117.020078
52 Ayerbe, L., Ayis, S. A., Crichton, S., Wolfe, C. D. A., & Rudd, A. G. (2014, July). Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: The South London Stroke Register. Age and Ageing, 43(4), 542–547
https://doi.org/10.1093/ageing/aft208
53. Wright, F., Wu, S., Chun, H.-Y. Y., & Mead, G. (2017). Factors associated with poststroke anxiety: A systematic review and meta-analysis. Stroke Research and Treatment, 2017, 2124743.
https://doi.org/10.1155/2017/2124743
54 Menlove, L., Crayton, E., Kneebone, I., Allen-Crooks, R., Otto, E., & Harder, H. (2015, June). Predictors of anxiety after stroke: A systematic review of observational studies. J Stroke Cerebrovasc Dis, 24(6), 1107–1117
https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.12.036
55. Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006, May 22). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097
https://doi.org/10.1001/archinte.166.10.1092
56 Beck, A. T., Epstein, N., Brown, G., & Steer, R. (1988). Beck Anxiety Inventory [Database record]. APA PsycTests. https://doi.org/10.1037/t02025-000
57 Hamilton, M. (1959). The assessment of anxiety states by rating. The British Journal of Medical Psychology, 32(1), 50–55. https://doi.org/10.1111/j.2044-8341.1959.tb00467.x
58 Kronenberg, G., Schöner, J., Levitanus, M., Alvarado Balderrama, A. V., Geran, R., Laumeier, I., . . . Gertz, K. (2021, April). The importance of previous lifetime trauma in stroke-induced PTSD symptoms and mental health outcomes. Journal of Psychiatric Research, 136, 589–594.
https://doi.org/10.1016/j.jpsychires.2020.10.033
59 Ferro, J. M., Caeiro, L., & Figueira, M. L. (2016, May). Neuropsychiatric sequelae of stroke. Nature Reviews. Neurology, 12(5), 269–280
https://doi.org/10.1038/nrneurol.2016.46
60 Edmondson, D., Richardson, S., Fausett, J. K., Falzon, L., Howard, V. J., & Kronish, I. M. (2013, June 19). Prevalence of PTSD in survivors of stroke and transient ischemic attack: A meta-analytic review. PLoS One, 8(6), e66435–e66435.
https://doi.org/10.1371/journal.pone.0066435
61 First, M. B., & Ross, R. (2000). American Psychiatric Association: diagnostic and statistical manual of mental disorders. Washington 5th ed. text rev.
62 Kronish, I. M., Edmondson, D., Goldfinger, J. Z., Fei, K., & Horowitz, C. R. (2012). Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke (1970), 43(8), 2192–2197.
https://doi.org/10.1161/STROKEAHA.112.655209
63 Goldfinger, J. Z., Edmondson, D., Kronish, I. M., Fei, K., Balakrishnan, R., Tuhrim, S., & Horowitz, C. R. (2014, MayJun). Correlates of post-traumatic stress disorder in stroke survivors. J Stroke Cerebrovasc Dis, 23(5), 1099–1105.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.09.019
64 Pedowitz, E., Derby, L., Cruz, G. J., Trainor, A., Edmondson, D., & Cornelius, T. (2021, May-Jun). Relationship between NIH stroke symptoms and post-traumatic stress disorder in patients evaluated for transient ischemic attack/stroke. General Hospital Psychiatry, 70, 98–102
https://doi.org/10.1016/j.genhosppsych.2021.03.004
65. Rutovic, S., Kadojic, D., Dikanovic, M., Solic, K., & Malojcic, B. (2021, April). Prevalence and correlates of post-traumatic stress disorder after ischaemic stroke. Acta Neurologica Belgica, 121(2), 437–442
https://doi.org/10.1007/s13760-019-01200-9
66. Weiss, D., & Marmar, C. (1997). The impact of event scale— revised. W: Wilson J., Keane T.(red.). Assessing psychological trauma and PTSD: A handbook for practitioners.
67. Prins, A., Bovin, M. J., Smolenski, D. J., Marx, B. P., Kimerling, R., Jenkins-Guarnieri, M. A., . . . Tiet, Q. Q. (2016, October). The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211 https://doi.org/10.1007/s11606-016-3703-5
68 Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993, Oct). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. In annual convention of the international society for traumatic stress studies, San Antonio, TX (Vol. 462).
69 Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (pcl-5). 10(4), 206. http://www.ptsd.va.gov/
70. Frank, D., Gruenbaum, B. F., Zlotnik, A., Semyonov, M., Frenkel, A., & Boyko, M. (2022). Pathophysiology and current drug treatments for post-stroke depression: a review. International Journal of Molecular Sciences, 23(23), 15114–. https://doi.org/10.3390/ijms232315114
71 Woranush, W., Moskopp, M. L., Sedghi, A., Stuckart, I., Noll, T., Barlinn, K., & Siepmann, T. (2021, November 19). Preventive approaches for post-stroke depression: Where do we stand? a systematic review. Neuropsychiatric Disease and Treatment, 17, 3359–3377. https://doi.org/10.2147/NDT.S337865
68 Delaware Journal of Public Health - August 2023
72 Chun, H. Y. Y., Ford, A., Kutlubaev, M. A., Almeida, O. P., & Mead, G. E. (2022). Depression, anxiety, and suicide after stroke: a narrative review of the best available evidence. Stroke (1970), 53(4), 1402–1410.
https://doi.org/10.1161/STROKEAHA.121.035499
73. Love, M. F., Sharrief, A., Chaoul, A., Savitz, S., & Beauchamp, J. E. S. (2019). Mind-body interventions, psychological stressors, and quality of life in stroke survivors: a systematic review. Stroke (1970), 50(2), 434–440.
https://doi.org/10.1161/STROKEAHA.118.021150
74. Medeiros, G. C., Roy, D., Kontos, N., & Beach, S. R. (2020, Sep-Oct). Post-stroke depression: A 2020 updated review. General Hospital Psychiatry, 66, 70–80
https://doi.org/10.1016/j.genhosppsych.2020.06.011
75 Wijeratne, T., Sales, C., & Wijeratne, C. (2022, July 7). A narrative review on the non-pharmacologic interventions in post-stroke depression. Psychology Research and Behavior Management, 15, 1689–1706
https://doi.org/10.2147/PRBM.S310207
76 Mortensen, J. K., & Andersen, G. (2021, June).
Pharmacological management of post-stroke depression: An update of the evidence and clinical guidance. Expert Opinion on Pharmacotherapy, 22(9), 1157–1166. https://doi.org/10.1080/14656566.2021.1880566
77. Carvalho, A. F., Sharma, M. S., Brunoni, A. R., Vieta, E., & Fava, G. A. (2016). The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: A critical review of the literature. Psychotherapy and Psychosomatics, 85(5), 270–288
https://doi.org/10.1159/000447034
78 Laporte, S., Chapelle, C., Caillet, P., Beyens, M.-N., Bellet, F., Delavenne, X., Bertoletti, L. (2017, April). Bleeding risk under selective serotonin reuptake inhibitor (SSRI) antidepressants: A meta-analysis of observational studies. Pharmacological Research, 118, 19–32.
https://doi.org/10.1016/j.phrs.2016.08.017
79. Dwyer Hollender, K. (2014, June). Screening, diagnosis, and treatment of post-stroke depression. J Neurosci Nurs, 46(3), 135–141.
https://doi.org/10.1097/JNN.0000000000000047
80. Knapp, P., Campbell Burton, C. A., Holmes, J., Murray, J., Gillespie, D., Lightbody, C. E., ..., & Knapp, P. (2017). Interventions for treating anxiety after stroke. Cochrane Database of Systematic Reviews, 2017(5), CD008860–. https://doi.org/10.1002/14651858.CD008860.pub3
81 Ahrens, J., Shao, R., Blackport, D., Macaluso, S., Viana, R., Teasell, R., & Mehta, S. (2023, May). Cognitive -behavioral therapy for managing depressive and anxiety symptoms after stroke: A systematic review and meta-analysis. Topics in Stroke Rehabilitation, 30(4), 368–383. https://doi.org/10.1080/10749357.2022.2049505
82. Wang, S. B., Wang, Y.-Y., Zhang, Q.-E., Wu, S.-L., Ng, C. H., Ungvari, G. S., . . . Xiang, Y.-T. (2018, August 1). Cognitive behavioral therapy for post-stroke depression: A metaanalysis. Journal of Affective Disorders, 235, 589–596. https://doi.org/10.1016/j.jad.2018.04.011
83 Lee, Y., Chen, B., Fong, M. W. M., Lee, J.-M., Nicol, G. E., Lenze, E. J., . . . Wong, A. W. K. (2021, May). Effectiveness of non-pharmacological interventions for treating post-stroke depressive symptoms: Systematic review and meta-analysis of randomized controlled trials. Topics in Stroke Rehabilitation, 28(4), 289–320 https://doi.org/10.1080/10749357.2020.1803583
84 Patel, K., Watkins, C. L., Sutton, C. J., Holland, E.-J., Benedetto, V., Auton, M. F., . . . Lightbody, C. E. (2018, September 25). Motivational interviewing for low mood and adjustment early after stroke: A feasibility randomised trial. Pilot and Feasibility Studies, 4(1), 152–152.
https://doi.org/10.1186/s40814-018-0343-z
85 Cheng, Y. C., Kuo, P.-H., Su, M.-I., & Huang, W.-L. (2022, April). The efficacy of non-invasive, non-convulsive electrical neuromodulation on depression, anxiety and sleep disturbance: A systematic review and meta-analysis. Psychological Medicine, 52(5), 801–812
https://doi.org/10.1017/S0033291721005560
86. Starkstein, S. E., & Hayhow, B. D. (2019, June 25). Treatment of post-stroke depression. Current Treatment Options in Neurology, 21(7), 31
https://doi.org/10.1007/s11940-019-0570-5
87. Zou, L., Yeung, A., Zeng, N., Wang, C., Sun, L., Thomas, G. A., & Wang, H. (2018). Effects of mind-body exercises for mood and functional capabilities in patients with stroke: an analytical review of randomized controlled trials. International Journal of Environmental Research and Public Health, 15(4), 721–. https://doi.org/10.3390/ijerph15040721
88. Chan, W., Immink, M. A., & Hillier, S. (2012, May-Jun). Yoga and exercise for symptoms of depression and anxiety in people with poststroke disability: A randomized, controlled pilot trial. Alternative Therapies in Health and Medicine, 18(3), 34–43. https://pubmed.ncbi.nlm.nih.gov/22875560
89 Blumenthal, J. A., & Rozanski, A. (2023, Mar-Apr). Exercise as a therapeutic modality for the prevention and treatment of depression. Progress in Cardiovascular Diseases, 77, 50–58. https://doi.org/10.1016/j.pcad.2023.02.008
90 Meister, K., & Juckel, G. (2018, May). A systematic review of mechanisms of change in body-oriented yoga in major depressive disorders. Pharmacopsychiatry, 51(3), 73–81. https://doi.org/10.1055/s-0043-111013
91 Delaware Bioscience Association. (2023). Delaware Bio, 2023 https://www.delawarebio.org
92 USA FACTS. (2023). Health. https://usafacts.org/data/topics/people-society/health/
93. AARP. (2022, Jan). Census data for Delaware shows growth in 65+ population https://states.aarp.org/delaware/census-data-for-delaware-showsgrowth-in-65-population
94. Stein, L. A., Goldmann, E., Zamzam, A., Luciano, J. M., Messé, S. R., Cucchiara, B. L., Mullen, M. T. (2018, November 2). Association between anxiety, depression, and post-traumatic stress disorder and outcomes after ischemic stroke. Frontiers in Neurology, 9, 890–890 https://doi.org/10.3389/fneur.2018.00890
69
Cognitive Rehabilitation Interventions for Post-Stroke Populations
Meghan Mulhern, M.A., C.C.C.-S.L.P. Christiana Care Health System & Good Shepherd Penn Partners
As of 2023, stroke continues to be one of leading causes of significant long-term disability in the United States.1 Cognitive deficits are a common component of post-stroke sequala, limiting or impacting participation in functional activities of daily living. In addition to having substantial impacts on the individual diagnosed with stroke, family members, caregivers, and society also absorb the impacts of post stroke cognitive impairment in acute and chronic phases of recovery. It is estimated that approximately 60% of individuals have cognitive impairments as a result of stroke in the acute stages of recovery (within one year of their stroke) and those who experience mild severity deficits have the highest occurrence of recovery.2,3
Given the high incidence of stroke and resultant significant impacts of cognitive impairment, there is a substantial need for evidence-based interventions and multidisciplinary efforts to facilitate return to independence, work, and participation in functional aspects of daily living.4 Cognitive rehabilitation addresses skills in the cognitive domains of attention, memory, and executive functioning and how they impact functionality and safety. In a course of cognitive rehabilitation, rehabilitative therapists commonly refer to more advanced activities of daily living that require increased cognitive demands as Instrumental Activities of Daily Living (IADLs). Examples of IADLs may include meal preparation, managing medications, housekeeping, managing financial responsibilities, time management for appointments, and self-care.
HOW DOES COGNITIVE REHABILITATION START?
Cognitive assessments and interventions that comprise cognitive rehabilitation are within the scope of practice of speechlanguage pathologists (SLP), occupational therapists, and neuropsychologists. In this review, assessment and intervention facilitated by SLPs in cognitive rehabilitation will be explained to inform members of interdisciplinary teams, patients, families, and communities of the beneficial impacts of cognitive rehabilitation for stroke.
The specific education and training of a speech-language pathologist provides expertise in evaluating and intervening on how cognitive deficits impact communication within the modalities of speaking, listening, reading, and writing, which are frequently included in the demands of IADLs. In many cases, the location of stroke or brain injury can largely assist in predicting the types of cognitive deficits to be expected, given the known function of that location in the brain. The impact of cognitive impairment on communication is described as cognitive-linguistic or cognitive-communication impairment, with further analysis of deficits provided in the areas of attention, memory, executive functioning, and language. SLP involvement in cognitive rehabilitation is noted to be separate from other types of rehabilitation interventions aimed at treating aphasia and motor speech disorders that also may result from stroke and can be addressed by a SLP.
Cognitive domains addressed in cognitive-linguistic interventions include attention, memory, and executive functioning, with each domain having further sub-divisions to more specifically describe skills. Skills in attention are recognized in a hierarchy, including focused, sustained, selective, alternating, and divided attention. Deficits in visual attention, commonly observed to be a unilateral neglect, are also recognized under the domain of attention and functionally impact reading and writing. In the context of poststroke cognitive impairments, deficits in memory are commonly observed in subcategories of verbal and nonverbal memory, short term memory or delayed recall, working memory, and prospective memory. Executive functioning refers to skills and abilities for reasoning, judgement, problem solving, sequencing, inhibition, self-monitoring, information processing, and attention to detail.5,6 The combination of skills in these domains interact for completion of IADLs.
Some cognitive-communication deficits are found to be specifically related to right hemisphere damage caused by stroke or acquired brain injuries. In addition to impairments in the aforementioned areas of cognition, right hemisphere damage may demonstrate more specific impacts on macrostructure components of verbal discourse and discourse comprehension. Skills in word retrieval, syntax, grammar, and phonological processing might not be negatively impacted as commonly seen in aphasia.5 Additional impairments specific to right hemisphere damage also include reduced insight or awareness of deficits, known as anosagnosia, and visual neglects, typically causing one to ignore stimuli in left visual field.7
SLPs, occupational therapists (OTs), and neuropsychologists have consistent roles in initial and ongoing assessment of cognitive functioning to inform cognitive rehabilitation programs across a variety of treatment settings, such as acute or subacute rehabilitation facilities or therapy provided in the home, outpatient, or community-based locations. Assessment begins with screening to determine appropriate options for more specific evaluation of cognitive domains, which can include formal and informal assessment procedures to inform clinical impression of skills in functional contexts. Assessment must also recognize culturally and linguistically relevant stimuli and input from the patient, patient’s family or support person, and interprofessional team as part of comprehensive approach.5 With all components of current skills and prior level of functioning considered, severity ratings may be provided to further describe current level of functioning or degree of impairment. Not only are descriptive terms and severity ratings essential for tracking progress, but they are also informative in planning interventions and identifying needs for support in daily activities for self-care, independent living, or return to work.
Although assessment terminology is often centralized around identifying impairments or deficits, the consensus among evidence supporting cognitive rehabilitation intends to improve overall participation in personally relevant, functional tasks.
70 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.012
Progress is measured in generalization and carryover of skills or strategies and participation in meaningful tasks. This motive also stems from the World Health Organization International Classification of Functioning, Disability, and Health (WHOICF) framework, which promotes capitalizing on strengths and addressing barriers to success.4 Cognitive rehabilitation should provide simulations of how the different domains of cognition intricately interact in activities of daily living and patient specific goals to reduce disability.
WHAT DO COGNITIVE REHABILITATION INTERVENTIONS ENTAIL?
Trends in literature continue to suggest the highest evidence support for cognitive rehabilitation is demonstrated when measured in patient reported outcomes concerning participation in functional tasks versus measured performance in specific, non-IADL functions within the different cognitive domains.8 This trend continues to reiterate the goal of participation in cognitive rehabilitation and allows for recognizing the carryover of trained strategies that ultimately may require skills in more than one domain of cognition. In keeping with principles of neuroplasticity, interventions are also recommended to be high frequency, patient-specific, meaningful, and to promote for generalization.5,6 The specific domains of cognition are, however, considered in development of treatment goals and activities and may be necessary to measure progress specifically as a result of interventions.
Like other concepts of rehabilitation, interventions in cognitive rehabilitation can be classified into restorative and compensatory approaches. Restorative approaches attempt to repair or restore an impaired function. Compensatory approaches teach and carryover new strategies, skills, or accommodations to compensate for deficits when original function may not be able be fully recovered.5,6 Often, family members or a support person is not only beneficial, but essential in the success in carryover of new skills or strategies. Therefore, their participation in training within treatment sessions is highly encouraged and even required prior to discharge in some situations.
Efforts to increase the evidence base for cognitive rehabilitation are ongoing because of the heterogeneity of cognitive impairments post stroke as well as the heterogeneity of participants in supporting studies. Because of this, evidence-based practice for cognitive rehabilitation for post stroke impairments may also draw upon support for cognitive rehabilitation serving individuals with acquired or traumatic brain injuries (TBI).
Attention
Direct approaches to attention in therapeutic interventions may include addressing specific levels of attention. Focused attention is the most basic level of attention, with the ability to respond to stimuli in any form, including auditory, visual or tactile. Following focused attention is sustained attention, which describes abilities to maintain attention for a duration of time. Examples of sustained attention may include reading a book, brushing teeth, or listening to a lecture. Selective attention includes completing similar activities of sustained attention, but with an additional distractor present that would require active filtering of said distraction to remain on target. Alternating attention requires abilities to shift attention between stimuli,
including pausing one task, starting another task, and returning to the first task. Lastly, divided attention entails completing two tasks or responding to and processing two types of stimuli simultaneously and accurately. This is considered the highest or most complex form of attention. Examples of divided attention may include having a conversation while cooking a meal or listening to music while responding to emails.6
Based on performance within the different levels of attention, rehabilitation therapists may generate relevant, functional tasks to target these skills within restorative and compensatory techniques. Some restorative approaches with computer-based training and Attention Process Training (APT) have been studied in isolation with gains measured in their specific types of trained tasks, however, have not found to be significant in improving functional carryover to other tasks and patient perceived performance in IADLs.8,9
However, these types of interventions provided in combination with additional compensatory strategy training demonstrated the most functional and positive outcomes of attention skills in carryover measures as well within increased white matter microstructural changes and redistribution of the cerebral attention network in neuroimaging following brain injury and stroke.8,10–12 Specific examples of direct attention training can include cancellation tasks with single or alternating targets and completing tasks within presence or absence of a variety of distractors. Compensatory strategy training begins with education of potential distractors and their impact on overall accuracy in tasks to promote awareness or understanding for attentional strategies. Specific strategies might include managing internal and external distractions or segmenting tasks into smaller steps or shorter durations. Distractions can be present via auditory or visual stimuli as well as within physical symptoms, emotions, or internal thoughts.5,6 Because attention skills are required for further information processing in memory and executive functioning tasks, basic or complex attention will be assessed and addressed to further improve performance in tasks that may initially be classified with memory or executive functioning demands.
Apart from the previously described levels of attention, cognitive rehabilitation may also address unilateral visual neglects under the domain of attention. Interventions provided by SLPs will specifically target increasing awareness of unilateral neglect and attention to the neglected side within communication tasks requiring reading and writing. Some examples of intervention include providing multimodal cueing or brightly colored materials to improve response to all stimuli in targeted visual field within describing pictures, reading, providing written instructions, or completing IADL tasks.5
Memory
Intervention for memory skills in cognitive rehabilitation typically targets delayed recall or short term memory, working memory for short term information processing, and prospective memory, recall of a planned task or action.5,6 Across all forms of memory in therapy targets, both restorative and compensatory approaches are again considered. Restorative approaches within evidence-based practice for cognitive rehabilitation may include trials of spaced or distributed practice or retrieval along with errorless learning, an instructional technique in which errors are
71
minimized or avoided prior to advancing to the next step of a task.13–16 These interventions would likely initially occur in a highintensity format in therapy sessions directed by a speech-language pathologist, but could also be trained for family members or caregivers to replicate for carryover and memory benefit outside of therapy sessions.
There is a larger body of support for training of compensatory memory strategies across all severity ranges of impairments for memory.8 Compensatory strategy training for memory can be further divided into internal and external strategies. Internal strategies may include use of mnemonics, visualizations or imagery, associations, rehearsal, repetition, and semantic elaborations, including using additional associations with preexisting knowledge or identifying multiple salient features of the memory target. External compensatory memory strategies entail any use of external storage of information apart from the brain with examples including calendars, to-do lists, journals, recordings, labels, pictures, alarms, timers or use of technology for prospective reminders.5,6 For moderate to severe memory deficits, recommendations for intervention include emphasis on errorless learning and external memory strategies. Internal memory strategies have demonstrated increased effectiveness with more mild severity memory deficits and for those with a considerable level of cognitive reserve, because of the additional executive functioning skills required for strategy carryover.8 Participation in a course of cognitive rehabilitation with a SLP can help select which memory interventions would be suitable for patient specific goals.
Executive Functioning
Executive functioning skills are often required for successful carryover of memory and attention strategies, however, can also be also at risk for impairment in the setting of stroke. If executive functioning impairments are severe, interventions may need to target increasing awareness to cognitive impairment and training of individual functional tasks with understanding that skill acquisition may not carryover to untrained tasks.8,17 Goals to address executive functioning skills in therapy may include improving accuracy in reasoning, attention to detail, problem solving, and sequencing with tasks mimicking demands for return to independent living or work. Maximum inclusion of scenarios, stimuli, or personally relevant information is recommended to facilitate carryover of improved accuracy and strategy use outside of therapy and in real life context.
For mild to moderate severity deficits in executive functioning, evidence supports metacognitive and compensatory strategy training.5,8 Metacognition is the awareness of one’s own thought processes, which may include understanding specific changes in cognitive functioning and anticipating their impact. Applying metacognitive strategies evokes a “top down” approach in evaluating and adapting performance, specifically with cognitive demands, in everyday activities.18 The first stage of metacognitive strategy training requires awareness of potential cognitive deficits.19 This can be facilitated in therapy sessions, but is ultimately most successful or meaningful with personally relevant experiences or tasks. Following developed awareness, training in therapy would teach strategies for executive functioning or other domains of cognition and facilitate planning carryover of strategies. The final step would be self-evaluating one’s own performance in tasks to make improvements or adjustments
to performance or task execution as needed.5,19 Standardized or personal rating systems can allow for clear differentiation between expected or predicted accuracy and actual performance when used before, during, and following a task.19 For example, these rating systems may evaluate for accuracy, perceived levels of difficulty, or time required to complete a task, or whatever the goal may be to address. These rating systems can also be helpful for fostering motivation when performance and progress is tracked, and in turn, encourage continued use of self-monitoring skills for a variety of untrained tasks not specifically targeted in therapy sessions.
Other metacognitive strategy approaches include learning to modify or control the environment to allow for carryover of trained strategies to support attention, memory, and additional executive functioning skills or to reduce potential distractions, ultimately improving accuracy or reducing difficulty.5,6 Some individuals significantly benefit from use of graphic organizers, time management strategies, and any strategies to increase organization in the home, with medications, in the work place, or wherever necessary. Metacognitive strategy training has been observed to be effective in acute and chronic phases of recovery post stroke when specifically trained by rehabilitation therapists.8,19 The overall goal of metacognitive strategies is again to reduce the negative impact of cognitive deficits on task execution or performance and increasing independence, with hopeful reduction in disability.18
Although less supporting evidence is available in comparison to metacognitive strategy training post stroke, dual task training has some level of support for restorative approaches to executive functioning within trained tasks.8,20,21 However, dual task training has been more specifically studied with diagnosis of TBI. Dual task training can involve any combination of motor and cognitive tasks that are completed simultaneously.21 The demands of dual task training also simulate similar demands of divided attention, requiring completion of two tasks, at the same time. Dual task training is often applied in other rehabilitation therapies, such as physical therapy and occupational therapy, to address gait training with anticipated distractions present at home or in the community, using simple verbal reasoning tasks completed while walking. Examples of dual task training specifically for cognitive rehabilitation may include shopping while completing calculations, discourse or conversational tasks during cooking, listening and recalling a story while working on a simple or multi-step project. Limited carryover is appreciated for training executive functioning skills to improve further carryover of visual scanning strategies to address unilateral neglect across untrained tasks.8,20 This interaction continues to demonstrate the complex interaction of cognitive skills that benefit from ongoing support by rehabilitative clinicians to facilitate patient specific needs.
Advancements in technology are beginning to find their way into new modalities for cognitive rehabilitation interventions. Virtual Reality (VR) is now being explored to provide simulations of activities of daily living (ADLs) by also targeting underlying cognitive skills in information processing, executive functioning, attention, memory, and language. Their ecological validity continues to be explored, however, shows promising results when used in combination with traditional compensatory strategy training provided by rehabilitative therapists for overall participation gains in ADLs and in some standardized cognitive assessments over short periods of time.8,22
72 Delaware Journal of Public Health - August 2023
Discourse
Cognitive rehabilitation may also include addressing how cognitive impairments negatively impact discourse skills, commonly caused by stroke in the right hemisphere of the brain. Effective communication involves cognitive skills in sustained attention, memory, and executive functioning. Skills in these domains allow for topic recognition, response generation or thought organization, recall of communication partner’s response, and awareness of errors and revisions.5,23
Interventions are structured to target both verbal and comprehension goals and would also require some degree of metacognitive training or communication partner training. Deficits in executive functioning may contribute to increased verbosity, tangentiality, impulsivity, focusing on irrelevant details, and thought disorganization in conversation.5,24 A combination of cognitive deficits can also limit understanding of abstract or figurative language, including information that can be interpreted in many ways requiring mental flexibility. This further can contribute to difficulty making inferences or understanding macrostructure components of conversations, such as the over overall topic or “big picture” of discussions.25,26 Further, indirect forms communication information can become more difficult to decipher, such as emotions, jokes, irony and sarcasm.5
In guidance provided by a speech-language pathologists, these types of discourse difficulties can be addressed with functional, patient specific goals, that may also need to be informed by family members or a support person if awareness to these challenges is reduced. Recommended therapeutic tasks would break down these macrostructure components into smaller units and prompting description of how items may be related to draw or recognize an inference. Examples of stimuli used to target these goals could include discussing news stories, having complex or opinionated discussions, organizing information into pictures to tell a story, or creating outlines for planned speaking tasks.5
CONCLUSION
The overall goals of cognitive rehabilitation in the setting of stroke are to facilitate cognitive function for participation or independence in everyday tasks, to limit the impacts or severity of disability, and to improve quality of life. These needs may evolve over time based on progress, caregiver support, or different phases of recovery after stroke. However, chronicity of stroke recovery should not discourage individuals or families from seeking guidance from rehabilitation professionals to maximize participation in activities of daily living. Individuals and their support systems can benefit from cognitive rehabilitation throughout the stages of stroke recovery if there are functional, task-specific goals related to activities of daily living along with motivation.
Ms. Mulhern may be contacted at meghan.mulhern@christianacare.org
REFERENCES
1. Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., . . . Martin, S. S., & the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2023, February 21). Heart disease and stroke statistics-2023 update: A report from the American Heart Association. Circulation, 147(8), e93–e621. https://doi.org/10.1161/CIR.0000000000001123
2. El Husseini, N., Katzan, I. L., Rost, N. S., Blake, M. L., Byun, E., Pendlebury, S. T., . . . Smith, E. E., & the American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Council on Lifestyle and Cardiometabolic Health. (2023, June). Cognitive impairment after ischemic and hemorrhagic stroke: A scientific statement from the American Heart Association/American Stroke Association. Stroke, 54(6), e272–e291.
https://doi.org/10.1161/STR.0000000000000430
3. Tang, E. Y., Amiesimaka, O., Harrison, S. L., Green, E., Price, C., Robinson, L., . . . Stephan, B. C. (2018, January 15). longitudinal effect of stroke on cognition: A systematic review. Journal of the American Heart Association, 7(2), e006443. https://doi.org/10.1161/JAHA.117.006443
4. World Health Organization. (2001). The international classification of functioning, disability and health (ICF). Geneva: WHO.
5 American Speech-Language-Hearing Association. (n.d). Right hemisphere damage. (Practice Portal). Retrieved from www.asha.org/Practice-Portal/Clinical-Topics/Right-Hemisphere-Damage/
6. American Speech-Language-Hearing Association. (n.d.). Traumatic brain injury in adults (Practice Portal). Retrieved from www.asha.org/Practice-Portal/Clinical-Topics/Traumatic-Brain-Injuryin-Adults/
7. Salvato, G., Sedda, A., & Bottini, G. (2014, September). In search of the disappeared half of it: 35 years of studies on representational neglect. Neuropsychology, 28(5), 706–716. https://doi.org/10.1037/neu0000062
8. Cicerone, K. D., Goldin, Y., Ganci, K., Rosenbaum, A., Wethe, J. V., Langenbahn, D. M., . . . Harley, J. P. (2019, August). Evidence-based cognitive rehabilitation: Systematic review of the literature from 2009 through 2014. Archives of Physical Medicine and Rehabilitation, 100(8), 1515–1533.
https://doi.org/10.1016/j.apmr.2019.02.011
9. Barker-Collo, S. L., Feigin, V. L., Lawes, C. M., Parag, V., Senior, H., & Rodgers, A. (2009, October). Reducing attention deficits after stroke using attention process training: A randomized controlled trial. Stroke, 40(10), 3293–3298.
https://doi.org/10.1161/STROKEAHA.109.558239
10. Kim, Y. H., Yoo, W. K., Ko, M. H., Park, C. H., Kim, S. T., & Na, D. L. (2009, June). Plasticity of the attentional network after brain injury and cognitive rehabilitation. Neurorehabilitation and Neural Repair, 23(5), 468–477. https://doi.org/10.1177/1545968308328728
11. Nordvik, J. E., Schanke, A. K., Walhovd, K., Fjell, A., Grydeland, H., & Landrø, N. I. (2012). Exploring the relationship between white matter microstructure and working memory functioning following stroke: A single case study of computerized cognitive training. Neurocase, 18(2), 139–151. https://doi.org/10.1080/13554794.2011.568501
12. Fernández, E., Bringas, M. L., Salazar, S., Rodríguez, D., García, M. E., & Torres, M. (2012, October). Clinical impact of RehaCom software for cognitive rehabilitation of patients with acquired brain injury. MEDICC Review, 14(4), 32–35.
https://doi.org/10.37757/MR2012V14.N4.8
73
13. Ownsworth, T., Fleming, J., Tate, R., Shum, D. H., Griffin, J., Schmidt, J., . . . Chevignard, M. (2013, November 5). Comparison of error-based and errorless learning for people with severe traumatic brain injury: Study protocol for a randomized control trial. Trials, 14, 369. https://doi.org/10.1186/1745-6215-14-369
14. Sohlberg, M. M., & Mateer, C. A. (2001). Cognitive rehabilitation: An integrative neuropsychological approach. New York, NY: Guilford.
15 Sohlberg, M. M., & Turkstra, L. S. (2011). Optimizing cognitive rehabilitation: Effective instructional methods. New York, NY: Guilford.
16 Melton, A., & Bourgeois, M. (2005). Training compensatory memory strategies via the telephone for persons with TBI. Aphasiology, 19, 353–364 https://doi.org/10.1080/02687030444000804
17. Rotenberg-Shpigelman, S., Erez, A. B., Nahaloni, I., & Maeir, A. (2012). Neurofunctional treatment targeting participation among chronic stroke survivors: A pilot randomised controlled study. Neuropsychological Rehabilitation, 22(4), 532–549. https://doi.org/10.1080/09602011.2012.665610
18. Jaywant, A., Mautner, L., Waldman, R., O’Dell, M. W., Gunning, F. M., & Toglia, J. (2023, May 4). Feasibility and acceptability of a remotely delivered executive function intervention that combines computerized cognitive training and metacognitive strategy training in chronic stroke. International Journal of Environmental Research and Public Health, 20(9), 5714. https://doi.org/10.3390/ijerph20095714
19. Skidmore, E. R., Holm, M. B., Whyte, E. M., Dew, M. A., Dawson, D., & Becker, J. T. (2011, April). The feasibility of meta-cognitive strategy training in acute inpatient stroke rehabilitation: Case report. Neuropsychological Rehabilitation, 21(2), 208–223. https://doi.org/10.1080/09602011.2011.552559
20. van Kessel, M. E., Geurts, A. C., Brouwer, W. H., & Fasotti, L. (2013, July 10). visual scanning training for neglect after stroke with and without a computerized lane tracking dual task. Frontiers in Human Neuroscience, 7, 358.
https://doi.org/10.3389/fnhum.2013.00358
21. Evans, J. J., Greenfield, E., Wilson, B. A., & Bateman, A. (2009, January). Walking and talking therapy: Improving cognitivemotor dual-tasking in neurological illness. J Int Neuropsychol Soc, 15(1), 112–120. https://doi.org/10.1017/S1355617708090152
22. Faria, A. L., Pinho, M. S., Bermúdez I Badia, S. (2020, June 16). A comparison of two personalization and adaptive cognitive rehabilitation approaches: A randomized controlled trial with chronic stroke patients. Journal of Neuroengineering and Rehabilitation, 17(1), 78.
https://doi.org/10.1186/s12984-020-00691-5
23. Berube, S. K., Goldberg, E., Sheppard, S. M., Durfee, A. Z., Ubellacker, D., Walker, A., . . . Hillis, A. E. (2022, October 25). An analysis of right hemisphere stroke discourse in the modern cookie theft picture. American Journal of SpeechLanguage Pathology, 31(5S), 2301–2312.
https://doi.org/10.1044/2022_AJSLP-21-00294
24 Minga, J. (2016). Discourse production and right hemisphere disorder. Neurophysiology and Neurogenic Speech and Language Disorders, 1, 96–105.
25. Tompkins, C. A., Scharp, V. L., Meigh, K. M., & Fassbinder, W. (2008, February 1). Coarse coding and discourse comprehension in adults with right hemisphere brain damage. Aphasiology, 22(2), 204–223.
https://doi.org/10.1080/02687030601125019
26. Tompkins, C. A., Fassbinder, W., Lehman Blake, M., Baumgaertner, A., & Jayaram, N. (2004, December). Inference generation during text comprehension by adults with right hemisphere brain damage: Activation failure versus multiple activation. J Speech Lang Hear Res, 47(6), 1380–1395.
https://doi.org/10.1044/1092-4388(2004/103)
74 Delaware Journal of Public Health - August 2023
BE A

LEARN TO SPOT A STROKE F.A.S.T.
WHAT IS STROKE?
A stroke occurs when the flow of oxygen to a part of the brain is blocked. Without oxygen, brain cells start to die within a few minutes.
In the United States, nearly 800,000 people have a stroke every year, and around 130,000 of them die from it.
But, stroke is treatable by doctors and the faster the person receives treatment at the hospital, the less likely they are to die or have a disability (like being unable to walk or or talk) from the stroke.

YOU CAN BE A STROKE HERO AND POSSIBLY HELP SAVE A LIFE by learning how to spot a stroke F.A.S.T.!

USE THE LETTERS F-A-S-T to SPOT THE SUDDEN SIGNS OF STROKE and know when to CALL 911.

You can be a Stroke Hero and your superpower is recognizing the signs of stroke, and calling 911 right away.


75
stroke.org
© Copyright 2020 American Heart Association, Inc., a 501(c)(3) not-for-profit. Unauthorized use prohibited. 3/20DS15971 FACE DROOPING ARM WEAKNESS SPEECH DIFFICULTY TIME TO CALL 911
The Effects of Stroke and Stroke Gait Rehabilitation on Behavioral and Neurophysiological Outcomes: Challenges and Opportunities for Future Research
Trisha Kesar, P.T., Ph.D. Division of Physical Therapy, Department of Rehabilitation Medicine, Emory University School of Medicine
ABSTRACT
Stroke continues to be a leading cause of adult disability, contributing to immense healthcare costs. Even after discharge from rehabilitation, post-stroke individuals continue to have persistent gait impairments, which in turn adversely affect functional mobility and quality of life. Multiple factors, including biomechanics, energy cost, psychosocial variables, as well as the physiological function of corticospinal neural pathways influence stroke gait function and training-induced gait improvements. As a step toward addressing this challenge, the objective of the current perspective paper is to outline knowledge gaps pertinent to the measurement and retraining of stroke gait dysfunction. The paper also has recommendations for future research directions to address important knowledge gaps, especially related to the measurement and rehabilitation-induced modulation of biomechanical and neural processes underlying stroke gait dysfunction. We posit that there is a need for leveraging emerging technologies to develop innovative, comprehensive, methods to measure gait patterns quantitatively, to provide clinicians with objective measure of gait quality that can supplement conventional clinical outcomes of walking function. Additionally, we posit that there is a need for more research on how the stroke lesion affects multiple parts of the nervous system, and to understand the neuroplasticity correlates of gait training and gait recovery. Multimodal clinical research studies that can combine clinical, biomechanical, neural, and computational modeling data provide promise for gaining new information about stroke gait dysfunction as well as the multitude of factors affecting recovery and treatment response in people with post-stroke hemiparesis.
INTRODUCTION
Stroke is a leading cause of adult disability in the United States,1 with stroke prevalence, stroke-related healthcare costs, and public health burden expected to increase in the next 20 years.2 Gait dysfunction persists at discharge from rehabilitation in over 2/3rd stroke survivors, adversely affecting community participation and quality of life.3–6 Due to the importance of walking in daily activities, restoration of gait function is a major goal of rehabilitation.4,7 However, stroke gait deficits are complex and multi-factorial. Stroke gait impairments adversely affect kinematics and kinetics in all paretic lower limb joints, disrupt stance and swing phases, and are marked by inter-limb asymmetry.3,8,9 making the diagnosis and identification of targets for treatment challenging. Several gait training interventions have been shown to improve walking function, and there is consensus that stroke survivors benefit from gait rehabilitation.10–15 However, agreement in literature is lacking on how to maximize treatment rehabilitation efficacy.16,17 Also, for a majority of gait interventions, irrespective of whether the intervention is proven to be statistically superior, there is high inter-individual variability in treatment effects.16,18,19 While a subset of stroke participants show large or meaningful improvements (responders), others do not (non-responders). The challenge is that multiple factors, including biomechanics, energy cost, psychosocial factors,
as well as the physiological function of corticospinal neural pathways influence stroke gait function and training-induced gait improvements. As a step toward addressing this challenge, the objective of the current perspective paper is to outline knowledge gaps and future research opportunities pertinent to the measurement and retraining of gait after stroke.
RECOMMENDATIONS FOR FUTURE RESEARCH RELATED TO MEASURING THE EFFECTS OF STROKE ON GAIT PERFORMANCE AND WALKING FUNCTION USING BEHAVIORAL DATA
Clinical outcomes commonly used to assess sensorimotor impairment (e.g. Fugl-Meyer score) and gait function (e.g. gait speed)20 are an indispensable part of clinical rehabilitation, but they fail to capture gait quality and spatio-temporal movement patterns (how a person is moving). With respect to gait biomechanics outcomes, comprehensively mapping the effects of stroke is challenging because stroke gait impairments adversely affect kinematics (the description of motion) and kinetics (description of forces causing motion) in all paretic lower limb joints, disrupting all phases of gait.8,9 Our laboratory has published several studies that measured post-stroke gait patterns via biomechanical evaluation (gait kinematics and kinetics).
76 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.013
There is high variability in gait biomechanics metrics over the gait cycle between the paretic and nonparetic leg of stroke survivors, compared to an able-bodied individual. These effects of stroke on multiple gait variables across different stroke survivors are often poorly characterized using current approaches. Even with laboratory instrumentation, typically, in biomechanics and rehabilitation research, our lab21–29 and others30–39 use discrete metrics derived from complex gait data (e.g. peak ankle angle, peak anterior ground reaction force (AGRF)) to answer scientific questions about effects of interventions18,22,40–43 However, such univariate analysis of discrete variables fails to capture the multivariate nature of gait deficits. Discrete variables that represent one sub-phase or singular point in the gait cycle may fail to capture the time courses and continuous nature of gait throughout the walking cycle and across multiple cycles. Even the time histories of continuous kinematics and kinetics may fail to capture the inter-dependences between the variables and interlimb coordination over time. There is a need for more research incorporating computational methods to capture multivariate effects of stroke on gait, while accounting for different phases of gait, to derive comprehensive, holistic metrics of gait quality. Furthermore, two stroke survivors with the same gait speed or Fugl-Meyer score can have very different impairments in their gait biomechanics or coordination patterns. Due to lack of access to expensive laboratory equipment and limited treatment time, clinicians commonly also subjectively observe and their patient’s walking patterns without using quantitative data, limiting the objectivity and reproducibility of clinical decision-making. With emerging technologies, wearable sensors and smart phone videos can enable gait to be measured quantitatively in clinical settings. However, these systems still generate a lot of data, subject to interpretation, including multiple joint angles, and over 20-50 spatiotemporal gait metrics.44,45 Thus, another avenue for future research is the development and clinical validation of gait analysis methods that can be applied to clinical settings, while being rapid, objective, intuitive, interpretable, and user-friendly to supplement clinical outcomes.
Biomechanical metrics or computational analysis have strong potential for enhancing our understanding of the biomechanical mechanism underlying rehabilitation response, because they can provide valuable insights about restitution versus compensation as well as underlying changes in motor control. Gait treatments may allow compensation, rather than true restitution, to improve gait speed and endurance. Outcomes of gait function (e.g. gait speed or endurance) lack the specificity to differentiate behavioral restitution from compensation, and fail to elucidate mechanisms. In a 2018 study, three categories of stroke survivors who walked at similar self-selected speeds demonstrated high variability in pelvic excursion deviation and inter-limb asymmetry in gait biomechanics,9 supporting the sensitivity and advantage of biomechanical measures over speed-based outcomes. Use of gait speed and endurance to assess treatment-related improvements, without regard to biomechanical patterns or neuropathological responses is a limitation in gait rehabilitation research. For example, training-induced improvements in speed may be accompanied by improved propulsive symmetry, greater reliance on the nonparetic leg (e.g. for forward propulsion), or energy-inefficient compensations from proximal joints (e.g. circumduction, increased pelvic excursion9). Similarly,
improvements in paretic peak AGRF can be accompanied by worsening of other metrics, including inter-limb propulsion or step length asymmetry, or inefficient compensations in other gait variables at different points in the gait cycle. Previous studies have also suggested that gait rehabilitation efficacy may depend on individual differences in muscle coordination28,46,47 that generate spatiotemporal gait coordination patterns. Individual-specific biophysical modeling methods can also help predict and interpret mechanisms of treatment-induced changes in stroke gait,28,46 and merit more investigation in future research. Finally, multi-modal clinical research studies with inter-disciplinary study teams can combine clinical, biomechanical, and modeling data to gain new information about stroke gait dysfunction as well as factors affecting recovery and treatment response.
RECOMMENDATIONS FOR FUTURE RESEARCH RELATED TO MEASURING THE EFFECTS OF STROKE ON NEURAL CIRCUITS USING NON-INVASIVE HUMAN NEUROPHYSIOLOGY DATA
Stroke induces a cascade of changes in cortical and spinal circuits involved in locomotor control.48–50 The stroke-lesion induces structural and functional changes in cortical, brain stem, and spinal circuitry controlling locomotion.48 Effects of stroke on different neural circuits are complex, with potential disparities at different sites of the neuraxis, necessitating the use of multimodal approaches for in-depth assessment. There is a gap in our understanding of neurobiological processes underlying gait recovery and rehabilitation. The international Stroke Recovery and Rehabilitation Roundtable convened to “move rehabilitation research forward,” listed “identifying neurobiological mechanisms of treatment” and “sequential development, testing, and refining of interventions” as important research goals.51,52
While increasing gait speed, understandably, is a major focus of gait rehabilitation, increases in gait speed may occur via diverse biomechanical and neural mechanisms. Although gait treatments may increase speed by making a compensatory strategy more effective, current neurorehabilitation philosophies based on neuroplasticity principles strive for restitution of deficits. In a 2017 review, Bowden et. al. concluded that “because rehabilitation literature is yet to support a causal, mechanistic link for functional gains post-stroke, a multimodal approach to stroke rehabilitation is necessary.”53 We posit that lack of inclusion of neuroplasticity outcomes is a major limitation in gait rehabilitation research.16,17,51,52,54–59
Neuroplasticity, the capacity of the nervous system to demonstrate structural and functional change in response to experience, is a fundamental yet under-investigated mechanism of stroke gait rehabilitation.48,49,60–64 Neuroplasticity research has helped develop consensus that to induce lasting improvements in gait function, training must incorporate repetitive, intense, and challenging practice,65 and informed innovative clinical algorithms to predict upper limb recovery post-stroke.61,66 Several non-invasive neuromodulation interventions have also been tested to enhance post-stroke recovery.67–69 However, current neuroplasticity principles are still derived largely from upper limb studies, leaving a gap regarding neural substrates of gait treatments. While randomized controlled trials may show that an intervention is
77
efficacious, they often fail to inform us whether the intervention modified the stroke-related neurophysiological sequelae, and why or for whom the intervention is effective.70 Thus, there is a need for a shift toward mechanism-focused clinical trials.52,70
The importance of corticospinal tract and motor cortex (M1) excitability in human locomotor control and stroke recovery is well studied. Transcranial magnetic stimulation-derived outcomes such as motor evoked potential amplitude and motor threshold can supplement clinical and biomechanical measures to evaluate overall corticospinal tract excitability or output in the lesioned hemisphere post-stroke. Paired pulse transcranial magnetic stimulation methods can probe intracortical circuitry, which also plays a role in gait, and can influence traininginduced plasticity.55,71–73 Hoffman’s or H-reflexes and related non-invasive measures (e.g. reciprocal inhibition) can provide valuable measures of spinal circuit physiology, which in turn may be associated with spasticity and coactivation during gait.55,74 In addition to cortical and spinal circuits, the effects of stroke and training-induced neuroplasticity on brain stem, propriospinal, and other circuitry can provide important information to guide future clinical research and practice. Related, measures of brain structure derived using neuro-imaging can supplement neurophysiology, as well as behavioral gait outcomes.
As an example to illustrate research on gait rehabilitationinduced neuroplasticity, high-intensity treadmill training is an evidence-supported treatment that provides practice of thousands of steps and aerobic exercise within a safe, predictable environment. However, depending on the type and content of adjunctive feedback or cues (verbal, biofeedback, stimulation), the effects of the treatment on paretic leg biomechanical deficits may vary. Importantly, neural correlates underlying high-intensity training need more study. A single session of high-intensity interval treadmill walking exacerbated already suppressed ankle muscle corticospinal excitability in the paretic leg post-stroke.75 Four weeks of treadmill training in chronic stroke improved gait speed compared to control treatment, but increased cortical excitability in the non-lesioned hemisphere.76 Similarly, the ‘FastFES’ intervention combines fast treadmill training with functional electrical stimulation (FES) to ankle dorsi- and plantar-flexor muscles timed with the appropriate phase of gait. FastFES is designed to improve paretic leg AGRF by synergistically facilitating more posterior positioning of paretic trailing limb relative to the body’s center of mass and use FES to augment activation of the paretic plantarflexors during late stance—key parameters underlying forward propulsion (L. N. Awad et al., 2016a; Hsiao, Knarr, Higginson, & Binder-Macleod, 2015a).18,77 FastFES forms a valuable gait treatment paradigm because it uses a hypothesis-based biomechanical approach to improve gait function by targeting specific impairments in the paretic leg; has been shown to improve gait speed, endurance, and energy efficiency; and should facilitate motor learning and neuroplasticity.18,22,30 However, similar to most gait interventions, with high-intensity fast treadmill training and FastFES, not all participants improve gait function, with training-induced change in gait speed showing high inter-individual variability.18,37 We posit that inclusion of neurophysiology measures in clinical trials is important to understand how and why an intervention improves gait function, especially with regards to neural mechanisms. Another related limitation in current gait rehabilitation is that intervention-prescription is not determined based on baseline impairments or neurobiological characteristics.
SUMMARY
Stroke continues to be a leading cause of adult disability, contributing to immense healthcare costs. Even after discharge from rehabilitation, post-stroke individuals continue to have persistent gait impairments, which in turn adversely affect functional mobility and quality of life. This perspective paper provides an overview of current research, and recommendations for future research directions to address important knowledge gaps. We posit that there is a need for leveraging emerging technologies to develop innovative, comprehensive, methods to measure gait patterns quantitatively, to provide clinicians with objective measure of gait quality that can supplement conventional clinical outcomes of walking function. Additionally, we posit that there is a need for more research on how the stroke lesion affects multiple part of the nervous system, and to understand the neuroplasticity correlates of gait training and gait recovery.
Dr. Kesar may be contacted at tkesar@emory.edu
REFERENCES
1. American Heart Association. (2012). Heart disease and stroke statistics—2012 update. A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee.
2. Ovbiagele, B., Goldstein, L. B., Higashida, R. T., Howard, V. J., Johnston, S. C., Khavjou, O. A., . . . Trogdon, J. G., & the American Heart Association Advocacy Coordinating Committee and Stroke Council. (2013, August). Forecasting the future of stroke in the United States: A policy statement from the American Heart Association and American Stroke Association. Stroke, 44(8), 2361–2375.
https://doi.org/10.1161/STR.0b013e31829734f2
3. Chen, G., Patten, C., Kothari, D. H., & Zajac, F. E. (2005, August). Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait & Posture, 22(1), 51–56.
https://doi.org/10.1016/j.gaitpost.2004.06.009
4. Mayo, N. E., Wood-Dauphinee, S., Ahmed, S., Gordon, C., Higgins, J., McEwen, S., & Salbach, N. (1999, May-Jun). Disablement following stroke. Disability and Rehabilitation, 21(5-6), 258–268.
https://doi.org/10.1080/096382899297684
5. Olney, S. J., & Richards, C. (1996). Hemiparetic gait following stroke. Part I: Characteristics. Gait & Posture, 4, 136–148.
https://doi.org/10.1016/0966-6362(96)01063-6
6. Turnbull, G. I., Charteris, J., & Wall, J. C. (1995, September). A comparison of the range of walking speeds between normal and hemiplegic subjects. Scandinavian Journal of Rehabilitation Medicine, 27(3), 175–182.
https://pubmed.ncbi.nlm.nih.gov/8602480
7. Vestling, M., Tufvesson, B., & Iwarsson, S. (2003, May). Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. Journal of Rehabilitation Medicine, 35(3), 127–131.
https://doi.org/10.1080/16501970310010475
8. Chen, G., Patten, C., Kothari, D. H., & Zajac, F. E. (2005, August). Gait deviations associated with post-stroke hemiparesis: Improvement during treadmill walking using weight support, speed, support stiffness, and handrail hold. Gait & Posture, 22(1), 57–62.
https://doi.org/10.1016/j.gaitpost.2004.06.008
78 Delaware Journal of Public Health - August 2023
9. Little, V. L., McGuirk, T. E., Perry, L. A., & Patten, C. (2018, May). Pelvic excursion during walking post-stroke: A novel classification system. Gait & Posture, 62, 395–404.
https://doi.org/10.1016/j.gaitpost.2018.03.052
10. Daly, J. J., & Ruff, R. L. (2007, December 20). Construction of efficacious gait and upper limb functional interventions based on brain plasticity evidence and model-based measures for stroke patients. TheScientificWorldJournal, 7, 2031–2045.
https://doi.org/10.1100/tsw.2007.299
11. Hornby, T. G., Campbell, D. D., Kahn, J. H., Demott, T., Moore, J. L., & Roth, H. R. (2008, June). Enhanced gaitrelated improvements after therapist- versus robotic-assisted locomotor training in subjects with chronic stroke: A randomized controlled study. Stroke, 39(6), 1786–1792.
https://doi.org/10.1161/STROKEAHA.107.504779
12. Krebs, H. I., Volpe, B., & Hogan, N. (2009, February 25). A working model of stroke recovery from rehabilitation robotics practitioners. Journal of Neuroengineering and Rehabilitation, 6, 6.
https://doi.org/10.1186/1743-0003-6-6
13. Macko, R. F., Ivey, F. M., Forrester, L. W., Hanley, D., Sorkin, J. D., Katzel, L. I., . . . Goldberg, A. P. (2005, October). Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke: A randomized, controlled trial. Stroke, 36(10), 2206–2211.
https://doi.org/10.1161/01.STR.0000181076.91805.89
14. Moore, J. L., Roth, E. J., Killian, C., & Hornby, T. G. (2010, January). Locomotor training improves daily stepping activity and gait efficiency in individuals poststroke who have reached a “plateau” in recovery. Stroke, 41(1), 129–135.
https://doi.org/10.1161/STROKEAHA.109.563247
15. Whitall, J. (2004, March). Stroke rehabilitation research: Time to answer more specific questions? Neurorehabilitation and Neural Repair, 18(1), 3–8.
https://doi.org/10.1177/0888439003262876
16. Dickstein, R. (2008, Nov-Dec). Rehabilitation of gait speed after stroke: A critical review of intervention approaches. Neurorehabilitation and Neural Repair, 22(6), 649–660.
https://doi.org/10.1177/1545968308315997
17. Dobkin, B. H. (2009, December). Motor rehabilitation after stroke, traumatic brain, and spinal cord injury: Common denominators within recent clinical trials. Current Opinion in Neurology, 22(6), 563–569.
https://doi.org/10.1097/WCO.0b013e3283314b11
18. Awad, L. N., Reisman, D. S., Pohlig, R. T., & Binder-Macleod, S. A. (2016, September 23). Identifying candidates for targeted gait rehabilitation after stroke: Better prediction through biomechanics-informed characterization. Journal of Neuroengineering and Rehabilitation, 13(1), 84.
https://doi.org/10.1186/s12984-016-0188-8
19. Dobkin, B. H., Nadeau, S. E., Behrman, A. L., Wu, S. S., Rose, D. K., Bowden, M., . . . Duncan, P. W. (2014). Prediction of responders for outcome measures of locomotor Experience Applied Post Stroke trial. Journal of Rehabilitation Research and Development, 51(1), 39–50.
https://doi.org/10.1682/JRRD.2013.04.0080
20. Burke, E., Dobkin, B. H., Noser, E. A., Enney, L. A., & Cramer, S. C. (2014, August). Predictors and biomarkers of treatment gains in a clinical stroke trial targeting the lower extremity. Stroke, 45(8), 2379–2384.
https://doi.org/10.1161/STROKEAHA.114.005436
21. Awad, L. N., Lewek, M. D., Kesar, T. M., Franz, J. R., & Bowden, M. G. (2020, October 21). These legs were made for propulsion: Advancing the diagnosis and treatment of poststroke propulsion deficits. Journal of Neuroengineering and Rehabilitation, 17(1), 139.
https://doi.org/10.1186/s12984-020-00747-6
22. Awad, L. N., Reisman, D. S., Kesar, T. M., & Binder-Macleod, S. A. (2014, May). Targeting paretic propulsion to improve poststroke walking function: A preliminary study. Archives of Physical Medicine and Rehabilitation, 95(5), 840–848.
https://doi.org/10.1016/j.apmr.2013.12.012
23. Genthe, K., Schenck, C., Eicholtz, S., Zajac-Cox, L., Wolf, S., & Kesar, T. M. (2018, April). Effects of real-time gait biofeedback on paretic propulsion and gait biomechanics in individuals post-stroke. Topics in Stroke Rehabilitation, 25(3), 186–193. https://doi.org/10.1080/10749357.2018.1436384
24. Hakansson, N. A., Kesar, T., Reisman, D., Binder-Macleod, S., & Higginson, J. S. (2011, March). Effects of fast functional electrical stimulation gait training on mechanical recovery in poststroke gait. Artificial Organs, 35(3), 217–220. https://doi.org/10.1111/j.1525-1594.2011.01215.x
25. Higginson, J. S., Kesar, T., Perumal, R., & Binder-Macleod, S. A. (2007). Simulation-guided stimulation for paretic ankle muscles during stroke gait. Paper presented at the ASME Summer Bioengineering Conference, Keystone, Colorado.
26. Liu, J., Kim, H. B., Wolf, S. L., & Kesar, T. M. (2020, September). Comparison of the immediate effects of audio, visual, or audiovisual gait biofeedback on propulsive force generation in able-bodied and post-stroke individuals. Applied Psychophysiology and Biofeedback, 45(3), 211–220.
https://doi.org/10.1007/s10484-020-09464-1
27. Liu, J., Santucci, V., Eicholtz, S., & Kesar, T. M. (2021, January). Comparison of the effects of real-time propulsive force versus limb angle gait biofeedback on gait biomechanics. Gait & Posture, 83, 107–113.
https://doi.org/10.1016/j.gaitpost.2020.10.014
28. Sauder, N. R., Meyer, A. J., Allen, J. L., Ting, L. H., Kesar, T. M., & Fregly, B. J. (2019, October 1). Computational design of FastFES treatment to improve propulsive force symmetry during post-stroke gait: A feasibility study. Frontiers in Neurorobotics, 13, 80.
https://doi.org/10.3389/fnbot.2019.00080
29. Schenck, C., & Kesar, T. M. (2017, June 6). Effects of unilateral real-time biofeedback on propulsive forces during gait. Journal of Neuroengineering and Rehabilitation, 14(1), 52.
https://doi.org/10.1186/s12984-017-0252-z
30. Awad, L. N., Reisman, D. S., Pohlig, R. T., & Binder-Macleod, S. A. (2016, August). Reducing the cost of transport and increasing walking distance after stroke: A randomized controlled trial on fast locomotor training combined with functional electrical stimulation. Neurorehabilitation and Neural Repair, 30(7), 661–670.
https://doi.org/10.1177/1545968315619696
31. Awad, L. N., Reisman, D. S., Wright, T. R., Roos, M. A., & Binder-Macleod, S. A. (2014, Nov-Dec). Maximum walking speed is a key determinant of long distance walking function after stroke. Topics in Stroke Rehabilitation, 21(6), 502–509.
https://doi.org/10.1310/tsr2106-502
79
32. Balasubramanian, C. K., Bowden, M. G., Neptune, R. R., & Kautz, S. A. (2007, January). Relationship between step length asymmetry and walking performance in subjects with chronic hemiparesis. Archives of Physical Medicine and Rehabilitation, 88(1), 43–49.
https://doi.org/10.1016/j.apmr.2006.10.004
33. Bowden, M. G., Balasubramanian, C. K., Neptune, R. R., & Kautz, S. A. (2006, March). Anterior-posterior ground reaction forces as a measure of paretic leg contribution in hemiparetic walking. Stroke, 37(3), 872–876.
https://doi.org/10.1161/01.STR.0000204063.75779.8d
34. Bowden, M. G., Balasubramanian, C. K., Behrman, A. L., & Kautz, S. A. (2008, Nov-Dec). Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabilitation and Neural Repair, 22(6), 672–675.
https://doi.org/10.1177/1545968308318837
35. Brough, L. G., Kautz, S. A., Bowden, M. G., Gregory, C. M., & Neptune, R. R. (2019, January 3). Merged plantarflexor muscle activity is predictive of poor walking performance in post-stroke hemiparetic subjects. Journal of Biomechanics, 82, 361–367.
https://doi.org/10.1016/j.jbiomech.2018.11.011
36. Hsiao, H., Awad, L. N., Palmer, J. A., Higginson, J. S., & Binder-Macleod, S. A. (2016). Contribution of paretic and nonparetic limb peak propulsive forces to changes in walking speed in individuals poststroke. Neurorehabilitation and Neural Repair, 30(8), 743–752.
https://doi.org/10.1177/1545968315624780
37. Hsiao, H., Higginson, J. S., & Binder-Macleod, S. A. (2016, January 15). Baseline predictors of treatment gains in peak propulsive force in individuals poststroke. Journal of Neuroengineering and Rehabilitation, 13, 2.
https://doi.org/10.1186/s12984-016-0113-1
38. Hsiao, H., Knarr, B. A., Higginson, J. S., & Binder-Macleod, S. A. (2015, February). The relative contribution of ankle moment and trailing limb angle to propulsive force during gait. Human Movement Science, 39, 212–221.
https://doi.org/10.1016/j.humov.2014.11.008
39. Routson, R. L., Clark, D. J., Bowden, M. G., Kautz, S. A., & Neptune, R. R. (2013, July). The influence of locomotor rehabilitation on module quality and post-stroke hemiparetic walking performance. Gait & Posture, 38(3), 511–517. https://doi.org/10.1016/j.gaitpost.2013.01.020
40. Allen, J. L., Kautz, S. A., & Neptune, R. R. (2011, April). Step length asymmetry is representative of compensatory mechanisms used in post-stroke hemiparetic walking. Gait & Posture, 33(4), 538–543.
https://doi.org/10.1016/j.gaitpost.2011.01.004
41. Awad, L. N., Lewek, M. D., Kesar, T. M., Franz, J. R., & Bowden, M. G. (2020, October 21). These legs were made for propulsion: Advancing the diagnosis and treatment of poststroke propulsion deficits. Journal of Neuroengineering and Rehabilitation, 17(1), 139.
https://doi.org/10.1186/s12984-020-00747-6
42. Awad, L. N., Palmer, J. A., Pohlig, R. T., Binder-Macleod, S. A., & Reisman, D. S. (2015, June). Walking speed and step length asymmetry modify the energy cost of walking after stroke. Neurorehabilitation and Neural Repair, 29(5), 416–423.
https://doi.org/10.1177/1545968314552528
43. Jonkers, I., Delp, S., & Patten, C. (2009, January). Capacity to increase walking speed is limited by impaired hip and ankle power generation in lower functioning persons post-stroke. Gait & Posture, 29(1), 129–137.
https://doi.org/10.1016/j.gaitpost.2008.07.010
44. Rosenberg, M. C., Christianson, H., Liu, J., Santucci, V., Sims, P., Schilder, A., . . . Kesar, T. M. (2023). Fastest may not maximize gait quality: differential and individual-specific immediate effects of gait speed on biomechanical variables post-stroke. medRxiv, 2023.2008.
45. Schwartz, M. H., & Rozumalski, A. (2008, October). The Gait Deviation Index: A new comprehensive index of gait pathology. Gait & Posture, 28(3), 351–357.
https://doi.org/10.1016/j.gaitpost.2008.05.001
46. Allen, J. L., Ting, L. H., & Kesar, T. M. (2018, December 20). Gait rehabilitation using functional electrical stimulation induces changes in ankle muscle coordination in stroke survivors: A preliminary study. Frontiers in Neurology, 9, 1127.
https://doi.org/10.3389/fneur.2018.01127
47. Awad, L. N., Binder-Macleod, S. A., Pohlig, R. T., & Reisman, D. S. (2015, July). Paretic propulsion and trailing limb angle are key determinants of long-distance walking function after stroke. Neurorehabilitation and Neural Repair, 29(6), 499–508.
https://doi.org/10.1177/1545968314554625
48. Bowden, M. G., Woodbury, M. L., & Duncan, P. W. (2013, February). Promoting neuroplasticity and recovery after stroke: Future directions for rehabilitation clinical trials. Current Opinion in Neurology, 26(1), 37–42.
https://doi.org/10.1097/WCO.0b013e32835c5ba0
49. Nudo, R. J., Plautz, E. J., & Frost, S. B. (2001, August). Role of adaptive plasticity in recovery of function after damage to motor cortex. Muscle & Nerve, 24(8), 1000–1019. https://doi.org/10.1002/mus.1104
50. Yang, J. F., & Gorassini, M. (2006, October). Spinal and brain control of human walking: Implications for retraining of walking. Neuroscientist, 12(5), 379–389.
https://doi.org/10.1177/1073858406292151
51. Bernhardt, J., Borschmann, K., Boyd, L., Thomas Carmichael, S., Corbett, D., Cramer, S. C., . . . Ward, N. (2016, June). Moving rehabilitation research forward: Developing consensus statements for rehabilitation and recovery research. Int J Stroke, 11(4), 454–458.
https://doi.org/10.1177/1747493016643851
52. Dobkin, B. H. (2009, Mar-Apr). Progressive staging of pilot studies to improve phase III trials for motor interventions. Neurorehabilitation and Neural Repair, 23(3), 197–206. https://doi.org/10.1177/1545968309331863
53. Wonsetler, E. C., & Bowden, M. G. (2017, July). A systematic review of mechanisms of gait speed change post-stroke. Part 2: Exercise capacity, muscle activation, kinetics, and kinematics. Topics in Stroke Rehabilitation, 24(5), 394–403.
https://doi.org/10.1080/10749357.2017.1282413
54. Bernhardt, J., Hayward, K. S., Kwakkel, G., Ward, N. S., Wolf, S. L., Borschmann, K., . . . Cramer, S. C. (2017, July). Agreed definitions and a shared vision for new standards in stroke recovery research: The Stroke Recovery and Rehabilitation Roundtable taskforce. Int J Stroke, 12(5), 444–450.
https://doi.org/10.1177/1747493017711816
80 Delaware Journal of Public Health - August 2023
55. Burke, D., Wissel, J., & Donnan, G. A. (2013, January 15). Pathophysiology of spasticity in stroke. Neurology, 80(3, Suppl 2), S20–S26.
https://doi.org/10.1212/WNL.0b013e31827624a7
56. Dobkin, B. H. (2007, Jan-Feb). Confounders in rehabilitation trials of task-oriented training: Lessons from the designs of the EXCITE and SCILT multicenter trials. Neurorehabilitation and Neural Repair, 21(1), 3–13.
https://doi.org/10.1177/1545968306297329
57. Krakauer, J. W., Carmichael, S. T., Corbett, D., & Wittenberg, G. F. (2012, October). Getting neurorehabilitation right: What can be learned from animal models? Neurorehabilitation and Neural Repair, 26(8), 923–931.
https://doi.org/10.1177/1545968312440745
58. Robbins, S. M., Houghton, P. E., Woodbury, M. G., & Brown, J. L. (2006, June). The therapeutic effect of functional and transcutaneous electric stimulation on improving gait speed in stroke patients: A meta-analysis. Archives of Physical Medicine and Rehabilitation, 87(6), 853–859.
https://doi.org/10.1016/j.apmr.2006.02.026
59. States, R. A., Pappas, E., & Salem, Y. (2009, July 8). Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst Rev, 2009(3), CD006075.
https://pubmed.ncbi.nlm.nih.gov/19588381
60. Birkenmeier, R. L., Prager, E. M., & Lang, C. E. (2010, September). Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: A proof-of-concept study. Neurorehabilitation and Neural Repair, 24(7), 620–635.
https://doi.org/10.1177/1545968310361957
61. Kleim, J. A., & Jones, T. A. (2008, February). Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. J Speech Lang Hear Res, 51(1), S225–S239.
https://doi.org/10.1044/1092-4388(2008/018)
62. Lang, C. E., Macdonald, J. R., Reisman, D. S., Boyd, L., Jacobson Kimberley, T., Schindler-Ivens, S. M., . . . Scheets, P. L. (2009, October). Observation of amounts of movement practice provided during stroke rehabilitation. Archives of Physical Medicine and Rehabilitation, 90(10), 1692–1698.
https://doi.org/10.1016/j.apmr.2009.04.005
63. Wittenberg, G. F. (2009, October). Neural plasticity and treatment across the lifespan for motor deficits in cerebral palsy. Developmental Medicine and Child Neurology, 51(Suppl 4), 130–133.
https://doi.org/10.1111/j.1469-8749.2009.03425.x
64. Zeiler, S. R., & Krakauer, J. W. (2013, December). The interaction between training and plasticity in the poststroke brain. Current Opinion in Neurology, 26(6), 609–616.
https://doi.org/10.1097/WCO.0000000000000025
65. Cramer, S. C., Sur, M., Dobkin, B. H., O’Brien, C., Sanger, T. D., Trojanowski, J. Q., . . . Vinogradov, S. (2011, June). Harnessing neuroplasticity for clinical applications. Brain, 134(6), 1591–1609.
https://doi.org/10.1093/brain/awr039
66. Stinear, C. M. (2017, October). Prediction of motor recovery after stroke: Advances in biomarkers. Lancet Neurol, 16(10), 826–836.
https://doi.org/10.1016/S1474-4422(17)30283-1
67. Chieffo, R., Comi, G., & Leocani, L. (2016, January). Noninvasive neuromodulation in poststroke gait disorders: Rationale, feasibility, and state of the art. Neurorehabilitation and Neural Repair, 30(1), 71–82.
https://doi.org/10.1177/1545968315586464
68. Laffont, I., Bakhti, K., Coroian, F., van Dokkum, L., Mottet, D., Schweighofer, N., & Froger, J. (2014, November). Innovative technologies applied to sensorimotor rehabilitation after stroke. Annals of Physical and Rehabilitation Medicine, 57(8), 543–551.
https://doi.org/10.1016/j.rehab.2014.08.007
69. Madhavan, S., & Stinear, J. W. (2010, January). Focal and bi-directional modulation of lower limb motor cortex using anodal transcranial direct current stimulation. Brain Stimulation, 3(1), 42.
https://doi.org/10.1016/j.brs.2009.06.005
70. Chaulk, C. P., & Kazandjian, V. A. (2004, September). Moving beyond randomized controlled trials. American Journal of Public Health, 94(9), 1476.
https://doi.org/10.2105/AJPH.94.9.1476
71. Li, S., & Francisco, G. E. (2015, April 10). New insights into the pathophysiology of post-stroke spasticity. Frontiers in Human Neuroscience, 9, 192.
https://doi.org/10.3389/fnhum.2015.00192
72. Naro, A., Leo, A., Russo, M., Casella, C., Buda, A., Crespantini, A., . . . Calabrò, R. S. (2017, May). Breakthroughs in the spasticity management: Are non-pharmacological treatments the future? J Clin Neurosci, 39, 16–27.
https://doi.org/10.1016/j.jocn.2017.02.044
73. Trompetto, C., Marinelli, L., Mori, L., Pelosin, E., Currà, A., Molfetta, L., & Abbruzzese, G. (2014). Pathophysiology of spasticity: Implications for neurorehabilitation. BioMed Research International, 2014, 354906.
https://doi.org/10.1155/2014/354906
74. Levin, M. F., & Hui-Chan, C. (1993, February). Are H and stretch reflexes in hemiparesis reproducible and correlated with spasticity? Journal of Neurology, 240(2), 63–71.
https://doi.org/10.1007/BF00858718
75. Madhavan, S., Stinear, J. W., & Kanekar, N. (2016). Effects of a single session of high intensity interval treadmill training on corticomotor excitability following stroke: Implications for therapy. Neural Plasticity, 2016, 1686414.
https://doi.org/10.1155/2016/1686414
76. Yen, C. L., Wang, R. Y., Liao, K. K., Huang, C. C., & Yang, Y. R. (2008, Jan-Feb). Gait training induced change in corticomotor excitability in patients with chronic stroke. Neurorehabilitation and Neural Repair, 22(1), 22–30.
https://doi.org/10.1177/1545968307301875
77. Hsiao, H., Knarr, B. A., Higginson, J. S., & Binder-Macleod, S. A. (2015, April 18). Mechanisms to increase propulsive force for individuals poststroke. Journal of Neuroengineering and Rehabilitation, 12, 40.
https://doi.org/10.1186/s12984-015-0030-8
81
Artificial Intelligence and the Evaluation and Treatment of Stroke
Lee P. Dresser, M.D. General Neurologist, Wilmington Neurology Consultants; Chair, Delaware Stroke Initiative
Michael Anders Kohn, M.D., M.P.P. Professor, Epidemiology and Biostatistics, University of California San Francisco
ABSTRACT
Stroke affects close to 800,000 Americans every year and is a major cause of disability and mortality. Prompt, accurate diagnosis and treatment of stroke is of critical importance in minimizing these deleterious effects. Recent advances in computer technology have allowed the development artificial intelligence technology that can be applied to the diagnosis, treatment and rehabilitation of victims of stroke.
INTRODUCTION
In 2021, more than 795,000 people in the United States suffered a stroke. About 610,000 (77%) of those were first time strokes. The annual stroke related costs were nearly $56.5 billion, and this included the costs of health care services, medicine and missed days of work. Stroke is a leading cause of disability and reduced mobility.1 Over the past decade, improvements in technology have enabled the application of artificial intelligence (AI) in medicine and specifically to the evaluation and treatment of stroke.
Computer technology has long been applied in medicine but originally was quite limited by slow speeds and high costs. In the 1950s computers were large and slow. The IBM Model 350 Disk File had a storage capacity of only 5 megabytes. In 1980 IBM introduced Model 3380 with a hard drive size of more than 1 gigabyte, but it was the size of a refrigerator, weighed 550 pounds and cost $100,000. Since then the speed of computers has increased exponentially (Figure 1) and the prices have markedly decreased.2
AI is a generic term that refers to the simulation of thought processes by computer systems, enabling them to perform tasks that typically require human intelligence, such as understanding natural language, recognizing patterns, solving problems, and making decisions. While AI has not achieved human intelligence (at least, not yet), the capacity to learn from data increases the amount and sophistication of tasks that can be tackled by machine learning systems.3 Currently we are exposed to AI daily when using virtual assistants such as Siri and Alexa, speech and image recognition on our smartphones, and personalized recommendations on streaming platforms.4
Machine learning (ML) is a subfield of AI that consists of a set of algorithms that use data to make predictions or decisions without being explicitly programmed. There are three primary subdivisions of ML: supervised learning, unsupervised learning, and reinforcement learning.5,6
SUPERVISED LEARNING
Supervised learning starts with labelled “training” data and predicts labels for new “test” data.
Algorithms
Regression methods including LASSO (Least Absolute Shrinkage and Selection Operator), Classification Trees, Random Forests, Gradient Boosting algorithms (like XGBoost and LightGBM), Support Vector Machines, and Artificial Neural Networks (more on this below).

Example
In an algorithm to distinguish spam emails from non-spam (ham) emails, a large number of emails, both spam and ham, are analyzed for different features, such as keywords and presence of exclamation marks. These features are input variables and the label of the email, spam or ham, is the target variable. Seventy to eighty percent of the emails are used as the training set. A supervised learning algorithm, such as logistic regression, is fed the training data. The algorithm learns the patterns and relationships between the input features and the target variable (spam/ham) during the training process. Once the model is trained, the remaining 20-30% of the emails, the test data, is provided to the model. If the predicted labels are close in accuracy to the actual labels in the test set, then the model can be used to make spam versus ham predictions on new, unseen emails.
82 Delaware Journal of Public Health - August 2023 Doi: 10.32481/djph.2023.08.014
Figure 1. Advances in Computer Speed Over Time
UNSUPERVISED LEARNING
Unsupervised learning starts with unlabeled training data and identifies patterns and clusters.
Algorithms
K-means Clustering and Principal Component Analysis (PCA)
Example
Analyzing customers of an online store to help tailor marketing campaigns. The customers do not have any specific labels, but the clustering algorithm would help assign them to certain clusters or labels based on known data about the customers. Then marketing campaigns could be devised to target the specific characteristics of each cluster (label).
REINFORCEMENT LEARNING
Reinforcement learning is learning from experience. An agent communicates with its environment, and is given a reward function that it tries to optimize. The purpose of the agent is to understand the effect of its decisions and discover the best strategies for maximizing its rewards during the training and learning procedure.
Algorithms
Q-Learning, State-Action-Reward-State-Action (SARSA) and Deep Q Networks (DQNs)Algorithms: Q-Learning, SARSA (StateAction-Reward-State-Action), and Deep Q Networks (DQNs).
Example
Training a robot in a maze to find the exit as quickly as possible. Rewards and penalties are assigned to guide the robot’s behavior. Each time the robot takes a step closer to the exit, it receives a positive reward. If the robot hits a wall, it receives a negative penalty. Reaching the exit gives the robot the highest positive reward. Through trial and error, the robot (agent) learns to associate actions with higher rewards and, over time, converges on an optimal policy to solve the maze navigation problem.3
DEEP LEARNING
Deep Learning (DL) is relatively new type of supervised learning that deserves special mention. It attempts to replicate the workings of the human brain by using artificial neural networks (ANN). DL employs a range of algorithms that use neural-type networks with many (i.e., deep) layers. It is a sophisticated approach to building intelligent systems that can learn and make decisions based on a vast amount of data. DL enables the system to perform complex tasks such as image recognition. This has been utilized for the analysis of computerized tomography (CT) and magnetic resonance imaging (MRI) to help quickly and accurately detect abnormalities, such as acute cerebral ischemia or hemorrhage.3,6,7 ANNs are composed of multiple connected nodes or “neurons.” A typical network consists of an input layer connected to hidden layers which are eventually connected to an output layer (Figure 2). The hidden layers covertly process information between the input and output layers. This is analogous to the human visual system instantly recognizing three lines forming a triangle. We are not consciously aware of the mental processing involved with recognizing three lines (input) as a triangle (output).7 Object recognition software such as that employed in self-driving cars to detect pedestrians and obstacles may use upwards of 150 hidden (deep) layers.7

RADIOLOGY
The management of stroke is highly dependent on the interpretation of imaging studies. Automated imaging analysis could greatly speed up CT and MRI interpretation.
DL methods of image analysis could also be valuable in areas where neuroradiologists are not immediately available. CT perfusion is utilized in acute cerebral infarctions to detect brain tissue at risk and to help clinicians decide which patients are good candidates for thrombolytic and neuro-interventional therapy, such as mechanically extracting blood clots from large cerebral vessels. ANNs can be used to “de-noise” perfusion images to give clearer pictures. They can also reduce radiation dose for CT scans.6 Amazingly, DL methods do not require a priori assumptions of what image features are important. The network can learn on its own to identify them.
AI is well suited to be employed in radiology since it excels in image analysis. Radiology has an established digital workflow that makes it easy to integrate AI. It can rapidly detect and flag intracranial hemorrhage and large vessel occlusion. This could expedite the decision to use thrombolytic or neuro-interventional therapy for the acute treatment of cerebral ischemia.
In ANN the term “weights” represents the strength of the connection between the two nodes it connects. The sizes of networks used to interpret data is staggering. AI models consisting of networks with billions of weights can train on a large amount of data. These models can evaluate clinical data and radiographic data to generate suggestions for therapy, follow up and additional testing.7
83
Figure 2. Model of an Artificial Neural Network
Input Layer
Hidden Layer
Output Layer
OUTCOMES
By analyzing and combining clinical, laboratory, and imaging information, AI can give individualized recommendations for the best therapy to treat stroke and provide prognostic information for functional outcomes. This technology is also being used to assist with stroke rehabilitation. Robotic devices using AI can analyze a patient’s movement patterns and provide guidance to help improve motor and gait function. It likely also can assist in developing programs to help with the treatment of speech, language and vision problems.8 By analyzing clinical and imaging data, AI may also be able to predict which patients will suffer from depression and cognitive dysfunction after strokes.8
Dysphagia is a common complication of stroke. This can lead to malnutrition, pneumonia and possibly death. Videofluoroscopic swallow studies (VFSS) are the standard tool to evaluate swallowing function after stroke. Researchers have employed AI to evaluate the VFSS images of 190 stroke patients.9 The model developed was very accurate in distinguishing normal swallowing, penetration of swallowed food and liquid into the upper airway, and frank aspiration. It is emphasized that using a high-quality dataset is a prerequisite for obtaining excellent learning and analysis results when using image data.6 The old adage regarding computers of “garbage in, garbage out” is equally applicable to AI.
LIMITATIONS
Besides the necessity for high quality data, there are some other limiting factors to the use of AI in stroke. It is not clear for many of the machine learning algorithms how and why a decision has been cast. This is particularly true of the most popular deep neural network approaches currently in use. This is termed the “black box problem.” Concern regarding this opacity has lead the governments of the United States and United Kingdom, as well as the European Union, to call for measures to make AI intelligible.3 Confidence in AI systems can be hindered by this lack of transparency. Also, if models are not updated to reflect factors such as changes in disease prevalence, their accuracy can decrease.6
Despite these limitations, AI holds tremendous potential to assist medical professionals in the care of stroke patients. It likely will become progressively more accurate in the diagnosis and evaluation of stroke and its sequelae. It therefore will become increasingly more helpful in assisting with optimizing treatment and rehabilitation to limit damage to the brain and help stroke patients recover faster and more completely. Dr. Dresser may be contacted at lpdresser@gmail.com
REFERENCES
1. Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., . . . Martin, S. S., & the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2023, February 21). Heart disease and stroke statistics—2023 update: A report from the American Heart Association. Circulation, 147(8), e93–e621. https://doi.org/10.1161/CIR.0000000000001123
2 Haug, C. J., & Drazen, J. M. (2023, March 30). artificial intelligence and machine learning in clinical medicine, 2023. The New England Journal of Medicine, 388(13), 1201–1208. https://doi.org/10.1056/NEJMra2302038
3. Yang, G., Ye, Q., & Xia, J. (2022, January). Unbox the blackbox for the medical explainable AI via multi-modal and multi-centre data fusion: A mini-review, two showcases and beyond. Inf Fusion, 77, 29–52 https://doi.org/10.1016/j.inffus.2021.07.016
4 Cohen, F. (2023, May). The role of artificial intelligence in headache medicine: Potential and peril. Headache, 63(5), 694–696
https://doi.org/10.1111/head.14495
5 Theobald, O. (2021). Machine Learning for Absolute Beginners: A Plain English Introduction (Third Edition).
6 Rajpurkar, P., & Lungren, M. P. (2023, May 25). The current and future state of ai interpretation of medical images. The New England Journal of Medicine, 388(21), 1981–1990. https://doi.org/10.1056/NEJMra2301725
7. Mouridsen, K., Thurner, P., & Zaharchuk, G. (2020, August). Artificial intelligence applications in stroke. Stroke, 51(8), 2573–2579.
https://doi.org/10.1161/STROKEAHA.119.027479
8. Choo, Y. J., & Chang, M. C. (2022, October 31). Use of machine learning in stroke rehabilitation: A narrative review. Brain & Neurorehabilitation, 15(3), e26
https://doi.org/10.12786/bn.2022.15.e26
9 Kim, J. K., Choo, Y. J., Choi, G. S., Shin, H., Chang, M. C., & Park, D. (2022, February 14). Deep learning analysis to automatically detect the presence of penetration or aspiration in videofluoroscopic swallowing study. Journal of Korean Medical Science, 37(6), e42.
https://doi.org/10.3346/jkms.2022.37.e42
84 Delaware Journal of Public Health - August 2023
Interest-Free Student Loans
Interest-Free Student Loans
Attention Delaware residents pursuing careers in the health care field at Delaware institutions! Unlock your potential with the Delaware Academy of Medicine's Student Financial Aid Program!
Attention Delaware residents pursuing careers in the health care field at Delaware institutions! Unlock your potential with the Delaware Academy of Medicine’s Student Financial Aid Program!
Are you passionate about nursing, physician assistant, behavioral health, dental, medical assistant, or other heath care positions? The Delaware Academy of Medicine's Student Financial Aid program is here to support your dreams and make your education more affordable than ever before. With a small commitment to work in Delaware after graduation, we are offering interest-free student loans ranging from $2,500 to $15,000. Funds are available until they are depleted, so apply now!
Are you passionate about nursing, physician assistant, behavioral health, dental, medical assistant, or other heath care positions?
The Delaware Academy of Medicine’s Student Financial Aid program is here to support your dreams and make your education more affordable than ever before. With a small commitment to work in Delaware after graduation, we are offering interest-free student loans ranging from $2,500 to $15,000. Funds are available until they are depleted, so apply now!
85
Acute Cerebral Ischemia
A common mechanism of acute brain injury that results from impaired blood ow to the brain.
Ambulatory
Medical care provided on an out-patient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services.
Atherosclerosis
A disease of the arteries characterized by the deposition of plaques of fatty material on their inner walls.
Atrial Fibrillation
A type of cardiac arrhythmia characterized by irregular and o en rapid electrical activity in the atria (upper chamber) of the heart.
Cardioembolic Stroke
When the heart pumps materials like debris or a blood clot into the brain, resulting in the blockage of blood vessels
Carotid Stenosis
A narrowing of the blood vessels in the neck that carry blood from the heart to the brain.
Coagulopathy
A bleeding disorder in which the blood’s ability to coagulate (form clots) is a ected: hypercoagulopathy will clot more than normal; hypocoagulopathy will clot less than normal.
Contraindication
A condition or circumstance that indicates a particular technique or medication should not be used.
Electrocardiogram (EKG)
A line graph that shows changes in the electrical activity of the heart over time.
Etiology
e cause, set of causes, or manner of causation of a disease or condition.
Hemiplegia
One-sided muscle paralysis or weakness, usually a symptom of a brain-related cause or condition.
Hemorrhagic Stroke
A stroke due to a ruptured blood vessel that bleeds into the surrounding brain.
Hyperlipidemia
An abnormally high concentration of fats or lipids in the blood.
Hypertension
High blood pressure
Hypoglycemia
Low blood sugar
Hypotension
Low blood pressure
Hypovolemia
Low blood volume
Intracranial Hemorrhage
Any bleeding within the intracranial vault (skull), including the brain parenchyma and surrounding spaces.
LEXICON
86 Delaware Journal of Public Health - August 2023
Ischemic Stroke
A stroke when the blood supply to a part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients.
Normal Time/Well Time
e amount of time that has passed since a stroke patient was last seen as “normal” or “well.”
NPO
None per os, no food by mouth.
Number Needed to Treat (NNT)
e number of patients that need to be treated to prevent one additional bad outcome.
Occlusion
e blockage or closing of an opening, blood vessel, or hollow organ.
Odds Ratio
A measure of association between an exposure and an outcome. e odds that an outcome will occur given a particular exposure, compared to the odds of the outcome occurring in the absence of that exposure.
Parenchyma
e functional tissue of an organ.
Penumbra
e area surrounding an ischemic event; the reversibly injured brain tissue around the location of a stroke.
Perfusion
e passage of blood or other uid through the blood vessels or other natural channels in an organ or tissue
Postictal
e period that begins when a seizure subsides and ends when the patient returns to baseline.
Reperfusion
Restoring the ow of blood to an organ or tissue, typically a er a heart attack or stroke.
Risk Ratio
Compares the risk of a health event (disease, injury, risk factor, or death) among one group with the risk among another group.
Thrombectomy
Surgery to remove a thrombus (blood clot) from a blood vessel.
Thrombolysis/Thrombolytic
e treatment of and medicines used to dissolve blood clots within the body.
Thrombocytopenia
A de ciency of platelets in the blood, which can lead to bleeding in the tissues, bruising, and slow blood clotting a er an injury.
Transient Ischemic Attack
A brief episode of neurological dysfunction resulting from an interruption in the blood supply to the brain or the eye, sometimes a precursor of a stroke.
LEXICON
87
RESOURCES
American Heart Association
Acute Ischemic Stroke Healthcare Professional Resources:
https://www.stroke.org/en/professionals/stroke-resource-library/acute-ischemicstroke-healthcare-professional-resource-page
Prehospital/EMS Checklist:
https://www.heart.org/en/professional/quality-improvement/mission-lifeline/mission-lifeline-stroke
American Stroke Association
Resource Library:
https://www.stroke.org/en/professionals/strokeresource-library
Delaware Stroke Resources
Delaware Stroke Resources:
http://delawarestrokeresources.org/
University of Delaware Clinical Stroke Studies:
https://www.udel.edu/academics/colleges/chs/departments/pt/research/research-studies/stroke-studies/
National Institutes of Health
Stroke Scale:
https://www.ninds.nih.gov/health-information/public-education/know-stroke/health-professionals/nih-stroke-scale
National Transition of Care Checklist
https://static1.squarespace.com/static/5d48b6eb75823b00016db708/t/5d49bc833b48f80001f15 4bc/1565113475856/TOC_Checklist.pdf
Nurse Certification
Registered Neuroscience Nurse:
https://abnncertification.org/cnrn/about
Registered Rehabilitation Nurse:
https://rehabnurse.org/crrncertification/crrn-certification
Stroke Certified Registered Nurse:
https://abnncertification.org/scrn/about
Preparedness Assessment for Transition Home After Stroke:
https://www.rehabnurse.org/pathtool
World Stroke Organization:
https://www.world-stroke.org/professional
88 Delaware Journal of Public Health - August 2023
RESOURCES
Guidelines
AHA Guidelines:
https://professional.heart.org/en/guidelines-and-statements/guidelines-and-statements-search
2021 Nursing Care of Patients with Acute Ischemic Stroke
Prehospital and Acute Phase:
https://www.ahajournals.org/doi/10.1161/STR.0000000000000356
Endovascular/Intensive Care:
https://www.ahajournals.org/doi/10.1161/STR.0000000000000358
Post hyperacute and Prehospital Discharge:
https://www.ahajournals.org/doi/10.1161/STR.0000000000000357
2019 Acute Ischemic Stroke Guidelines:
https://www.ahajournals.org/doi/10.1161/STR.0000000000000211
2017 Treatment and Outcome of Hemorrhagic Transformation after Intravenous Alteplase in Acute Ischemic Stroke:
https://www.ahajournals.org/doi/full/10.1161/str.0000000000000152
2015 Guidelines for the Management of Spontaneous Intracerebral Hemorrhage:
https://www.ahajournals.org/doi/10.1161/str.0000000000000069
2015 Guidelines for the Management of Patients with Unruptured Intracranial Aneurysms:
https://www.ahajournals.org/doi/full/10.1161/str.0000000000000070
2012 Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage:
https://www.ahajournals.org/doi/full/10.1161/str.0b013e3182587839
2016 Guidelines for Adult Stroke Rehabilitation and Recovery:
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000098
89
The Nation Needs to Invest in Public Health Now
Timothy E. Gibbs, M.P.H. Executive Director, Delaware Academy of Medicine / Delaware Public Health Association
Katherine Smith, M.D., M.P.H. Program Director, Delaware Academy of Medicine / Delaware Public Health Association
Every day in communities across the nation, our public health system and public health workforce are striving to help everyone get and stay healthy. Our public health workforce has worked overtime during the COVID-19 pandemic to protect our communities, and while we are grateful for the temporary emergency funding provided by Congress to help state and local health departments, we know that we must ensure our public health system and workforce have adequate funding: we must be prepared for the next public health emergency.
Over the last decade, federal funding for public health programs and agencies has fallen. In fiscal year 2021, only 4.4% of federal health spending went toward public health.
Federal spending makes a big difference. In addition to ensuring state and local health departments have funding to address public health emergencies like COVID-19, federal funding for public health goes toward solving community problems like preventing childhood lead poisoning, reducing maternal and infant mortality, curbing tobacco use, and lowering obesity rates.
According to the American Public Health Association’s Speak for Health data sheets, Delaware receives $111 per person in funding from the Centers for Disease Control and Prevention (CDC) and the Health Resources Services Administration (HRSA), ranking the state 17th in the nation. The Prevention and Public Health Fund awarded Delaware $7.28 million in grants for community and clinical prevention efforts, and improvements to public health infrastructure in the 2020 fiscal year. Since then, significant additional funding has come to Delaware through the American Rescue Plan Act (ARPA), the CDC, and the Health Resources and Services Administration (HRSA).
Robust funding for the public health system is essential to protecting the health of our communities, saving lives, and reducing costs in the health care system. The future of our nation’s health depends on a strong and properly equipped public health infrastructure at the community level — in Delaware, and in cities and towns across the country.
As the leading voice for public health in our country, the American Public Health Association has sounded the alarm on inadequate public health funding. If we fail to act now and truly invest in public health, our communities will suffer. Congress must increase annual funding for key public health agencies like the CDC, HRSA and the National Institutes of Health (NIH), and maintain existing and future funding available through the Prevention and Public Health Fund. Every dollar invested today will go toward the future of our country’s health.
We support efforts to provide sustained and long-term additional annual funding for the CDC—as well as state, local, tribal, and territorial core public health infrastructure—to modernize the nation’s public health system, rebuild the workforce and promote healthier communities. In the Senate, Senator Patty Murray has introduced the Public Health Infrastructure Saves Lives Act, which would establish a program to annually fund public health infrastructure. We urge Congress to include this important legislation in the infrastructure legislation that is currently being developed.
It is time our nation’s health is made a priority. For our Delaware delegation in Washington, DC, the message is clear: your continued commitment to increasing investments in public health is fundamental to our pursuit of becoming a healthy nation.
Mr. Gibbs may be contacted at tgibbs@delamed.org Dr. Smith may be contacted at ksmith@delamed.org.
Doi: 10.32481/djph.2023.08.015
90 Delaware Journal of Public Health - August 2023
Index of Advertisers The Nation's Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 American Public Health Association Immunization Summit 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 Immunization Coalition of Delaware The DPH Bulletin - July 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27 Delaware Division of Public Health Delaware Stroke Summit . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33 Beebe Healthcare The DPH Bulletin - August 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42 Delaware Division of Public Health Be A Stroke Hero . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 75 American Stroke Association Submission Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 92 Delaware Journal of Public Health 91
Public Health
Delaware Journal of Submission Guidelines
updated August, 2023
About the Journal
Established in 2015, The Delaware Journal of Public Health is a peer-reviewed electronic publication created by the Delaware Academy of Medicine/Delaware Public Health Association. The publication acts as a repository of news for the medical, dental, and public health communities, and is comprised of upcoming event announcements, past conference synopses, local resources, peer-reviewed content ranging from manuscripts and research papers to opinion editorials and personal interest pieces, relating to the public health sector. Each issue is largely devoted to an overarching theme or current issue in public health.
The content in the DJPH is informed by the interest of our readers and contributors. If you have an event coming up, would like to contribute an Op-Ed, would like to share a job posting, or have a topic in public health you would like to see covered in an upcoming issue, please let us know.
If you are interested in submitting an article to the Delaware Journal of Public Health, or have any additional inquiries regarding the publication, please contact the managing editor at managingeditor@djph.org, or the publisher at tgibbs@delamed.org.
Information for Authors Submission Requirements
The DJPH accepts a wide variety of submission formats, including brief essays, opinion editorials pieces, research articles and findings, analytic essays, news pieces, historical pieces, images, advertisements pertaining to relevant, upcoming public health events, and presentation reviews. Additional types of submission not previously mentioned may be eligible, please contact a staff member for more information.
The initial submission should be clean and complete, without edits or markups, and contain both the title and author(s) full name(s). Submissions should be 1.5 or double spaced with a font size of 12. Once completed, articles should be submitted via the submission page at https://djph.org/submissions/submit-an-article/ Graphics, images, info-graphics, tables, and charts are welcome and encouraged to be included in articles. Please ensure that all pieces
are in their final format, and all edits and track changes have been implemented prior to submission. To view additional information for online submission requirements, please refer to the DJPH website: https://djph.org/submissions/submit-an-article/.
Trial registration information is required for all clinical trials and must be included in the final article and/or abstract.
Abstracts
Authors must submit a structured or unstructured abstract along with their article. Abstracts will have a maximum of 200 words, including headings. Structured abstracts should employ 4-5 headings, and may include Objectives, Methods, Results, and Conclusions. A fifth heading, Policy Implications, may be used if relevant to the article. All abstracts should provide the date(s) and location(s) of the study if applicable, as well as any trial registration information.
92 Delaware Journal of Public Health - August 2023
Submission Length
While there is no prescribed word length, full articles will generally be in the 2,500-4,000word range, and editorials or brief reports will be in the 1,500-2,500-word range. If there are any questions regarding the length of a submission or APA guidelines, please contact a staff member.

Copyright
The journal and its content is copyrighted by the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA). The contents are licensed under Creative Commons License – CC BY-NC-ND (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Images are NOT covered under the Creative Commons license and are the property of the original photographer or company who supplied the image.
Opinions expressed by authors of articles summarized, quoted, or published in full within the DJPH represent only the opinions of those authors and do not necessarily reflect the official policy of the Academy/DPHA, the DJPH, or the institution with which the authors are affiliated.
Conflicts of Interest
Any conflicts of interest, including political, financial, personal, or academic conflicts, must be declared prior to the submission of the article, or in conjunction with a submission. Conflicts of interest are any competing interests that may leave readers feeling misled or deceived, and/or alter their perception of subject matter. Declared conflicts of interest will be published alongside articles in the final publication.
Nondiscriminatory Language
Use of nondiscriminatory language is required in all DJPH submissions. The DJPH reserves the right to reject any submission found to be using sexist, racist, or heterosexist language, as well as unethical or defamatory statements.
93
Delaware Academy of Medicine / DPHA
P.O. Box 89 Historic New Castle, DE 19720 ISSN
www.dela med.org | www.djph.org
e Del aware Academy of Medicine is a private , nonprofit organization founded in 1930. O ur mission is to enhance the well being of our communit y through medical education an d the promotion of public health. O ur educational initiatives span the spect rum f rom consumer health education tocontinuing medical education conferences and symposia e Del aware Public Health A ssociation wa s officially rebor n at the 141 st Annual Meeting of the American Public He alth A ssociation (AHPA) hel d in B oston, M A in November, 2013. At this meeting, af filiation of t he DPH A wa s t ransferred to the Del aware Academy of Medicine officially on November 5, 2013 by action of the A PH A Governing Council . e Del aware Academy of Me dicine, who’s mission statement is “ to promote the well-being of o ur communit y through education and the promotion of public health,” is honored to take on t his responsibility in the First State
Follow Us: 2639-6378