


www.delamed.org | www.djph.org Volume 9 | Issue 2 June 2023 A publication of the Delaware Academy of Medicine / Delaware Public Health Association
Delaware Journal of
Public Health
Delaware Academy of Medicine
OFFICERS
S. John Swanson, M.D. President Killingsworth
Lynn Jones, FACHE
President-Elect
Professor Rita Landgraf (Co-Chair) Vice President
Jeffrey M. Cole, D.D.S., M.B.A. Treasurer
Stephen C. Eppes, M.D. Secretary
Omar A. Khan, M.D., M.H.S. (Co-Chair) Immediate Past President
Timothy E. Gibbs, M.P.H. Executive Director, Ex-officio
DIRECTORS
David M. Bercaw, M.D.
Lee P. Dresser, M.D.
Eric T. Johnson, M.D.
Erin M. Kavanaugh, M.D.
Joseph Kelly, D.D.S.
Joseph F. Kestner, Jr., M.D.
Brian W. Little, M.D., Ph.D.
Arun V. Malhotra, M.D.
Daniel J. Meara, M.D., D.M.D.
Ann Painter, M.S.N., R.N.
John P. Piper, M.D.
Charmaine Wright, M.D., M.S.H.P. EMERITUS
Robert B. Flinn, M.D.
Barry S. Kayne, D.D.S.
Delaware Public Health Association
Advisory Council:
Omar Khan, M.D., M.H.S. Chair
Timothy E. Gibbs, M.P.H. Executive Director
Louis E. Bartoshesky, M.D., M.P.H.
Gerard Gallucci, M.D., M.H.S.
Melissa K. Melby, Ph.D.
Mia A. Papas, Ph.D.
Karyl T. Rattay, M.D., M.S.
William J. Swiatek, M.A., A.I.C.P.
Delaware Journal of Public Health
Timothy E. Gibbs, M.P.H.
Publisher
Omar Khan, M.D., M.H.S. Editor-in-Chief
Stephen Metraux, Ph.D., Roger Hesketh, Sean O’Neill, M.C.P., Mimi Rayl, M.R.P.
Guest Editors
Liz Healy, M.P.H.
Managing Editor
Kate Smith, M.D., M.P.H.
Copy Editor
Suzanne Fields
Image Director
Public Health Delaware Journal of
A publication of the Delaware Academy of Medicine / Delaware Public Health Association
3 | In This Issue
Omar A. Khan, M.D., M.H.S.; Timothy E. Gibbs, M.P.H.
4 | Guest Editor
StephenMetraux,Ph.D.;RogerHesketh;SeanO’Neill, M.C.P.; MimiRayl,M.R.P
6|HomelessnessInDelaware:AnAssessment
StephenMetraux,Ph.D.;StevenW.Peuquet,Ph.D.
14|DemographicsofthePopulationExperiencing Homelessness and Receiving Publicly Funded Substance Use and Mental Health Treatment Services in Delaware
David Borton, M.A.; Rachel Ryding, Ph.D.; Meisje J. Scales, M.P.H., C.P.S.; Kris Fraser, M.P.H., P.M.P.
18 | Health & Housing in Delaware: Matching Medicaid Claims and Encounters and the Community Management Information System databases
Erin Nescott, M.S.; Stephen Metraux, Ph.D.; Mary Joan McDuffie, M.A.; Elizabeth Brown, MD, M.S.H.P.
24 | Evaluating Approaches to Linking Evictions Records: Assessing the Feasibility of Research with Integrated Data
J. J. Cutuli, Ph.D.; Mary Joan McDuffie, M.A.; Erin Nescott, M.S.
30 | Housing in Delaware for the Intellectual and Developmental Disabilities Population
Jody A. Roberts, Ph.D.; Ankita Mohan
34 | Homelessness Among Persons on Delaware’s Sex Offender Registry
Stephen Metraux, Ph.D.; Alexander C. Modeas, M.A.
44 | An Overview of Poverty in Delaware
Erin Nescott, M.S., Janice Barlow, M.P.A.; Miranda Perez-Rivera
50 | Considering the Benefits Cliff Embedded in the Relationship between Housing and Health

Dorothy Dillard, Ph.D.; Bianca Mers, M.C.R.P.
54 | Gauging and Responding to the Need for Home Repair Assistance in Delaware
Katharine Millard, M.S.P.P.M.; Stephen Metraux, Ph.D.
60 | The Perilous Intersection of Housing Precarity and Climate Change in Delaware
Victor W. Perez, Ph.D.; William Swiatek, M.A., A.I.C.P
62 | Global Health Matters
Fogarty International Center
74 | Solving Homelessness in Delaware Requires Resolving the Disparities That Cause It
Sequoia Rent, B.A.
80 | LGBTQ+ Youth Homelessness in Delaware: Building a Case for Targeted Surveillance and Assessment of LGBTQ+ Youth Needs and Experiences
Mary Louise Mitsdarffer, Ph.D., M.P.H.; Rebecca McColl, M.A.; Erin Nescott, M.S.; Jim Bianchetta; Eric K. Layland, Ph.D.; Tibor Tóth, Ph.D.
88 | Delaware’s Domestic Violence Housing Crisis
Monica Beard, D.Phil., Esq.
94 | Providing a Home for Good
Eugene R. Young, Jr.
96 | Homelessness, Housing and Health: The Secrets ALICE Will Not Tell You
Michelle A. Taylor, Ed.D.
100 | Fire on My Tongue
Michael Kalmbach, M.F.A.
102 | Sunday Breakfast Mission: A Christian Non-Medical Model Toward Addiction Homelessness Rehabilitation
Reverend Tom Laymon
104 | Housing, Poverty, and Health Outcomes
Kim Blanch, R.N., B.S.N..
110 | A Vision for Community, Connection and Reinvestment
Amanda August, M.A
116 | Leveraging Delaware’s Public Health Resources to Mitigate Spread of Communicable Diseases in Congregate Settings
Laura A. Strmel, M.P.A.; Diane Hainsworth, B.S.N./B.A; Muriel Gillespie; Sydney Kappers, B.S.; Mollee Dworkin, M.S.
122 | Social Capital from Online Social Media is Associated with Visiting a Healthcare Practitioner at Least Once a Year Among College Students
Joshua Fogel, Ph.D.; Ashaney Ewen, B.S., B.B.A.
130 | Ensuring Access to Opioid Treatment Program Services Among Delawareans Vulnerable to Flooding
Jennifer A. Horney, Ph.D., M.P.H.; Sarah Elizabeth Scales, M.P.H.; Urkarsh Gangwal; Shangjia Dong, Ph.D.
134 | Postpartum Contraceptive Use, Pregnancy Intentions in Women With and Without a Delivery of a NAS-Affected Infant in Delaware, 2012-2018
Khaleel Hussaini, Ph.D.; George Yocher, M.S.
142 | Lexicon & Resources
144 | Index of Advertisers
The Delaware Journal of Public Health (DJPH), first published in 2015, is the official journal of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA).

Submissions: Contributions of original unpublished research, social science analysis, scholarly essays, critical commentaries, departments, and letters to the editor are welcome. Questions?
Write ehealy@delamed.org or call Liz Healy at 302-733-3989
Advertising: Please write to ehealy@delamed.org or call 302-733-3989 for other advertising opportunities. Ask about special exhibit packages and sponsorships. Acceptance of advertising by the Journal does not imply endorsement of products.
Copyright © 2023 by the Delaware Academy of Medicine / Delaware Public Health Association. Opinions expressed by authors of articles summarized, quoted, or published in full in this journal represent only the opinions of the authors and do not necessarily reflect the official policy of the Delaware Public Health Association or the institution with which the author(s) is (are) affiliated, unless so specified.
Any report, article, or paper prepared by employees of the U.S. government as part of their official duties is, under Copyright Act, a “work of United States Government” for which copyright protection under Title 17 of the U.S. Code is not available. However, the journal format is copyrighted and pages June not be photocopied, except in limited quantities, or posted online, without permission of the Academy/DPHA.Copying done for other than personal or internal reference use-such as copying for general distribution, for advertising or promotional purposes, for creating new collective works, or for resale- without the expressed permission of the Academy/DPHA is prohibited. Requests for special permission should be sent to ehealy@delamed.org
ISSN 2639-6378
June 2023 Volume 9 | Issue 2
The issue of homelessness, poverty, and substandard housing is a significant public health concern that affects millions of individuals worldwide. Homelessness is the state of lacking a permanent, safe, and adequate dwelling, while substandard housing refers to conditions that do not meet basic health and safety standards. These issues have far-reaching implications for public health, as they contribute to the spread of communicable diseases, exposure to environmental hazards, and the exacerbation of physical and mental health problems.
Individuals facing homelessness and those living in substandard housing are at an increased risk of exposure to environmental and infectious diseases due to poor living conditions and limited access to healthcare. They may also lack access to clean water, sanitation facilities, and basic hygiene necessities, further increasing their vulnerability to illness. Moreover, these individuals often face barriers to healthcare, including limited access to medical care, lack of health insurance, and difficulties accessing medication.
In addition to physical health concerns, homelessness and substandard housing have a significant impact on mental health. The stress of living in unstable and unsafe environments, coupled with the lack of support networks, can lead to anxiety, depression, and other mental health concerns. Individuals facing homelessness also face a greater risk to their personal safety, and of substance abuse and addiction

Addressing the connection between homelessness, substandard housing, and public health requires a multi-sectoral approach that involves collaboration between healthcare, housing, and social services. Efforts to improve access to affordable housing, healthcare, and social support networks can help address the root causes of these issues and improve public health outcomes for vulnerable populations.

We were privileged to be interviewed on this topic by the University of Delaware’s First State Insights online radio show. Our comments amplify this brief summary and we encourage you to take a listen for free: Housing, Place, and Health Outcomes by First State Insights (soundcloud.com)
Homelessness and substandard housing are significant public health concerns that require urgent attention, and we hope this issue helps explicate these areas for the reader. This issue, we welcome guest editors from the University of Delaware: Dr. Stephen Metraux, Roger Hesketh, and Mimi Rayl from the Center for Community Research and Service, and Sean O’Neill from the Institute for Public Administration; they have gathered a number of excellent articles. As always, we look forward to hearing from you with your feedback on this issue, and suggestions for future issues of the Delaware Journal of Public Health.
IN THIS ISSUE
Timothy E. Gibbs, M.P.H Publisher, Delaware Journal of Public Health
Doi: 10.32481/djph.2023.06.001
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
3
An Introduction to the Homelessness, Housing & Poverty Issue
Stephen Metraux, Ph.D.
Associate Professor, Biden School of Public Policy and Administration, Director, Center for Community Research and Service, University of Delaware
Roger Hesketh
Assistant Policy Scientist, Center for Community Research and Service, University of Delaware
Sean O’Neill, M.C.P Policy Scientist, Institute for Public Administration, University of Delaware
Mimi Rayl, M.R.P.
Ph.D. Student, Housing Initiatives Coordinator, Center for Community Research and Service, University of Delaware
We are pleased to present this special issue of the Delaware Journal of Public Health, with a focus on homelessness, housing and poverty. These three topics are tightly intertwined with each other, and with public health. Briefly put, as both poverty and access to affordable housing become more acute, homelessness becomes more widespread and entrenched. Poverty and housing are both elemental in their roles as social determinants of health; as deprivation of income and housing impacts both individual and population health in numerous ways. When economic and housing conditions lead to homelessness, this confluence produces a multiplier effect, as existing health conditions become exacerbated and vulnerabilities to a range of new health risks abound.
This issue features an unprecedented collection of studies on these three intertwined topics as they manifest in a Delaware context. While homelessness, housing and poverty are all prominent problems in Delaware, most of our understanding about the dynamics of these topics comes from other places and do not factor in Delaware’s unique constellation of political, services and socioeconomic structures. As such, these studies start to define how broader dynamics around public health and services provision play out in this unique setting.
We present these studies in three sections. In the first section, six studies use different empirical data sources to show how homelessness plays out in Delaware in specific populations and circumstances.
•Metraux (one of the issue editors) and Peuquet use almost two decades worth of counts of people experiencing homelessness and beds that shelter them to show how, perversely, homelessness in Delaware is at unprecedented levels while the supply of temporary housing available to shelter them has seen substantial cutbacks.
•Two studies, Borton et al. and Metraux and Modeas, apply data from state systems to document alarmingly high levels of homelessness among people in known risk groups: those who receive behavioral health treatment services and those who are on the state’s sex offender registry, respectively.
•Roberts and Mohan use data collected from interviewing services providers to document the extreme vulnerability to homelessness and housing insecurity experienced by individuals with intellectual and developmental disabilities who are served by the state’s Division of Developmental Disabilities Services in the midst of the current housing crisis.
•Nescott et al. demonstrate a hidden cost of homelessness, estimating that, in 2019, experiencing homelessness was associated with excess Medicaid costs of $4,611 (non-chronic homelessness) to $5,218 (chronic homelessness) per person.
•Cutuli et al. develop an approach that matches homeless, Medicaid, and eviction court data and show the feasibility of such an approach to identify adults and children who are at risk for health complications associated with their housing instability.
4 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.002
These studies are noteworthy in their compelling documentations of how housing need specifically impacts vulnerable populations, and the urgency for housing-specific responses to be part of the mix of services that most of those in the populations studied receive from healthcare, social services and criminal justice systems in Delaware. Beyond this, the studies collectively bring to bear, in a manner unprecedented in Delaware, the power of data to inform policy and services on homelessness in Delaware. These studies lay a foundation for an empirically grounded research agenda and additional innovative uses of available data.
The second section of this issue features seven analyses of special topics within the realm where homelessness, housing and poverty intersect. Nescott et al. provide an overview of poverty in Delaware, the first such assessment to incorporate the years following the onset of the COVID-19 pandemic, Dillard and Mers take a deeper dive into a specific aspect of poverty with her focus on the “benefits cliff” faced by extremely low- and low-income families when they attempt to gain economic self-sufficiency. Other analyses show how homelessness, housing and poverty exacerbate preexisting disparities in a range of health and social outcomes (Rent); magnify the impact of climate change (Perez & Swiatek); and represent burdens borne disproportionately by sexual minority groups (Mitsdarffer et al.) and domestic violence survivors (Beard). Finally, Millard et al. demonstrate the need for housing repair assistance, and how modest help with home repairs and modifications act to both preserve housing stock and enable healthier lives. Each of these studies opens a door into a specific facet of the topics covered in this special issue, and situate it in Delaware, thereby giving it dimensions that are at once more familiar and more difficult to ignore.
The third section provides seven views from providers who bear witness to the quotidian manifestations of homelessness, housing scarcity, and poverty and simultaneously labor to ameliorate the concomitant deprivations. Taylor and Young each report from their vantage points as heads of the United Way of Delaware and the Delaware State Housing Authority, respectively, on assistance for housing development (Taylor) and homeless services (Young). Kalmbach and Laymon each describe their programs; the former an art-inspired day center and the latter a Christian-oriented shelter and transitional housing facility, and put forth two very different approaches to addressing homelessness, a problem that both acknowledge, for different reasons, is getting worse.
Rounding out these dispatches are ones from:
•Blanch on how Beebe Health System has been expanding its commitment to identifying and responding to the social determinants of health of its patient population and support connection to appropriate resources.
•August on Jefferson Street Center, a community development corporation, and its efforts at revitalization and community-building in Northeast Wilmington.
•Strmel on how Delaware’s Division of Public Health implemented COVID-19 prevention and mitigation strategies in Delaware’s homeless shelters.
These provider perspectives complement those provided by the empirical research studies in the first section and the analyses in the second section.
Taken together, the studies in this issue show the many ways in which homelessness, housing and poverty manifest themselves in Delaware. The reader will get a good idea of not only the challenges faced by those involved with these topics, but also the work that is being done. It promises to give the reader a solid point of departure from which to continue the critical work of addressing these issues.
5
Homelessness In Delaware: An Assessment
Stephen Metraux, Ph.D. & Steven W. Peuquet, Ph.D. Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
ABSTRACT
The authors provide an assessment of trends and dynamics of homelessness in Delaware since 2007, when the last systematic study of this topic was released. Using population data on homelessness in the state, the authors present evidence that, after a period of apparent stability, homelessness in Delaware is currently at levels that are unprecedentedly high, while providers of homeless services have not adapted to this change. As a first step to addressing this alarming trend, the authors call for stakeholders to regroup and develop a coordinated, statewide approach to address this problem.
INTRODUCTION
The number of people in Delaware who were counted as homeless on a given night doubled between 2020 and 2022.1 Housing Alliance Delaware (HAD), who organizes the annual counts of Delaware’s homeless population, announced it without much fanfare. Media outlets dutifully reported this unprecedented surge. Beyond that there was little response, and assistance for emergency housing was actually cut later in the year. In this essay, we frame this moment, when the response to homelessness in Delaware appears incommensurate to the extent of need, in an historical context that goes back to 2007, when the last systematic assessment of homelessness in Delaware was undertaken. Such an analysis provides insight on how homelessness in Delaware got to this present situation, as well as a basis for how to proceed.
Sixteen years ago, in 2007, University of Delaware’s Center for Community Research and Service (CCRS) released a report titled Homelessness in Delaware: Twenty Years of Data Collection and Research. 2 The study looked back to 1987, when CCRS conducted the first study of the extent and nature of homelessness in Delaware. Based upon that and subsequent counts of the state’s homeless population, the CCRS report found there to have been an initial decade of marked increase (from 1986 to 1995), followed by a decade during which the size of the homeless population first dipped and then remained constant. This assessment was a milestone, both because it was the first longitudinal analysis of homelessness in the state, and because, for the first time, data was available to support such an empirically grounded retrospective.
The CCRS report presented a picture of cautious optimism. Homelessness was not getting worse, and, after adjusting for general population growth, was lower than the national rate. The US Department of Housing and Urban Development (HUD) and national advocacy groups, through strategies that targeted “chronically homeless” individuals and called for services enriched permanent housing to supplant shelters, offered means by which to reduce and even eliminate homelessness.3 Finally, local initiatives were falling into place for collecting data, both from comprehensive, single-night counts and from compiling administrative records on shelter and other homeless services, as a means to monitor progress in efforts to reduce homelessness.
After the 2007 CCRS report came a pair of successive reports from the Delaware Interagency Coalition on Homelessness (DICH). DICH was launched in 2005 by Governor Ruth Ann Minner’s executive order, and consisted of representatives from state agencies and key community stakeholders. The reports that DICH issued were plans, ambitiously titled Breaking the Cycle: Delaware’s Ten-Year Plan to End Chronic Homelessness and Reduce Long-Term Homelessness4 (2007) and Delaware’s Plan to Prevent and End Homelessness5 (2013), that built on the belief that homelessness was a problem that could be solved. Both DICH plans laid out roadmaps, but there has been no subsequent examination of how (or even whether) these plans were implemented, or of any impact these plans may have had. Homelessness in Delaware has clearly grown to a scale far greater than what was envisioned by these plans. But beyond that we know little about the interplay between dynamics of the homeless population and the availability of services to house them, both temporarily and permanently.
ASSESSING HOMELESSNESS IN DELAWARE
The 2006 count of Delaware’s homeless population, examined in detail in the 2007 CCRS report, was the first of what has become an annual series of Point in Time (PIT) counts of the homeless population, both in Delaware and nationwide, that continue to this day. The core of the PIT count involves volunteers and outreach workers going to interim housing facilities and to other, non-shelter locations to count people experiencing homelessness. PIT counts are conducted in late January, and results are reported to (and standardized by) HUD.6 For the past 17 years, HUD has issued an Annual Homeless Assessment Report to the US Congress based upon these data and has made these reports and the underlying PIT data available online.7 PIT counts are the means by which the magnitude of homelessness is most commonly assessed, analogous to what the unemployment rate is to labor and the consumer price index is to inflation: imperfect but ubiquitous.
Figure 1 shows the annual size of the homeless population from Delaware’s PIT counts for the years 2006 through 2022.8 We see this series of counts as consisting of two segments. The first segment, starting with the 2006 count of 1,089 homeless people,
6 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.003
shows little evidence of sustained increases or decreases for the next 13 years. While the rise in 2009 coincides with the immediate aftermath of the Great Recession, overall population changes look to be minor fluctuations more than any clear evidence of sustained increases or decreases. These fluctuations may also have more to do with inconsistencies in the counting process, which is sensitive to weather, numbers of volunteers, and other intangibles unrelated to the actual population size, than to actual changes in the homeless population.
While Delaware’s PIT count remained largely unchanged, Delaware’s overall population between 2006 and 2018 increased from 864,764 to 973,764, a 12.6 percent increase.9 This means that Delaware’s rate of homelessness, which was 12 per 10,000 people in 2007, dropped to 9.6 per 10,000 in 2019.7 So, while the homeless population size was relatively unchanged, homelessness as a proportion of the overall population declined by about 25 percent over this time. However, homelessness in the US also declined over this period, from 22 to 17 per 10,000.7 This amounted to a 23 percent rate of decline nationally, comparable to Delaware’s rate of decline.
Taken together, in 2019 (as in 2006) Delaware’s level of homelessness remained at the low end of what is “typical” for rates in other US states. Such a consistently low rate more likely reflects Delaware’s relative lack of highly urbanized areas and relatively low housing costs, than how Delaware has responded to homelessness. There is no evidence in Delaware’s homeless population counts that specific programmatic initiatives—like the DICH reports—were linked to systematic decreases in the homeless population.
In abrupt contrast, the second segment of annual Delaware PIT counts shows three consecutive and substantial year-to-year increases. This started with a count of 1,165 in 2020, a 26.5 percent increase and, at the time, Delaware’s highest PIT count ever. This rate of increase was also the highest that year of any state. By comparison, the national PIT count only increased by two percent.10 A closer look shows that Delaware’s increase was across the board – among families and individuals, sheltered and unsheltered, and those newly homeless and with long-term, “chronic” homelessness patterns.11 All this indicates a real increase in Delaware’s homeless population, rather than minor yearly fluctuations.
The 2020 count, conducted in January, preceded the COVID pandemic shutdown, and thus the increase could not be blamed on the pandemic. But additional alarming increases followed into the pandemic, with a 35 percent increase in 2021 and then a 50 percent increase in 2022. The 2022 count was ultimately more than double that of the then-record 2020 count, and in 2022 the homeless rate stood at 23.6 per 10,000. This was now substantially higher than the national rate of 18,12 and more than wiped out the population-adjusted decline that occurred over the thirteen years in the first segment.
INTERIM HOUSING CAPACITY (SHELTER, TRANSITIONAL HOUSING, AND MOTEL VOUCHERS)
The increases in the PIT counts in 2021 and 2022 reflected major changes in the way that interim housing was provided in Delaware following the pandemic lockdown. This underscores
how the PIT count is influenced not only by the size of the homeless population, but also by the supply of accommodations available to this population.
Interim housing is a term we use to include emergency shelter (EH), transitional housing (TH), seasonal shelter, and hotel/motel vouchers. All are used, in various circumstances, as temporary accommodations for homeless households (both individuals and families). HAD reports data on interim housing capacity to HUD annually in the Housing Inventory Count.13 Up through early 2020, ES and TH were the predominant forms of interim housing in Delaware. After the onset of COVID the majority of households received interim housing through hotel and motel vouchers. This reflects a stunning transformation of service delivery and provides key insights to the homeless population dynamics in the state.
Figure 2 is a time series of Delaware’s combined ES and TH capacity, broken down by family or individual household (i.e., 1-person household). For comparison, Figure 2 also shows the numbers of family and individual households that stayed in interim housing on the night of that year’s PIT count.8 This latter count reflects upwards of 90 percent of those enumerated in the PIT count, as relatively few people are typically counted in unsheltered locations in this count (more on this below). Up through 2019 the supply of ES/TH beds stayed flat for families and declined slightly for individuals, mirroring patterns for the PIT counts of family and individual households, respectively.
Figure 2’s pairing of homeless households and available ES/TH accommodations show that when there is a decline in the ES/ TH supply, there is a corresponding decrease in the number sheltered. The clearest example of this is in 2019, when the closure of the SafeSpace Delaware (formerly the Rick Van Story Resource Center), following its loss of state funding,14 was mirrored by a drop in the number of individuals in the PIT count. Having fewer shelter beds does not mean that more people resolved their homelessness. It means that there are less beds available for those experiencing homelessness, and those who are unable to get a bed are less likely to be included in the PIT count. Conversely, as happened in 2016, when the interim housing supply expands, those who occupy these additional beds are almost certain to be included in the PIT count.
The gap in most years in which the ES/TH capacity exceeds the occupancy numbers, both in family and individual households, creates the impression that there was no need to expand existing interim housing capacity. In other words, ES/TH supply seemingly stayed flat because no further capacity was needed. The view on the ground was different, however. The vacancies indicated in Figure 2 do not line up with the types of households seeking interim housing for various reasons. For example, vacancies in TH facilities designed for veterans, elderly, or persons with psychiatric disabilities will be unsuitable for those outside of these subpopulations. Thus, the Delaware Center for Homeless Veterans does not accommodate non-veterans, even if they have a vacancy. Geography is also a factor; people in southern Delaware may not be able to travel to northern Delaware, even if there are vacancies. These and other supply and demand mismatches explain why Delaware’s Centralized Intake system, a “one stop” source since 2013 for arranging shelter assignments to most of Delaware’s ES/TH facilities, reported fielding more than 1,100
7


8 Delaware Journal of Public Health - June 2023
Figure 1. Total Homeless Population in Delaware8
Figure 2. Homeless Individuals and Families and Corresponding Emergency Shelter and Transitional Housing Capacities in Delaware8,13
inquiries in July 2022 from households who were homeless or were having a housing crisis, and were only able to make 213 referrals to available homeless assistance resources.1
A final aspect that warrants further examination concerns 2021 and 2022, when the number of people staying in interim housing vastly exceeded the ES/TH supply. This overflow represents the numbers of households receiving hotel/motel vouchers, a form of interim housing not included in the ES/TH numbers in Figure 2. In Delaware, a limited supply of hotel/motel vouchers have traditionally been available to pay for short term stays when there are no other places for households to stay. The only regular provider of these vouchers is the state’s Department of Health and Social Services (DHSS), which had traditionally provided assistance for up to 50 homeless households at a time who were receiving other state-administered assistance. But with the onset of the COVID pandemic, that changed.
The COVID pandemic wreaked havoc on the provision of interim housing. Most ES and TH facilities, in Delaware and elsewhere, were in congregate settings. This means that, in some facilities, people slept with other individuals and families in large rooms, and, in most facilities, they ate and otherwise spent time with others in common areas. Such arrangements were not conducive to COVID quarantine, thus public health guidelines necessitated that congregate ES/TH facilities cut back on the number of people they accommodated and that they take other measures to limit transmission of COVID. In some cases, facilities had to close outright. Even with these precautions, many were fearful of staying at these facilities and exposing their households to COVID. In response, federal assistance provided funding to states for using hotels and motels, which had rooms sitting empty due to lockdown restrictions, to accommodate households who would otherwise have been faced with going to ES or TH facilities. In Delaware, DHSS administered this hotel/ motel voucher assistance.15
This created a situation wherein interim housing suddenly became more desirable and easier to come by. Households that were homeless and/or precariously housed, who otherwise could not or would not have stayed in ES or TH facilities, now applied for and received the DHSS vouchers. As a result, DHSS’s voucher program quickly transformed from its small-scale, short-term pre-pandemic incarnation to administering a voucher program for hundreds of households, both families and individuals, for indefinite periods of time. In 2021, DHSS provided vouchers for 839 people on the night of the PIT count, and in 2022, this number increased further to 1,056.16 At this point, DHSS was Delaware’s largest supplier of interim housing, providing emergency accommodations for more than all the ES and TH facilities combined. Then, in early fall 2022, DHSS scaled back the voucher program to pre-pandemic levels after federal support for this program was no longer available.
The 2021 and 2022 PIT count numbers provide a window into the actual demand for interim housing in Delaware. HAD called it “a crisis laid bare,”11 as it revealed the presence of hundreds of additional individuals and families who were homeless but who otherwise would have been invisible in the PIT count. DHHS data indicated, for example, that the majority of voucher holding families came from Sussex County, the southernmost of Delaware’s three counties that contains a
quarter of Delaware’s population and was the most underserved in terms of interim housing until vouchers became available.17 As mentioned earlier, indications are that Delaware’s homeless population was on the increase even before the pandemic due to a tightening supply of affordable housing, and this trend also likely contributed to people receiving DHSS vouchers. However, while the COVID pandemic led to less available EH and TH beds, there is no evidence that it directly led to increased levels of homelessness.
With interim housing capacity and occupancy expanding in tandem to twice its pre-pandemic levels in just two years, Delaware’s interim housing system now lacks the capacity to absorb the actual demand for interim housing in the wake of DHSS’s voucher program rollback. Little is known as to what people, facing homelessness and who otherwise would have applied for vouchers, are now doing. Presumably, they will retreat into a world of makeshift housing arrangements that include sleeping outdoors, in cars, in exploitative or abusive situations, “doubled up” with friends or relatives, or in substandard housing, where only a sliver of them will get included in the PIT count.
UNSHELTERED HOMELESSNESS
In the 2006 PIT count, outreach workers and volunteers fanned out across the state to count people who were homeless and sleeping in unsheltered locations. They counted 213 persons, with the acknowledgement that this count was far from comprehensive. This was the most people that were ever counted in Delaware PIT count. Subsequent unsheltered counts have been as low as 22 (2011-2012), 10 (2013), and 37 (2014-2015). In 2020 and 2022 the unsheltered counts were at 150 and 154 people,8 respectively, the highest tallies since 2007.
There is no evidence that fluctuations in the unsheltered PIT counts reflect changes in the actual numbers of persons experiencing unsheltered homelessness. A more likely explanation is that resources and conditions particular to individual PIT counts can better explain the drops in unsheltered counts in the early 2010s, and the fluctuations in numbers in other years. Even when the numbers went back up to 150, which paralleled the increases in the overall PIT counts discussed previously, these were likely still substantial undercounts.
The unsheltered portion of the PIT count, in general, is notorious for its methodological limitations.18 Even in a state as small as Delaware, the resources needed to adequately canvas the state far exceed what is available. Even then, the unsheltered homeless population seeks, by default, to be unnoticed, unobtrusive and hidden, often staying in locations that would only be found if their whereabouts were known beforehand. In two tragic illustrations of this, in 2019, four people died from carbon monoxide poisoning while sleeping in a tent with a faulty heater,19 and in 2020 a man, 64 years old, a veteran, and diagnosed with severe mental illness, died of exposure, literally on Main Street, in Newark.20 None of these people were receiving services, and none were included in the PIT count.
Two other counts of homeless subpopulations indicate the magnitude of the Delaware PIT’s undercount of those experiencing homelessness in circumstances other than interim housing. One is a study, included in this issue, of homelessness among people on Delaware’s sex offender registry (SOR).21 People
9
on the SOR are required to report their residence regularly to state police and must check in monthly when they are experiencing homelessness. Their homeless status is noted on their SOR record, which is publicly available online.22 On a night in November 2021, 121 people on the SOR reported homelessness; on a night in February 2023, that number rose to 140. Less than 10 people in each of these counts reported staying in interim housing; indeed, most homeless facilities are off limits to people on the SOR. Thus, the number of people who are homeless (presumably unsheltered) and on the SOR is almost as many as were counted as unsheltered on the 2022 PIT (n=154). Assuming that people on the SOR would constitute, at most, only a modest minority of the unsheltered population, the actual size of the overall unsheltered homeless population in Delaware could easily exceed 400 or 500. The second count covers a very different population: children and youth enrolled in Delaware’s 19 public school districts who were identified as “homeless” in reports to the US Department of Education (DOE). Over the course of the 2018-2019 academic year, the DOE count had 3,539 students as homeless, with only 122 of these students staying in interim housing. The large majority lived doubled up (2,604) and, by definition, not covered by the PIT count. As the PIT counts increased in subsequent years, the DOE counts dropped to 2,709 (2019-2020) and 2,576 (2020-2021). These decreases were attributed to the added difficulties in identifying homeless students during the COVID pandemic.23 While the PIT counts and the DOE counts are not directly comparable, the DOE count provides a window into how large numbers of homeless and precariously housed families are missed by the PIT count. Presumably, these households who were among those who “appeared” in the 2021 and 2022 PIT counts when hotel/motel vouchers were more available, and will again be uncounted in the PIT count now that these vouchers are scarcer.
CHRONIC HOMELESSNESS AND PERMANENT SUPPORTIVE HOUSING
Among the first goals to reducing Delaware’s homeless population was “to adopt and oversee the implementation of a plan to reduce homelessness and end chronic homelessness in Delaware.” DICH’s 2007 plan, Breaking the Cycle, laid out the process to do just that, with the key element consisting of adding 409 new units of permanent supportive housing (PSH) to the existing supply of 277 units.4
PSH, simply put, is the provision of housing that is both affordable and coupled with support services that provide whatever is needed to let the tenant maintain this housing. This housing targets the most difficult to serve among the homeless population, and consistently shows retention rates of around 85 percent.24 This housing is often targeted to people designated as “chronically homeless,” meaning households in which a person has a disabling condition and who has either been continually homeless for a year or more or has had at least four episodes of homelessness in the past three years. In a typical homeless population, less than 20 percent meet the chronic threshold, yet this subpopulation typically consumes upwards of 80 percent of homeless services. Thus, the DICH report asserted that not only would such a near-tripling of Delaware’s PSH supply disproportionately reduce the need for homeless services, but it would also lead to substantial collateral reductions in this group’s use of inpatient hospital, criminal justice and emergency health care services.4
Tracking the progress to attaining the twin goals of an increased statewide PSH supply and a reduced number of people in the homeless population meeting chronic criteria are both possible using HIC data from Delaware that is reported to HUD.11 The benchmark used in the 2007 DICH plan was 297 chronically homeless persons,4 with the goal being to reach zero in ten years by, in part, having 686 PSH units in the state. This housing target was surpassed in 2019, with 724 PSH units dedicated to housing people who had experienced chronic homelessness,11 but there remained 168 people counted in the 2019 PIT count who were considered chronically homeless.8
Following the attainment of this benchmark, the number of PSH units started to decline. By 2022, the number of dedicated units had dwindled back to 420 units.11 Meanwhile, in a manner that reinforces the inverse relationship between PSH supply and numbers of people considered chronically homeless, in 2022 the PIT count enumerated 223 people as chronically homeless, sliding back toward the number cited in 2007.1 This decline in PSH is not a deliberate policy, rather it is partially due to existing projects converting PSH units to more conventional housing, as well as there being difficulty in attracting organizations to develop and manage new PSH housing in Delaware.25
Additionally, the goal in the 2007 DICH report may have been too modest, and an updated assessment is needed to determine the number of PSH units in which the annual turnover in tenants matches the demand for housing from people newly identified as chronically homeless.
DATA COLLECTION
The 2007 CCRS report and the 2007 DICH plan both drew heavily on the body of data on Delaware homelessness that was emerging at the time. The CCRS report notes the substantial progress made in two fundamental areas of data collection to guide efforts to reduce homelessness.2 One was establishing the PIT count. The second was the creation of a homeless management information system (DE-HMIS) that systematically collects administrative data compiled by homeless service providers in the state during the course of providing shelter and other services. The DICH plan endorsed the DE-HMIS, and went a step further in stating that “State Departments and Divisions should become users of DE-HMIS, both as the recipients and the providers of data.”4
Seventeen years later, we now have annual PIT count data available for studies, such as this one, which can use it, despite its clear flaws, as a basis for sketching a broader picture of the state of homelessness in Delaware. Getting accurate assessments of the nature and extent of the homeless population is a key first step for better determining the levels and types of resources needed to reduce, and ultimately solve homelessness.
The DE-HMIS, now known as the Community Management Information System (CMIS), also is well-established as a central data repository for administrative records on services provided by homeless service organizations, including shelters, transitional housing programs, PSH providers, outreach programs, and others. As described in the CCRS report, this web-based information system is a powerful means for making the collection of homelessness-related data systematic, accurate and inexpensive.2 Recent studies have combined CMIS data with other data sources to examine connections between homelessness and eviction,26 as well as (in this issue) the costs
10 Delaware Journal of Public Health - June 2023
that homelessness adds to Medicaid expenditures.27
However, the usefulness of the CMIS database is severely restricted by large gaps in the data it collects. One major data hole comes from the refusal of Delaware’s second largest provider of interim housing to share data on their services. A second and larger data hole is the inability of the State of Delaware and HAD, the organization that maintains CMIS, to develop a mechanism by which the State will share with CMIS their data on hotel/motel vouchers. In the wake of the recent expansion of the DHSS voucher program, this has led to a situation where data on homeless services reside in two isolated and incomplete databases, neither of which can be used to draw comprehensive conclusions about homelessness in Delaware at a point when comprehensive data is needed more than ever to address this crisis.17
2023 AND LOOKING AHEAD
As this article was going to press, preliminary 2023 PIT count and HIC results became available.28 Overall, the number of people counted as homeless in Delaware on the night of the count was 1,245 people. This number is substantially lower than the overall numbers from the last two PIT counts (see Figure 1), but is still higher than any of the pre-pandemic PIT counts, dating back to the first PIT count in 2006. Similarly, the preliminary 2023 HIC reported a substantial drop in the statewide supply of interim housing (emergency shelter, transitional housing, and hotel/ motel vouchers), largely driven by the rollbacks the State made in is hotel/motel voucher program, from 1,056 vouchers on a given night in 2022 to 98 vouchers in 2023.
While this drop in the PIT count will likely be framed as a reduction in the homeless population, our analysis here indicates that cuts in the availability of interim housing better explains this reduced count. In the absence of any signs that poverty has eased or that housing has gotten either more available or less costly over the previous year, a more likely explanation is that, were hotel and motel vouchers as available in 2023 as they were in 2022, there would be no reason to expect any reduction in this year’s PIT count.
Furthermore, in the wake of the reduction in hotel/motel voucher supply, one would expect that more people who otherwise might have received vouchers would be without any housing. The PIT count supports this assumption. Despite the overall drop in the PIT count, the count of the unsheltered homeless subpopulation increased in 2023, from 154 in 2022 to 198. This increase occurred despite a cold, pouring rain that fell on the night of the PIT count, as well as the dismantling of the Milford29 and Georgetown encampments30 earlier that January. In 2022, as many as 100 people lived in unsheltered circumstances in these two sites; places where they could readily be counted last year but stood empty just before this year’s count. That, in spite of these factors, there was such an increase in the unsheltered count this year indicates that actual homelessness has increased while the PIT count has dropped.
Ironically, these contemporary, heightened levels of homelessness coincide with the tenth anniversary of DICH’s ten-year plan to “prevent and end homelessness.”5 More than that, many of the problems called out by the previous reports from DICH and CCRS remain. Instead of visions of chronic homelessness being
diminished through an expanded availability of housing for this population, a declining supply of this housing has ushered in the same levels of chronic homelessness seen in 2007. Instead of being at the threshold of a coordinated and comprehensive data collection system, Delaware is still left without the basic tools for getting a systematic accounting of the nature and extent of its homeless population. And, based upon the fragmented data we present here, the size of the unsheltered homeless population conceivably exceeds that of those staying in interim housing. There have been no statewide initiatives that have addressed homelessness in Delaware since the PIT counts started increasing in 2020. Governor John Carney’s administration has not made any policy pronouncements on homelessness over this period. After using federal funding to massively increase access to hotel/motel vouchers, the State has scaled the program back to pre-COVID levels after federal funding ended. Beyond that, Governor Carney, in his most recent budget address, promoted increased state investments in affordable housing, but asserted that homelessness is “a very different problem” from the housing initiatives he has proposed to fund.31
Delaware’s nonprofit homeless services providers, when faced with the doubling of the homeless population, have stewarded a services system that is largely unchanged from its pre-pandemic structure. Part of this is dictated by the levels of available funding, but there has also been a lack of any stated vision or blueprint about how the homeless services system could better respond to homelessness at its current magnitude. The last time that the Delaware Continuum of Care (CoC), the collective of Delaware’s homeless services providers, assessed the state of homelessness was in 2017 with an action plan called Ending Homelessness in Delaware. 32 This action plan laid out specific, systemwide objectives and measures for responding to homelessness, along with a call for the CoC to report back two years later on the progress made toward implementing these objectives and measures. This follow up is now three years past due.
Finally, Delaware lacks an active grassroots advocacy structure focused on homelessness. The recent doubling of the homeless population and subsequent scaling back of services has been met with a conspicuous lack of protest, resistance, or calls for action coming from outside of the homeless services delivery systems. The one piece of legislation in front of the Delaware State Legislature that calls for a substantially different approach to addressing homelessness, the Homeless Bill of Rights (HB 55),33 has a limited backing and little prospect for passage. While Shyanne Miller, an advocate with the H.O.M.E.S. Campaign, acknowledges a need for radical action to end homelessness in Delaware and to fully realize housing as a human right, she also acknowledges the “pervasive silence amongst advocates serving people experiencing homelessness. There’s not enough community outcry and public rejection of austere policies that reduce resources and criminalize people experiencing homelessness.”34
In the absence of a statewide response, the most substantial activities in addressing Delaware’s homelessness are happening on local levels. In 2021, New Castle County, for example, purchased and repurposed a Sheraton hotel into what is now the Hope Center, the largest homeless facility in the state.35 In Georgetown, a partnership between the municipal government and the nonprofit Springboard Collaborative was instrumental in creating
11
a pallet shelter village to provide interim housing to Georgetown’s burgeoning unsheltered homeless population.30 These initiatives both leveraged federal COVID funding to launch these initiatives. In Kent County, the nonprofit organizations Dover Interfaith Housing and Code Purple Kent County are each in initial steps of building new interim housing capacity. While such expansions of capacity are badly needed, they are also ad hoc and not part of a more coordinated response.
A coordinated, statewide response is a critical first step toward addressing what are, based on the data presented here, unprecedented levels of homelessness for Delaware, even after the reductions in the 2023 PIT count results. In 2005, Governor Minner convened DICH to spearhead an effort to end homelessness. In 2007, CCRS’s report set the stage for a very well-attended statewide conference to further assess and act upon homelessness in Delaware. Sixteen years later, a similar convening is again needed to reinvigorate its approach, create an updated plan, and provide a collaborative framework for addressing homelessness. While unity and direction are prerequisite, such a first step will be followed by challenges related to implementation and assessment, given their historical absence in the wake of the plans reviewed here.
In summary, the pandemic has not so much induced waves of new homelessness as exposed deficiencies in how homelessness is being addressed. However, it also presents an opportunity for proceeding in a new manner. Putting these dynamics together creates a situation in which taking action commensurate to the current magnitude of the homelessness problem is critical, lest the problem become even larger and more intractable in the future.
Dr. Metraux may be contacted at metraux@udel.edu.
REFERENCES
1. Housing Alliance Delaware. (2022). Housing and homelessness in Delaware: 2022. Housing Alliance Delaware. Retrieved from:
https://www.housingalliancede.org/_files/ ugd/9b0471_322d16c2158c4ab09743a897dc12aa6d.pdf
2. Peuquet, S. W., Robinson, C. B., & Kotz, R. (2007). Homelessness in Delaware: Twenty years of data collection and research. University of Delaware Center for Community Research and Service and the Homeless Planning Council of Delaware. Retrieved from: https://udspace.udel.edu/server/api/core/bitstreams/2c5d57a8-cad4495a-bc4a-54fbc9bc6c02/content
3. Burt, M. R., Hedderson, J., Zweig, J., Ortiz, M. J., & Aron-Turnham, L. (2004). Strategies for reducjng chronic street homelessness. Department of Housing and Urban Development Office of Policy Development and Research. Retrieved from: https://www.huduser.gov/publications/pdf/chronicstrthomeless.pdf
4. Delaware Interagency Council on Homelessness. (2007). Breaking the cycle: Delaware’s ten-year plan to end chronic homelessness and reduce long-term homelessness. Delaware State Housing Authority. Retrieved from: http://www.destatehousing.com/FormsAndInformation/Publications/ delaware_ten_yr_plan.pdf
5. Delaware Interagency Council on Homelessness. (2013). Delaware’s plan to prevent and end homelessness. Delaware State Housing Authority. Retrieved from: http://www.destatehousing.com/FormsAndInformation/Publications/ plan_end_homeless.pdf
6. Exchange, H. U. D. (2015). Point-in-time count methodology guide. Department of Housing and Urban Development. Retrieved from: https://www.hudexchange.info/resource/4036/point-in-time-countmethodology-guide/
7. Exchange, H. U. D. (2023). AHAR Reports. Department of Housing and Urban Development. Retrieved from: https://www.hudexchange.info/homelessness-assistance/ahar/#2022-reports
8. Exchange, H. U. D. (2023). CoC homeless populations and subpopulations reports. Department of Housing and Urban Development. Retrieved from: https://www.hudexchange.info/programs/coc/coc-homelesspopulations-and-subpopulations-reports/
9. The Disaster Center. (2020). Delaware crime rates: 1960-2019. The Disaster Center. Retrieved from: https://www.disastercenter.com/crime/decrime.htm
10. Henry, M., de Sousa, T., Roddey, C., Gayen, S., & Bednar, T. J. (2021). The 2020 annual homeless assessment report (AHAR) to Congress. The U.S. Department of Housing and Urban Development, Office of Community Planning and Development. Retrieved from:
https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf
11. Housing Alliance Delaware. (2020). Housing and homelessness in Delaware: A crisis laid bare. Housing Alliance Delaware. Retrieved from: https://www.housingalliancede.org/_files/ ugd/9b0471_8c4b0aad6a664d309794565c70e8ff42.pdf
12. de Sousa, T., Andrichik, A., Cuellar, M., Marson, J., Prestera, E., & Rush, K. (2022). The 2022 annual homeless assessment report (AHAR) to Congress. The U.S. Department of Housing and Urban Development, Office of Community Planning and Development. Retrieved from:
https://www.huduser.gov/portal/sites/default/files/pdf/2022-AHAR-Part-1.pdf
13. Exchange, H. U. D. (2023). CoC housing inventory count reports. Department of Housing and Urban Development. Retrieved from:
https://www.hudexchange.info/programs/coc/coc-housing-inventorycount-reports/
14. Kuang, J. (2018, Dec). Most clients placed in temporary housing as ‘RVRC’ shelter closes for good in Wilmington. Delaware Online/Delaware News Journal. Retrieved from:
https://www.delawareonline.com/story/news/local/2018/12/31/ wilmington-rvrc-homeless-shelter-safespace-delawarecloses/2449603002/
15. Kiefer, P. (2022, May). Number of people experiencing homelessness in Delaware doubled over past two years. Delaware Public Media. Retrieved from:
https://www.delawarepublic.org/show/the-green/2022-05-20/numberof-people-experiencing-homelessness-in-delaware-doubled-over-pasttwo-years
12 Delaware Journal of Public Health - June 2023
16. Housing Alliance Delaware. (2022). Point in time count & housing inventory count: 2022 Report. Housing Alliance Delaware. Retrieved from: https://www.housingalliancede.org/_files/ugd/9b0471_ b4f4bc93e75c4923a891bc0d33fb4dbd.pdf
17. Metraux, S., Solge, J., & Mwangi, O. W. (2021). An overview of family homelessness in Delaware. Housing Alliance Delaware. Retrieved from: https://www.housingalliancede.org/_files/ugd/9b0471_ b09ebb113aa74d13ae09eba6677523df.pdf
18. Lee, T., Leonard, N., & Lowery, L. (2021). Enumerating homelessness: The point-in-time count and data in 2021. The National League of Cities. Retrieved from: https://www.nlc.org/article/2021/02/11/enumerating-homelessness-thepoint-in-time-count-and-data-in-2021/
19. Hughes, I., & Perez, N. (2020, Feb). ‘It’s devastating’: 4 found dead in tent at homeless camp in Stanton. Delaware Online/ Delaware News-Journal. Retrieved from: https://www.delawareonline.com/story/news/2020/02/18/large-policepresence-along-route-7-stanton/4798286002/
20. Cassidy, J. (2021, Mar). Homeless Delaware vet honored after being found dead on a cold wintry day in Newark. Delaware Online/Delaware News-Journal. Retrieved from: https://www.delawareonline.com/story/news/2021/03/26/communitycomes-together-honor-veteran-edgar-mack/6941492002/
21. Metraux, S., & Modeas, A. C. (in press). Homelessness among persons on delaware’s sex offender registry. Delaware Journal of Public Health.
22. Delaware State Police, State Bureau of Identification. (n.d.). Delaware sex offender central registry. State of Delaware. Retrieved from: https://sexoffender.dsp.delaware.gov/
23. National Center for Homeless Education. (2023). State Pages: Delaware. U.S. Department of Education. Retrieved from: https://profiles.nche.seiservices.com/StateProfile.aspx?StateID=10
24. Cunningham, M., Gourevitch, R., Pergamit, M., Gillespie, S., & Hanson, D. (2018). Denver supportive housing social impact bond initiative: housing stability outcomes. Urban Institute. Retrieved from: https://www.urban.org/sites/default/files/publication/99180/denver_ supportive_housing_social_impact_bond_initiative_3.pdf
25. Kuang, J. (2019, Nov). YMCA ends program that provides 41 beds for Wilmington’s homeless. Delaware Online/Delaware News-Journal. Retrieved from: https://www.delawareonline.com/story/news/2019/11/11/wilmingtonlose-41-beds-homeless-ymca-plans-end-program/2510678001/
26. Metraux, S., Mwangi, O., & McGuire, J. (2022, August 31). Prior evictions among people experiencing homelessness in Delaware. Delaware Journal of Public Health, 8(3), 34–38. https://doi.org/10.32481/djph.2022.08.009
27 Nescott, E. P., Metraux, S., McDuffie, M. J., & Brown, E. (in press). Health & homelessness: Matching Medicaid claims and encounters and the community management information system databases. Delaware Journal of Public Health.
28. Personal Communication. (2023). Housing Alliance Delaware.
29 Kiefer, P. (2023, Jan). Residents Milford homeless encampment disperse ahead of final sweep. Delaware Public Media.
Retrieved from:
https://www.delawarepublic.org/politics-government/2023-01-13/ residents-milford-homeless-encampment-disperse-ahead-of-final-sweep
30. Kiefer, P. (2023, Jan). Long-awaited Georgetown pallet shelter village welcomes first residents. Delaware Public Media.
Retrieved from:
https://www.delawarepublic.org/politics-government/2023-01-30/longawaited-georgetown-pallet-shelter-village-welcomes-first-residents
31 Carney, J. (2023). Governor Carney presents FY24 budget
Retrieved from:
https://www.youtube.com/watch?v=UxCaUQLcYgo (38:35 in video).
32 Delaware Continuum of Care. (2017). Ending homelessness in Delaware: Our action plan. Delaware State Housing Authority. Retrieved from: http://www.destatehousing.com/OtherPrograms/othermedia/h4g_ action_plan_2017.pdf
33. Lynn, S. (2023). House substitute 1 for House Bill 55. Delaware General Assembly. Retrieved from: https://legis.delaware.gov/BillDetail?legislationId=130082
34 Miller, S. (2023, Apr 24). H.O.M.E.S. Campaing. Personal communication.
35 Kuang, J. (2020, Dec). ‘I’m not scared anymore’: New Castle County’s hotel-turned-homeless shelter gets underway. Delaware Online/Delaware News-Journal. Retrieved from: https://www.delawareonline.com/story/news/2020/12/23/new-castlecountys-hotel-turned-homeless-shelter-housing-73-people/3990700001/
13
Demographics of the Population Experiencing Homelessness and Receiving Publicly Funded Substance Use and Mental Health Treatment Services in Delaware
David Borton, M.A.
Center for Drug and Health Studies, University of Delaware
Rachel Ryding, Ph.D.
Center for Drug and Health Studies, University of Delaware
Meisje J. Scales, M.P.H., C.P.S. Center for Drug and Health Studies, University of Delaware
Kris Fraser, M.P.H., P.M.P.
Division of Substance Abuse and Mental Health, Delaware Department of Health and Social Services
ABSTRACT
Objective: To determine the prevalence of clients experiencing homelessness in publicly funded substance use and mental health services in Delaware and uncover basic patterns in the demographics and service access of said clients. Methods: We analyzed Consumer Reporting Form data for clients admitted to publicly funded substance use and mental health treatment. All clients who were admitted to services from a publicly-funded provider and completed the CRF between 2019 and 2021 were included in this analysis (n=29,495). Results: 5,717 clients (19%) reported experiencing homelessness. 20% of men reported homelessness, compared to 18% of women, and 22% of Black clients reported homelessness, compared to 19% of White clients. 48% of admissions were to substance use treatment, 29% were to mental health treatment, and 23% were to treatment for both. Conclusions: Nearly one-fifth of clients who received publicly funded treatment between 2019 and 2021 reported experiencing homelessness, a vast overrepresentation when compared against the less than 1% of the population who was counted as homeless through the annual PIT count in Delaware. Policy Implications: Homelessness can be experienced across the lifespan and impacts individuals and families of all demographic makeups. Individuals are often unable to access primary care, insurance supported services, and chronic disease management teams resulting in a disproportionately high use of emergency services and departments for acute needs.
Funding for this project has been provided by the Delaware Department of Health and Social Services, Division of Substance Abuse and Mental Health through the Substance Abuse and Mental Health Services Administration (SAMHSA).
INTRODUCTION
Across the United States, the increasing prevalence of homelessness and other forms of housing insecurity present a major social justice issue. Social and economic conditions brought on during the COVID-19 pandemic have in some cases exacerbated housing issues that preceded the pandemic and have made housing less accessible and more expensive for many low-income households. Access to safe and affordable housing functions as a social determinant of health,1 making it important to examine populations experiencing homelessness from a public health lens. Conditions of homelessness can put people at greater risk for early mortality as well as for contracting infectious and chronic diseases.2
Per federal requirements, at a minimum, publicly funded substance use disorder and mental health treatment services in the United States must collect admissions and discharge data from the clients they serve. In Delaware, this data is collected using the Consumer Reporting Form (CRF) and reported by providers to
the Division of Substance Abuse and Mental Health (DSAMH). This state-level data is then reported and compiled as Substance Abuse and Mental Health Services Administration’s (SAMHSA) Treatment Episode Data Set (TEDS).
While there has been no recent publication of Delawarespecific data regarding clients in substance use disorder (SUD) treatment who have been or are currently homeless, there has been research using national TEDS data or data specific to other states. One study of treatment data in California found that people experiencing homelessness, when compared to clients with stable housing, have lower rates of retention and successful discharge, a greater prevalence of mental health diagnoses and unemployment, and were more likely to receive residential treatment.3 Another study, focused on national data, reported that while 12.5% of clients admitted for opioid use disorder treatment were experiencing homelessness, those who reported experiencing homelessness were less likely to receive medicationassisted treatment than clients in stable housing; those clients experiencing homelessness were also more likely to be male and admitted to a residential program.4
Because of the often-hidden nature of homelessness, it can be difficult to get a true measure of its prevalence across a population; as a result, groups experiencing homelessness are
14 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.004
often understudied. The Delaware Continuum of Care (COC) is a collaborative and community-based body committed to addressing homelessness in Delaware with the goal of securing housing for all. The COC conducts a point in time (PIT) count one night a year to assess the scope of the problem of homelessness in the state. In 2022, the PIT count reported 2,369 people experiencing homelessness in Delaware, which is double the number of people experiencing homelessness measured by the 2020 PIT count just prior to the onset of the pandemic.5 In particular, they found sharpest increases in homelessness among families with children, veterans, and Black or African American people.
While evidence suggests that people experiencing homelessness often have acute healthcare needs,6 there has been no recent publicized data on the prevalence of homelessness among clients receiving mental health and substance use treatment in Delaware. In this brief report, authors seek to fill this gap by using data from the CRF to analyze the prevalence of homelessness among people receiving publicly funded treatment in Delaware and key demographic characteristics of this priority population.
METHODS
We analyzed CRF data for clients admitted to publicly funded substance use and mental health treatment services in Delaware in 2019, 2020, and 2021. Clients are asked about the following: treatment and diagnosis (reported by clinician); substance use; medical status; employment; income; legal status; family; housing; and mental health. CRFs are completed at admission, discharge, and annually if the client remains in treatment longer than a year. The client’s provider interviews each client using the form, and all questions are self-reported by the client to the provider aside from diagnoses and treatment services provided which are filled out solely by the provider. All clients who were admitted to services from a publicly funded provider and completed the CRF between 2019 and 2021 were included in this analysis (n=29,495). As a part of the CRF, clients are asked for their current residential arrangement, which includes the option “None/Homeless,” as well as whether they have been homeless in the past 30 days. There is no operational definition of homeless on the CRF; as such a client’s status as homeless is determined by their own interpretation. Clients who reported past 30-day homelessness or “None/Homeless” at admission were included in the experiencing homelessness group for this analysis.
RESULTS
Between 2019 and 2021, 29,495 unique clients were admitted to publicly funded services. Of them, 5,717 clients (19%) reported experiencing homelessness at some point in that period. Table 1 summarizes rates of experiencing homelessness by demographic categories.
In this period, 20% of men reported homelessness, compared to 18% of women. When examining patterns of homelessness by race, 22% of Black clients reported homelessness, compared to 19% of White clients, 19% of mixed-race clients, and 17% of clients who reported another race. Hispanic or Latino clients had slightly lower rates of homelessness (17%) than clients who were not Hispanic or Latino (20%). Clients who did not complete high school experienced the highest rate (24%) of homelessness by education level. Similarly, clients who were unemployed had
higher rates of experiencing homelessness (29%) than any other group, followed by clients who were disabled (21%); 11% of clients who were either employed or students at admission reported experiencing homelessness. Veterans also had higher rates of homelessness (22%) than clients who were not veterans (19%).
The rate of client homelessness varied within this period. In 2019, 19% of clients experienced homelessness at some point that year (n=14,190). In 2020, the rate increased to 20% (n=12,074). In 2021, it decreased sharply to 15% (n=13,710).
Among clients experiencing homelessness in this period, 48% of admissions were for substance use diagnoses only, 29% were for mental health diagnoses only, and 23% were for co-occurring diagnoses. Table 2 shows select comparisons between the major response categories of client demographics and services accessed for both clients who experienced homelessness and those who did not during the analysis period. Withdrawal management services are short term (1-7 day) residential programs to help clients cease substance use and monitor safe withdrawal, otherwise known as detox programs. Mental health crisis services include short term (up to 30 days) admissions to residential mental health facilities. Community support services include Assertive Community Treatment, an evidence-based practice for community-based mental health treatment, DSAMH’s Community Behavioral Health Outpatient Treatment (CBHOT) Program, and case management. Outpatient includes medication for opioid use disorder (MOUD) treatment, criminal justice diversion programs for substance use, and other outpatient services. Short-term residential services include recovery housing and sober living communities, as well as residency in group homes. Long-term residential services include clients who are long-term residents of psychiatric hospitals.
15
Percentage of All Clients who Experienced Homelessness (n = 29,495) Gender Men 20% Women 18% Race Black 22% White 19% Mixed Race 19% Another Race 17% Ethnicity Hispanic or Latino 17% Not Hispanic or Latino 20% Employment/Education Less than HS Education 24% Employed/Student 11% Unemployed 29% Disabled 21% Veteran 22% Non-Veteran 19%
Table 1. Rates of Experiencing Homelessness by Demographics
As the table illustrates, men were represented at a slightly higher rate among those who experienced homeless compared to those who did not (61% to 57%, respectively). Black clients were more represented among clients who experienced homelessness as well (33% compared to 29%), while the opposite was true for White clients (59% compared to 62%). A much larger percentage of clients experiencing homelessness were unemployed (50%) than that of clients who were not (29%).
Clients who experienced homelessness accessed withdrawal management services at a higher rate than clients who did not (26% compared to 11%), as well as short term residential treatment (7% compared to 2%).
DISCUSSION
Nearly one-fifth of clients who received publicly funded treatment between 2019 and 2021 reported experiencing homelessness. There is no official population level estimate for homelessness in among Delawareans during this time period. The closest approximation comes from the annual PIT count, which estimates homelessness from a single night. The 2019, 2020, and 2021 PIT counts in Delaware suggested that on a given night, between 921 and 1,579 people were currently experiencing homelessness, which represents less than 1% of the population of Delaware. While point-in-time counts from a single night are not directly comparable to a measure of homelessness over the past 30 days, these data do suggest that people experiencing homelessness may
be overrepresented among DSAMH clients receiving SUD and mental health services.
When comparing treatment modalities, homelessness was more prevalent among clients admitted to substance use treatment as opposed to mental health treatment. People experiencing homelessness and people with substance use disorders are both highly stigmatized groups; when studying the intersections of these populations it is important to acknowledge that people experiencing homelessness are not typically homeless solely because of their substance use. Because of these dual stigmas associated with homelessness and substance use disorders, people experiencing homelessness who also struggle with substance use face additional barriers in accessing evidence-based health care.7 This underscores the importance of examining the demographic characteristics of this population in DSAMH services and that are more likely to serve people experiencing homelessness. Withdrawal management and short-term residential care were both identified in this data as modalities that serve a higher proportion of homeless or housing insecure clients. There was also a substantial difference in employment status among clients who reported homelessness compared to clients who were stably housed, with approximately half of homeless or housing insecure clients reporting unemployment. This suggests a strong need for workforce development programming for these clients, as well as investment in job opportunities paying a living wage.
16 Delaware Journal of Public Health - June 2023
Percent among Clients Who Experienced Homelessness (n=5,717) Percent among Clients Who
Not Experience Homelessness (n=23,778) Gender Men 61% 57% Women 39% 43% Race Black 33% 29% White 59% 62% Ethnicity Hispanic or Latino 6% 8% Employment/Education Less than HS Education 29% 22% Employed/Student 18% 36% Unemployed 50% 29% Veteran 6% 5% Service Access Withdrawal Management 26% 11% Mental Health Crisis Services 8% 12% Community Support Services 45% 44% Outpatient Treatment 10% 16% Short Term Residential Treatment 7% 2% Long Term Residential Treatment 10% 19%
Table 2. Comparison of Clients who Did or Did Not Experience Homelessness
Did
The overall rate of homelessness among the DSAMH treatment population varied over the course of the years of available data. The rate increased from 2019 to 2020, but then decreased in 2021. While extant data sources suggest an increase in the prevalence of homelessness and housing insecurity over this time period of time in Delaware5,8 these trends are not clearly reflected in our data. Given facility closures and gaps in CRF administration, it is still difficult to fully account for the impact that the pandemic may have had on both patterns in treatment enrollment and in data collection protocols across locations. In the final section of this paper we outline general public health implications for studying this population and possible future research agendas to continue the work that started here.
PUBLIC HEALTH IMPLICATIONS
Homelessness and behavioral health conditions are public health priorities that intersect when individuals need, seek, access, receive, and maintain treatment engagement. Homelessness can be experienced across the lifespan and impacts individuals and families of all demographic makeups. Though, as shown in this analysis, some are disproportionately impacted. As the rate of experiencing homelessness among DSAMH clients is higher than that of the general population, providers should consider these patterns when assessing the service needs of new clients. Further, individuals experiencing homelessness are at higher risk of morbidity and mortality from a number of causes, especially overdose.9 The reality of homelessness means that individuals are often unable to access and maintain care through primary care providers, insurance-supported services, and chronic disease management teams resulting in disproportionately high use of emergency services and departments for acute needs, including overdose and poisonings.6 As such, substance use and mental health treatment services for individuals experiencing homelessness is a public health opportunity and responsibility. In this context, the overall rate of clients experiencing homelessness found here demonstrates that, at a minimum, clients who are experiencing homelessness are successfully connecting with services. It is vital that as a part of a client’s substance use or mental health treatment, they also receive support and connection to services related to their overall wellbeing; this includes connection to housing-related services for clients who need them. As this paper is exploratory in nature and presents just a beginning to understanding this data, it is beyond our scope at this time to definitively make claims about the precise ways the pandemic may have influenced the population experiencing homelessness and receiving treatment services; while our analysis focuses on that time period, further contextualization is needed around Federal, State, community and provider level efforts related to homelessness that may have affected service access. Future research aimed at advancing the wellbeing of clients experiencing homelessness may examine admission and discharge trends in 2020 and beyond as more data is collected, paying close attention to differences in the type of treatment accessed and how that aligns with client needs. While this paper only looked at admissions over three years in aggregate, future research should also seek to examine client-level characteristics over time. It will also be important to identify associations between demographic categories, such as race and gender, and treatment services in the client population experiencing homelessness. The brief report focused only on introducing these categories with the purpose of
establishing baseline prevalence rates, but an extended analysis should examine more precise interactions between these terms. Given the demonstrated prevalence of homelessness in the client population served by DSAMH treatment, it is worthwhile to continue to consider the ways that these treatment services can be better tailored to meet the needs of clients experiencing homelessness to improve both the quality of treatment they receive and their health outcomes post-treatment.
Mr. Borton may be contacted at dborton@udel.edu
REFERENCES
1. Swope, C. B., & Hernández, D. (2019, December). Housing as a determinant of health equity: A conceptual model. Soc Sci Med, 243, 112571. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31675514/ https://doi.org/10.1016/j.socscimed.2019.112571
2. Fazel, S., Geddes, J. R., & Kushel, M. (2014, October 25). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet, 384(9953), 1529–1540. https://doi.org/10.1016/S0140-6736(14)61132-6
3. Padwa, H., Bass, B., & Urada, D. (2022, June). Homelessness and publicly funded substance use disorder treatment in California, 2016-2019: Analysis of treatment needs, level of care placement, and outcomes. Journal of Substance Abuse Treatment, 137, 108711. https://doi.org/10.1016/j.jsat.2021.108711
4. Han, B. H., Doran, K. M., & Krawczyk, N. (2022, January). National trends in substance use treatment admissions for opioid use disorder among adults experiencing homelessness. Journal of Substance Abuse Treatment, 132, 108504. https://doi.org/10.1016/j.jsat.2021.108504
5. Housing Alliance Delaware. (2022). Point in Time Count & Housing Inventory Count: 2022 Report. Retrieved from https://www.housingalliancede.org/coc-reports
6. Vohra, N., Paudyal, V., & Price, M. J. (2022, July 28). Homelessness and the use of Emergency Department as a source of healthcare: A systematic review. International Journal of Emergency Medicine, 15(1), 32. https://doi.org/10.1186/s12245-022-00435-3
7. Magwood, O., Salvalaggio, G., Beder, M., Kendall, C., Kpade, V., Daghmach, W., . . . Pottie, K. (2020, January 16). The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLoS One, 15(1), e0227298. https://doi.org/10.1371/journal.pone.0227298
8. National Center for Health Statistics. U.S. Census Bureau, Household Pulse Survey, 2020–2023. Likelihood of Eviction or Foreclosure. Generated interactively: from https://www.census.gov/data-tools/demo/hhp/#/?measures=EVICTFOR
9. Fine, D. R., Dickins, K. A., Adams, L. D., De Las Nueces, D., Weinstock, K., Wright, J., . . . Baggett, T. P. (2022, January 4). Drug overdose mortality among people experiencing homelessness, 2003 to 2018. JAMA Network Open, 5(1), e2142676.
https://doi.org/10.1001/jamanetworkopen.2021.42676
17
Health & Housing in Delaware: Matching Medicaid Claims and Encounters and the Community Management Information System Databases
Erin Nescott, M.S.
Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
Stephen Metraux, Ph.D.
Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
Mary Joan McDuffie, M.A.
Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
Elizabeth Brown, MD, M.S.H.P.
Division of Medicaid and Medical Assistance, State of Delaware Department of Health and Social Services
ABSTRACT
This study draws upon data from two databases: claims and encounters that were reimbursed by the state’s Division of Medicaid and Medical Assistance (DMMA) and the Homeless Management Information System (HMIS) database that collects homeless services data on individuals experiencing homelessness. Records from both sets are matched to identify 838 adults who both experienced homelessness and were Medicaid eligible in 2019, and to select, through propensity score matching, an equal set of control observations who were similarly Medicaid-eligible but had no record of homelessness. Outcomes are compared based upon scores on the Charlson Elixhauser Comorbidity index, incidence of substance use disorder, inpatient, emergency department, and outpatient visits, and inpatient, emergency department, and outpatient costs. Using ordinary least squares regression models, we estimate homelessness (as indicated by use of homeless services) to be associated with excess costs of $4,611 (non-chronic homelessness) to $5,218 (chronic homelessness) per person over the course of 2019, compared to similar Medicaid enrollees who were housed.
ACKNOWLEDGEMENTS
We gratefully acknowledge support for this project provided from the Delaware Division of Medicaid and Medical Assistance (DMMA), and data was provided by DMMA (Medicaid) and Housing Alliance Delaware (homeless services use). The content is solely the responsibility of the authors and does not necessarily represent the official view of the Delaware Division of Medicaid and Medical Assistance or the Housing Alliance Delaware.
INTRODUCTION
Homelessness has long been associated with poor health. Research has documented how health problems, including but not limited to mental health and substance abuse-related morbidities, have been catalysts of housing instability.1 Health and behavioral health conditions often cause economic problems, difficulty maintaining and securing employment, loss of familial and social supports, and other disruptions that can exacerbate unstable housing conditions leading to experiencing homelessness.2 Conversely, homelessness intensifies health conditions as the absence of housing creates barriers to accessing to medical care, imposes conditions that can cause poor health conditions, and exposes people to trauma, stress, violence and other factors that are deleterious to good health.3
Worsened health conditions and lack of access make it likely that, once an individual experiencing homelessness accesses health care, their presenting conditions will have become more acute and require more extensive care. This is then reflected in increased health care expenses associated with health care services received.
This has been demonstrated by numerous studies that have examined administrative records maintained by healthcare systems and third party payors and that have compared groups experiencing homelessness with comparable groups of housed controls.4 These studies have typically demonstrated substantial costs associated with homelessness, and decreased costs incurred after people transition from homelessness to permanent housing. Such studies illustrate a collateral benefit of addressing and ameliorating homelessness in its potential to mitigate poor health outcomes and reduce demands for health care and its corresponding costs.
In this study, we examine associations between homelessness and healthcare use in Delaware through matching records in the statewide homeless management information system (HMIS) database with the state’s Medicaid claims and encounters database. This adds to the body of research on the impacts of homelessness on health and is the first such study specific to outcomes and costs in Delaware. As such, it provides specific findings that can be of assistance in coordinating health care and housing responses to unstable housing and homelessness.
METHODS
In this study, we draw upon data from two databases: one containing the claims and encounters that were submitted to the state’s Division of Medicaid and Medical Assistance (DMMA); and the HMIS database that collects homeless services data on individuals experiencing homelessness and is maintained for the State of Delaware’s homeless continuum of care (COC) by
18 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.005
Housing Alliance Delaware (HAD). Records from both sets are matched to identify people who are both homeless and Medicaid eligible in 2019, creating an integrated dataset with indicators related to homelessness status and health utilization. The project was reviewed and approved by the University of Delaware’s Institutional Review Board (1647700-2).
The study group contains records for people who received three types of homelessness-related housing in 2019: temporary housing consisting of either shelter or transitional housing (n=490), rapid rehousing, where people receive housing with time-limited rental and services supports (n=302); and permanent supportive housing, (n=46), where people receive ongoing rental voucher and case management assistance. Of the 838 people in the study group, 190 (23%) were identified as “chronically homeless,” operationalized by the U.S. Department of Housing and Urban Development (HUD) as “a single individual (or head of household) with a disabling condition who has either: Experienced homelessness for longer than a year, during which time the individual may have lived in a shelter, Safe Haven, or a place not meant for human habitation; or experienced homelessness four or more times in the last three years” for a combined time of at least twelve months.4 Given the extensive time of homelessness experienced among those in this subgroup, their use of Medicaid-reimbursed services were examined separately from the others in the study group.
The Medicaid records for those in the study group are compared to a set of matched controls who were Medicaid eligible with no record of homelessness during 2019. This control group was selected using propensity score matching (PSM) based non-health related characteristics available in the Medicaid records. PSM, a quasi-experimental method that is commonly used for studies similar to this,5 allows us to match each homeless individual with a comparable control group of similar characteristics. The characteristics that were used to match the control group include age, race and ethnicity, sex, county, and Medicaid eligibility category.
The study and control groups are compared on the basis of their health status, their services use, and the associated reimbursement costs, listed in the Medicaid claims, incurred through their health care use. We use the Charlson-Elixhauser Comorbidity Index as a means to assess health status. The Charlson-Elixhauser index was developed to assess mortality risk among elderly populations, and often used as a proxy for general health status. This index generates a weighted comorbidity score based upon a combination of 20 different health conditions. A score of 0–1 indicates low comorbidity and a score of 2 or higher is considered high comorbidity.6,7 Along with frequencies of the individual component conditions of the Charlson-Elixhauser Comorbidity Index, we also report diagnoses related to substance use, which is often higher among homeless populations and may account for differences in health care use when compared to housed populations. Costs are used as a means to summarize and standardize Medicaid-reimbursed health care use across different modes of care (inpatient hospital, outpatient, emergency department, etc.) and as a measure by which to estimate additional costs to Medicaid associated with homelessness. We produce the latter estimate through fitting a basic ordinary least squares regression model that controls for comorbidity, substance use, and other factors that may also account for differences in health care use between housed and homeless populations.
Missing: 3-non-Homeless; 6-Homeless Chi-Square: 1.0351 p=.7927
Chi-Square: 1.2678 p=.9893
^MAGI is defined as Modified Adjusted Gross Income
19
Non-HomelessHomeless #%#% Age Groups 18 to 29 170 20%17120% 30 to 39 202 24% 202 24% 40 to 49 15318%15418% 50 to 59 21726%21626% 60 & older 9611%9511% Total 838100%838100% Chi-Square: .0137 p=1.0000 Sex Female 45554%45654% Male 38346%38246% Total 838100%838100% Chi-Square: .0024 p=.9609 Race Black 45454%45654% White 343 41% 342 41% Other 41 5%405% Total 838100%838100% Chi-Square:
County Kent 240 29%23829% New Castle 481 58% 478 57% Sussex 11414%11614% Total 835100%832100%
Table 1. Frequency Distributions of Homeless and Comparison Groups.
.0182 p=.9909
Medicaid Coverage Expansion 45254%44853% MAGI^ (Parent/Caretaker Medicaid MAGI-based) 19223%19323% SSI-Disability13316%13116% MAGI^ 121%182% SSI-Aged 152%152% Pregnancy Cov.162%152% Other 182%182% Total 838100%838100%
RESULTS
Frequency distributions of the homeless and comparison groups on the characteristics used for the PSM procedure are shown in Table 1. Chi-square analysis shows no statistically significant differences between the groups on these selection criteria. The table also shows some basic characteristics about the composition of the two groups. In both groups, around a quarter of the study population falls in the 30-39 age group (24%), while another rough quarter (26%) falls in the 50-59 age group. Slight majorities of both groups are female (54%), Black (54%), live in New Castle County (58%) and, in terms of eligibility for Medicaid coverage, fall in the expansion category (100% to 138% of the federal poverty line) (54%).
Table 2 shows results related to the Charlson Elixhauser Comorbidity index and the incidences of substance use disorder diagnoses, which are not included in calculating the index scores. These give some basic indications of the health of the two groups. Looking first at the overall index scores indicates that the homeless group, and particularly the chronically homeless subgroup, have substantially higher levels of comorbidity than the controls. At the extremes, 51% of the controls had a 0 score, while only 30% and 18% of the overall homeless group and chronically homeless subgroup, respectively, had the healthiest score. On the other end, while only 7% of the control group had scores of 5 and over, 13% of the overall homeless group and 19% of the chronically homeless had such scores. Among substance use diagnoses, twice as many of the overall homeless group, 35% compared to 15%, had at least one dependency diagnosis, and 43% of the chronically homeless subgroup had Medicaid records of some dependency diagnosis. In contrast to these stark differences, the differences in frequencies between groups for incidences of the individual comorbidity components did not, in all but a few cases, differ substantially. Only four diagnoses: alcohol abuse and pulmonary circulation disorders, showed statistically significant differences.
Table 3 shows Medicaid-reimbursed health care costs, both total and broken down by the primary types of health care service: inpatient hospitalization, emergency department (ED), and outpatient. For each service category, substantially higher proportions of the homeless group, and particularly the chronically homeless subgroup, make up the higher cost groupings. Conversely, much higher proportions of the control group show zero costs in each service category. For inpatient, 4% of the control group had $15,000 in costs or higher, while over 3 times of the chronic homeless group (13%) and exactly 3 times of the non-chronic homeless group (12%) fell into this category. 86% of the control group had no inpatient costs, while only 65% each of the chronic and non-chronic groups had held at $0 for inpatient costs. Twelve percent of the control group had over $300 in ED costs, compared to 46% for the chronic group and 38% for the non-chronic group. The control group holds the highest proportion of $0 for ED costs (62%) and is followed by the chronically homeless group at 27% and the non-chronic homeless at 31%. Considering outpatient costs, 12% had costs above $10,500 in the control group, with 20% of the chronic group and 13% of the non-chronic homelessness group in this category. For the $500 or below outpatient category, the control group had 35% of clients, the chronic 13%, and the non-chronic 16%. Similar trends are shown with looked at the distribution
Notes: Cancer and dementia diagnoses, which are component in calculating the Charlson-Elixhauser score, are not reported due to insufficient numbers in cell sizes (n<10) in both all homeless and control groups to maintain anonymity. Substance use diagnoses are not Charlson-Elixhauser score components. Chi-square test of difference between all homeless and control groups yield: * - p-value < 0.05; *** - p-value < 0.001. “Other Substance Dependence” includes dependencies on stimulants, sedatives, hallucinogens, inhalants, and other psychoactive substances.
20 Delaware Journal of Public Health - June 2023
NonHomeless (N=838) All Homeless (N=838) Chronic Homeless (N=190) Charlson-Elixhauser Comorbidity Score*** 0 51% 30%18% 1-2 31%38%44% 3-4 11%18%19% 5+ 7%13%19% Charlson-Elixhauser Comorbidity Score Diagnosis Components Alcohol Abuse* 19%23%22% Cardiac arrhythmia21%22%20% Chronic pulmonary disease 8%10%10% Coagulopathy 4%5%4% Complicated diabetes 13%13%14% Congestive heart disease 8%9%9% Deficiency anemia19%19%17% Fluid and electrolyte disorders 21%23%21% Hemiplegia 2%2% n/d HIV/AIDS 2%3%1% Hypertension 42%42% 44% Liver disease 13%14%13% Peripheral vascular disease 8%8%6% Behavioral conditions 25%29%33% Pulmonary circulation disorders*** 1%4%3% Renal failure 5%5% n/d Tumor 6%4%4% Weight Loss 2%2% n/d Substance Use Diagnoses Opioid dependence of any type*** 14%31%39% Cocaine dependence*** 3%13%13% Other substance dependence*** 1%5%8% Opioid, Cocaine, or other dependence*** 15%35%43%
Table 2. Charlson Elixhauser Comorbidity Results and Substance Use Disorder Diagnoses
Chi-square test of difference between all homeless and control groups yield: * - p-value < 0.001.First two cells in outpatient and total cost sections of the chronically homeless column are combined due to insufficient numbers in dataset. Total Cost represents sum of inpatient, emergency department, and outpatient costs.
of the sum (total inpatient, emergency, outpatient): 9% of the control group had $16,000 or more in cost, with 26% of the chronic group and 24% of the non-chronic homeless group in the same category. Forty-three percent of the control group had $0 for summed total costs, with 17% of the chronic group with $0 and 24% of the non-chronic.
Table 4 shows results of two ordinary least squares regression models with total costs as the dependent variable, logged in the first model and unlogged in the second. To safeguard against disproportionate impacts of individuals with exceedingly high Medicaid costs on the results, 83 outliers (those with total services costs in the highest 5%) were omitted from the analysis. After controlling for significant cost variation among different types of Medicaid eligibility, significantly lower costs for the male category and significantly higher costs for people with substance use diagnoses of dependency and higher comorbidity scores, the estimated, adjusted cost associated with homelessness is between $4,611 (non-chronically homeless) and $5,218 (chronically homeless) per person, when compared to the non-homeless control group.
DISCUSSION
This study examined people with records of homeless services use who were also eligible for Medicaid in 2019, and compared them to a set of controls who, as a group, were very similar in terms of demographics, type of Medicaid eligibility, and county of Medicaid receipt. The homeless group had a higher level of comorbidity, as measured by the Charlson-Elixhauser Comorbidity Index, and a substantially higher prevalence of dependency diagnoses for substance use. People in the homeless group had consistently higher levels of Medicaid services use overall. This translated into higher mean costs, which remained after adjusting for the various measures that were available in the Medicaid data. All in all, based on these data we estimate that homelessness (as indicated by use of homeless services) is associated with costs of $4,611 (non-chronic) to $5,218 per person over the course of 2019.
These findings are consistent with findings in other states showing both that homelessness is associated with poorer health and increased costs for state Medicaid programs. Although from this study we cannot definitively state that homelessness caused an individual to be sicker or the sickness caused homelessness, we have found that individuals who are homeless are sicker and have higher expenditures in Medicaid. Implicit in these findings is what has been shown in other states, namely that expenditures on getting people rehoused, and especially people who meet criteria for chronic homelessness, can be offset, at least in part, by savings from reductions in Medicaid costs.
Research has shown that homelessness creates new health problems and worsens existing ones. Health issues among people who are homeless are often a complex combination of physical, mental health, substance use, and social problems. Housing and health care work best together and are critical to preventing and ending homelessness. Health care services have a greater impact when a patient is stably housed.8
While expanding the availability of housing for homeless populations should not be contingent upon potential cost offsets, the promise of such savings could facilitate the financing of new housing.
This is one of only a few Delaware-specific studies that have been able to examine the collateral impacts of homelessness upon a related services system. Similarly structured studies looking at the impacts of homelessness on criminal justice, child welfare and mental health systems may reveal further cross-system services use dynamics that could inform and facilitate services interventions.
LIMITATIONS
This study has limitations. Gaps in CMIS data coverage diminished the size and representativeness of the study group, and limited our ability to assess relationships between time homelessness is experienced and Medicaid use. The unavailability of social security numbers may have limited the accuracy of the matches, although manual inspection of the matches indicates that those that matched appeared accurate. While these limitations may have reduced the ability of the study group to be representative of the entire adult homeless population, it was a large enough group in itself to merit assessing differences in health case. However, due to the nature of the cross-sectional data, a direction of causality cannot be claimed. Researchers are unable to determine if clients are sicker when they become homeless, or if becoming homeless makes them sicker.
21
NonHomeless N=802 Homeless N=791 Chronic Homeless N=173 Inpatient Cost* $0 86% 65% 65% $1-$14,999 10% 23% 22% $15,000 or more 4% 12% 13% Emergency Department Cost* $0 62% 31% 27% $1-$300 27% 32% 27% $301-$699 9% 23% 26% $700 or more 3% 15% 20% Outpatient Cost* $0 16% 7% 13% $1-$500 19% 11% $501-$4500 50% 49% 44% $4501-$10,500 9% 21% 24% $10,501-$15,999 3% 7% 12% $16,000 or more 4% 6% 8% Total Cost* $0 15% 6% 17% $1-$1,000 28% 18% $1,001-$5,000 34% 31% 32% $5,001-$15,999 13% 22% 25% $16,000 or more 9% 24% 26%
Table
3. Medicaid Reimbursed Health Care Costs
Table 4. OLS Cost Analysis
CONCLUSION
This report shows costs of homelessness borne by Medicaid, and suggests that Medicaid expenditures focused on addressing homelessness can potentially be offset by reduction in health care provision. This study also suggests that homeless prevention measures such as rental assistance, provided at an unprecedented scale through the Delaware Housing Assistance Program, has hidden cost savings through reduced Medicaid expenditures for recipients who otherwise might have become homeless. This is an example of the wide range of further research that can be done to confirm and to better understand the dynamics of the cost savings that are found here.
Ms. Nescott may be contacted at eplynch@udel.edu
REFERENCES
1. Cantor, J. C., Chakravarty, S., Nova, J., Kelly, T., Delia, D., Tiderington, E., & Brown, R. W. (2020, March). Medicaid utilization and spending among homeless adults in New Jersey: Implications for Medicaid-funded tenancy support services. The Milbank Quarterly, 98(1), 106–130. https://doi.org/10.1111/1468-0009.12446
2. Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y., & Alvarez, K. (2018, September 17). Social determinants of mental health: Where we are and where we need to go. Current Psychiatry Reports, 20(11), 95. https://doi.org/10.1007/s11920-018-0969-9
3. Office of the Assistant Secretary. (2021). health conditions among individuals with a history of homelessness. HHS Office of Planning And Evaluation Office Of Behavioral Health, Disability, And Aging Policy. ASPE Research Brief. https://permanent.fdlp.gov/gpo184594/HomelessHistRB.pdf
4. Koh, K. A., Racine, M., Gaeta, J. M., Goldie, J., Martin, D. P., Bock, B., . . . Song, Z. (2020, February). Health care spending and use among people experiencing unstable housing in the era of accountable care organizations. Health Affairs (Project Hope), 39(2), 214–223. https://doi.org/10.1377/hlthaff.2019.00687
5. National Alliance to End Homelessness. (2015, Dec). Here’s what you need to know about HUD’s new chronic homelessness definition. Retrieved from:
https://endhomelessness.org/blog/heres-what-you-need-to-knowabout-huds-new-chronic-homelessness-definition/
6. Brennan, K., Buggs, K., Zuckerman, P., Muyeba, S., Henry, A., Gettens, J., & Kunte, P. (2020). The preventive effect of housing first on health care utilization and costs among chronically homeless individuals: New evidence using propensity score analysis. Massachusetts Blue Cross Blue Shield. Retrieved from: https://www.bluecrossmafoundation.org/sites/g/files/csphws2101/ files/2020-12/Housing%20First_report_FINAL.pdf
Notes: 83 outliers (those with total services costs in the highest 5%) were omitted from the analysis. Prior to dropping these outliers, the skewness was 7.7 and the kurtosis was 88.4 indicating that the outliers were impacting the mean. After the outliers were dropped, skewness was 1.8 and kurtosis was 2.9, more within an acceptable range. Of the 83 clients dropped: 43% were non-homeless and 57% were homeless. This brings the total N to 1593. The R-Square is 0.1173 (logged) and 0.1542 (unlogged). ^ MAGI is defined as Modified Adjusted Gross Income
7. Gagne, J. J., Glynn, R. J., Avorn, J., Levin, R., & Schneeweiss, S. (2011, July). A combined comorbidity score predicted mortality in elderly patients better than existing scores. Journal of Clinical Epidemiology, 64(7), 749–759. https://doi.org/10.1016/j.jclinepi.2010.10.004
8. National Council on Healthcare for the Homeless. (2019). Homelessness & health: What’s the connection? Retrieved from: https://nhchc.org/wp-content/uploads/2019/08/homelessness-andhealth.pdf
22 Delaware Journal of Public Health - June 2023
Covariate Parameter Estimate Pr > |t| Parameter Estimate Pr > |t| Cost (logged)Cost (unlogged) Homeless Status Homelesschronic 2.66<.00015218<.0001 Homelessnot chronic 1.74 <.00014611<.0001 Non-homeless (reference) 0000 Comorbidity Score 0.05 0.4900 4310.0071 SUD Diagnosis Diagnosis present 3.30<.00019031<.0001 No Diagnosis (reference) 0000 Medicaid aid category MAGI^ (Parent/ Caretaker Medicaid MAGI-based) 0.03 0.9524 -30490.0022 SSI-Disability 1.110.02814498<.0001 SSI-Aged 0.76 0.579112490.6679 MAGI^ 0.81 0.53626950.8019 Pregnancy coverage 3.330.008999920.0002 Expansion (reference) 0000 Age 0.05 0.0015570.0630 Gender Male -2.51<.0001-17090.0359 Female (reference) 0000 Race/Ethnicity Black, non-Hispanic -0.24 0.5181 -3440.6579 Other race -5.110.0480 -37550.4921 Hispanic -0.230.7969-14230.4437 White, nonHispanic (reference) 0000 County Kent -0.07 0.8596 21630.0099 Sussex 0.17 0.7418 511 0.6440 Unknown county -2.140.4082-54080.3240 New Castle (reference) 0000
June 2023
The Nation’s Health headlines
Online-only news from The Nation’s Health newspaper
Stories of note include:
Changes to race, ethnicity data collection will impact health
Kim Krisberg
Private equity’s hold on health care growing, raising concerns
Mark Barna
Public support for LGBTQ+ rights high, even as restrictions grow
Teddi Nicolaus
State lawmakers leading new charge for single-payer care
Mark Barna
For the best vacation, don’t skip out on health and safety
Teddi Nicolaus
New APHA Press book a public health guide to policy engagement, advocacy
Mark Barna
APHA 2023 registration, housing open June 5

Michele Late
APHA toolkit helps students make connection between health, climate

Mary Stortstrom
https://www.thenationshealth.org/
23
HIGHLIGHTS FROM The NATION’S HEALTH A PUBLICATION OF THE AMERICAN PUBLIC HEALTH ASSOCIATION
Evaluating Approaches to Linking Evictions Records: Assessing the Feasibility of Research with Integrated Data
J. J. Cutuli, Ph.D.
Senior Research Scientist, Nemours Children’s Health
Mary Joan McDuffie, M.A.
Policy Scientist, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
Erin Nescott, M.S. Associate Policy Scientist, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
ABSTRACT
Objectives: This study investigates different approaches to integrating evictions data with Medicaid and homeless shelter utilization records at the individual level for the state of Delaware. We especially focus on evaluating the feasibility of creating an integrated dataset focused on children and adolescents through different approaches to matching. Methods: We attempt to link existing statewide records on evictions, Medicaid, and shelter from 2017-2019. We first compare direct match and probabilistic match approaches to linking evictions and Medicaid records, and then incorporate shelter records. Finally, we consider a limited set of characteristics relevant to potential future public health research among children who experienced eviction, had a shelter stay, and were enrolled in Medicaid. Results: Direct matching resulted in a lower match (14%) rate than probabilistic matching (22%) of eviction records to Medicaid data. Homeless shelter records had a high match rate to Medicaid records, even when using a direct match (75%). A sizeable subset of children (n=216) were linked across the three data sources, though this was from a small percentage of cases in the evictions data. Among this subset of children, most (71%) were enrolled in Medicaid in all three years considered by this study and Black children were greatly overrepresented (75%). Conclusions: Integrating evictions records with other health and human service data involves a number of challenges. Probabilistic matching yielded a considerably higher number of matches after manual review, resulting in a possible study sample of children who have experienced eviction, a homeless shelter stay, and were enrolled in Medicaid. Strategies to increase the match rate for eviction records through using records from other, more universal services may be necessary for investigations that require more comprehensive coverage of the population.
ACKNOWLEDGEMENTS
Research reported in this project was supported by the Institutional Development Award (IDeA) from the National Institute of Health’s National Institute of General Medical Sciences under grant numbers P20GM103446 and P20GM144270. We thank the Delaware Division of Medicaid and Medical Assistance for the use of the Medicaid claims and encounter data, Housing Alliance Delaware for providing access to the Community Management Information System data, and the Delaware Justice of the Peace Court for providing eviction data. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Delaware Division of Medicaid and Medical Assistance, Delaware Justice of the Peace Court, or Housing Alliance Delaware.
INTRODUCTION
This study considers the feasibility of matching evictions records to Medicaid and shelter use administrative records at the individual level for families with children and youth. Integrated datasets are an important tool for researchers in public health, healthcare delivery, and varied health and human service arenas. However, linking records requires that a set of relatively unique individual-level identifier variables be present across sources, commonly first name, last name, date of birth and, sometimes, social security number. This presents a challenge for researchers interested in linking evictions records with others: evictions data often only include the first and last name of the lease holder(s), the property address, and a small set of other details related to the eviction process. We investigate data match-rates between sources for children with different experiences of forced housing disruption (homeless shelter stay, eviction without a homeless shelter stay, and neither). Our goal is to quantify the match rate using different linkage approaches.
24 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.006
THE IMPORTANCE OF RESEARCH ON CHILD, YOUTH, AND FAMILY EVICTION AND HOMELESSNESS
Relatively little is reliably known about families who experience eviction, though studies of families and youth who experience homelessness suggest considerable risk for becoming disconnected from services and for poor outcomes. This underscores the importance of developing reliable methods to further research on family eviction. Crises that involve residential mobility challenge families to stay connected or reconnect to health care,1 early childhood programs,2 school,3 and a host of other formal and informal community supports.4 Homelessness and eviction are already viewed as prevalent issues though the economic consequences of the COVID-19 pandemic threaten great increases. Over 300,000 minor children and teens stay in U.S. homeless shelters each year,5 and about 500 specifically in Delaware.6 Children and minor teens in shelter have higher rates of chronic disease, acute disease, and emergency department utilization.7–9
Much less is known about children in families who are evicted, including reliable estimates of their number.10,11 Analyses linking evictions to census information suggest risk for very low birth weight and infant mortality,12 though other pediatric health outcomes are uninvestigated. Eviction or a move to shelter disproportionately involve families in deep poverty, women, and those from racial minority backgrounds.11,13 These disruptions may disconnect children from primary healthcare providers while forcing parents to prioritize competing basic needs. Interagency and inter-system collaboration may help maintain healthcare connections during crises, but there is essentially no rigorous evidence for children who experience eviction and homelessness.
PAST ATTEMPTS AT LINKING EVICTIONS RECORDS WITH OTHER DATA
Few published studies have attempted to integrate evictions records with other health and human service records to investigate impacts on children, though integrated data approaches that include shelter and other housing intervention records are much more common.14–16 Focusing on linking methodology, Collinson and Reed provide an early and mostdetailed description of their linking procedure.17 This group linked housing court records on eviction filings (containing only address, date, and first and last name) to a large database containing recipients of multiple public benefits in New York City (containing first and last name, address, and dates benefits were received), but only for cases where benefits receipt predated the eviction record. They cleaned the identifiers (e.g., removing non-numeric characters and aliases from names in the evictions data) and geocoded addresses to the parcel level to account for multiunit properties at the cost of precision. After processing and blocking the data, they engaged a matching algorithm that prioritized exact matches before probabilistically linking non-exact matches based on best-available name and geocode combinations past a predefined minimum threshold. This resulted in matching 40% of evictions records to benefits records, though this match rate increases to 57% when benefits records
are allowed to occur before or after the eviction record date. Though a 40% match rate seems low and would likely contribute to bias, the authors note that a majority of actual eviction cases (filings that proceeded to eviction) are contained in the 40% of filings that matched.
A more recent study by Schwartz and colleagues linked New York City eviction filings to New York State Medicaid records.18 The reported linking procedure is less detailed. The study team first geocoded each eviction filing to the parcel level and then identified patients as evicted if their most recent Medicaid enrollment information (as of the eviction date) matched the unit number and building of an eviction. Name was not considered in the match. This yielded 6,922 Medicaid recipients identified as having been evicted out of 20,810 total evictions, though it is not clear how many Medicaid recipients shared a household. At best, the match rate for evictions from this approach was about 33.3%. Neither of the above studies attempted to assign eviction records to children. This presents an additional challenge because children are not listed on eviction records. Instead, children must be linked to parents/caregivers using other data sources and the parents/caregivers must then be matched to the eviction records. This also implies two—instead of one—dynamic indicators: addresses can change as people move and family structures can change through separation or loss. Richter and colleagues linked eviction filing records to a benefits database containing Medicaid and other program records (analogous to Collinson & Reed17), though their method ultimately extends evicted-status to children connected to adults in the benefits data.19 In an attempt to contain the possibility of address and family structure records being out of date, they limited consideration to benefits data that occurred within six months prior to each eviction record. This group geocoded addresses in both datasets to the census block level, and used Soundex (phonetic indexing) to match names and addresses. This resulted in a match rate of 47.4% of eviction filings. Finally, though not focused on evictions, another effort attempted linkage on similar adult identifiers (guardian first and last name, address) found in education records from a school district, connecting data on adults to infer the presence of risk in the lives of children.20 The goal was to match guardians from the education data to an existing integrated data system that contained all hospital-based healthcare contacts, various population-wide public-records datasets that contain, at least, names and addresses (e.g., voter registration records), and other sources. This effort standardized addresses using a geocoding service. This process successfully linked 67% of guardians in the education records through an exact/deterministic match, and another 14% matched with an acceptable level of confidence through probabilistic matching (81% match rate, overall).
THE CURRENT STUDY
This study aims to describe the degree to which a linking protocol integrates data from Medicaid records, shelter utilization data, and court records ordering eviction at the household level. Past research matched between 33.3% and 47.4% of eviction filings at an individual level. We seek to answer a fundamental question: What is the match rate when trying to link eviction and Medicaid records using approaches that rely on name and address?
25
METHODS
We attempted to link records at the individual level from three different datasets to reflect the number of children who were evicted, those who stayed in a homeless shelter, and, for future analyses, have access to indicators of health and health care utilization using Medicaid records. This study considers all records from 2017 through 2019. All linkages were performed at the Center for Community Research & Service (CCRS) by policy analysts with individual business associate agreements with the state of Delaware granting permission to use the data. The project was reviewed and approved by the Delaware Division of Medicaid and Medical Assistance and the Institutional Review Boards of the University of Delaware and Nemours Children’s Health. All analyses were done on CCRS’s encrypted drive to safeguard the data and individual data has not been released.
EVICTION RECORDS
The Justice of the Peace court system maintains a publiclyavailable database of eviction filings in Delaware. Records included dates of filings and all listed defendants (max: 9 defendants per filing). Available identifier variables were first name, last name, sex, and address. Addresses were cleaned (e.g., removed nonresidential addresses) and geocoded to the address level using ARCGIS (92% of addresses were successfully geocoded), yielding longitude and latitude coordinates. We removed duplicate and repeated eviction filings (e.g., when additional filings contained the same defendant at the same address).
HOMELESS SHELTER RECORDS
Individual-level administrative records describe stays in homeless shelters for individuals and families in Delaware. These data come from the Community Management Information System (CMIS) which functions as the Homeless Management Information System for Delaware. Records contain a family code that allowed us to cluster individuals into family units. CMIS is managed by Housing Alliance Delaware.21
MEDICAID RECORDS
Analyses consider Medicaid Client data. These data were approved for use and made available through the Medicaid research partnership between the Delaware Division of Medicaid and Medical Assistance, the University of Delaware (UD) Center for Community Research and Service, and the UD College of Health Science. Data Client addresses were geocoded to the address level using ARCGIS (89% of addresses were successfully geocoded). Medicaid data also permit individuals to be clustered into families, allowing us to identify any minor children based on
Medicaid household codes. We applied a logic based on ages to demarcate children (minors under 18 years old) and guardians (e.g., those more than 15 years older than each minor) for cases linked to eviction records. Medicaid eligibility in Delaware is based on a combination of factors including household income and composition, and health status subject to income limits.22
LINKAGE PROCEDURES
We used Link Plus23 to link Medicaid, eviction, and homeless shelter records, first using direct matches on the complete identifiers (defendant first name, last name, sex, geocoded address). Direct matching requires the data to match exactly for records to be linked. We repeated the match starting with the direct-match cases and then adding additional matches using a probabilistic matching method on the same set of identifiers, using only the first three letters of the first and of the last names Probabilistic matching permit differences in field values to accommodate errors in data entry, alternate spelling of names, nicknames, or nonstandard abbreviations, for example. All matching involved a final step of manual review. CCRS staff reviewed each match to ensure it was a true match without any apparent logical errors. All analyses were completed by CCRS staff and we report linkage results for Medicaid and eviction records in aggregate form. We then attempted to link homeless shelter records with Medicaid records using a more-standard set of identifiers (first name, last name, birth date, and sex) and then integrating all three datasets.
RESULTS
Linkage rate details for matches between eviction and Medicaid records are provided in Table 1. Overall, about 14% of defendants with evictions filings matched to the Medicaid records using direct matching. This rate increases to 22% when using probabilistic matching and subsequent manual review of matches. This represents nearly 2,500 additional matches.
We linked homeless shelter data with Medicaid data by first name, last name, birth date, and sex via direct matching. There were 6,368 adult clients who had a shelter stay; 4,746 or 75% were matched to Medicaid records.
The linkage was then made between the Medicaid-Homeless data set and the Evictions-Medicaid data set by the Medicaid ID. First considering results from a direct linkage approach, there were 100 individuals who were present in all three datasets (2% of the linked Evictions-Medicaid data set). The household identifier was used to extract anyone living in the household of the eviction defendant. This resulted in 270 full benefit covered Medicaid clients who were in a household that had evictions claim and someone who experienced homelessness.
26 Delaware Journal of Public Health - June 2023
Eviction filings Unique Persons Direct Match Evictions-Medicaid Probabilistic Match Evictions-Medicaid Year N n % n % 2017 11,930 1,225 10% 1,749 15% 2018 11,924 1,570 13% 2,578 22% 2019 11,005 1,259 11% 2,310 21% All Years 31,151 4,337 14% 6,821 22%
Table 1. Match Rates by Approach Linking Evictions to Medicaid Records.
The same records were matched using a probabilistic linkage approach: There were 168 individuals who were present in all three datasets (2.46% of the linked Evictions-Medicaid data set), from 167 unique households. We then used the household indicator to identify other members living in the household as the eviction defendant. This resulted in 440 Medicaid clients who were in a household that had eviction claims and lived with or was someone who stayed in a homeless shelter. About half of these individuals were children and teens under 19 years old (See Table 2). Considering just the children, nearly three-quarters (74%) received Medicaid for at least one month in each of the three years of data considered in this study (2017-2019), the vast majority (71%) were Black, non-Hispanic race and ethnicity, and a slight majority (53%) were male.
There are several possible explanations for the lower match rate. First, past research used datasets containing enrollment in multiple benefit programs that included Medicaid as well as others (e.g., SNAP, TANF). It is possible that some individuals enrolled in these other programs and their information was not available to our match in Delaware, potentially lowering our match rate compared to other localities where this information was available. Furthermore, the reliance on Medicaid records in Delaware also means that persons who do not qualify could not be successfully matched (e.g., those without low income, without a child under 18 in the household and not blind, disabled or with a disabled household member, or over age 65). This is less a concern for the current study interested in matching families, and multiple other studies on evictions in Delaware suggest that families and those with low income appear to be disproportionally subjected to eviction filings.21,24 However, it might further help explain the relatively lower match rate since benefit programs such as SNAP (available in past research involving match rates) allows single adults to participate. Without these additional records, the match rate in Delaware would underperform as it will fail to link evicted persons who are not enrolled in Medicaid (e.g., single adults).
DISCUSSION
Different linkage techniques, different types of data, and differences in available identifiers have sizeable implications for match rates when integrating records across sources. This study was interested in determining the match rates when linking records from evictions, Medicaid, and shelter records across Delaware. Our goal was to evaluate the feasibility of future integrated data approaches to testing associations between evictions, stays in family shelter, and pediatric health care. Compared to deterministic matching techniques alone, probabilistic matching of eviction and Medicaid records resulted in a higher number of matches that remained after manual review. Though, overall match rates were low. Meanwhile, the match rate between shelter and Medicaid records was high, even when using a more conservative direct matching approach.
INTEGRATING EVICTION, MEDICAID, AND HOMELESS SHELTER RECORDS
Our attempts to link eviction and Medicaid records yielded match rates of 14% for a direct match approach and 22% for a probabilistic match approach. It is not surprising that probabilistic matching matched a higher number of cases since probabilistic linkage allows for differences in the fields that identify cases, such as misspellings or other data entry errors, nicknames and abbreviations, or other differences. However, only locating 22% of evictions cases in the Medicaid data results in a match rate that is below what has been typically found in other studies (albeit few in number), which generally match between 33-50% of evictions filings.17–19
Building on this theme, the match rate will incrementally improve as increasingly universal datasets are included in the match. This is evident in past research linking guardians in school records to health, human service and other publicly available records and using nearly the same set of identifiers (first and last name, address) and similar linkage procedures. This yielded a very high match rate (81%.20) In that study, health records were more comprehensive as they included all hospital-based contacts (e.g., those with private insurance or no insurance) as well as records not tied to program eligibility or service delivery (such as voter registration records). Higher match rates are possible with more comprehensive datasets.
An additional consideration is how the current study differed from past research in representing addresses. We took a relatively more-precise approach of geocoding x,y coordinates, which also would contribute to a more conservative match compared to other studies that geocoded to larger geographic units (e.g., parcel or census block17–19). This decision has implications for the likely sensitivity (true positive rate) and specificity (true negative rate) that would result from the match. Furthermore, actual match would fail if the Medicaid address data were not accurate (e.g., not current) as of the time of the eviction.
We achieved robust linkage (75%) between homeless shelter and Medicaid records, even when using the more conservative direct matching approach. This high match rate may be an example of the considerations described above: Shelter services frequently involve case management services, which can provide a direct pathway to Medicaid enrollment (and inclusion in the Medicaid data) for families in shelter. Also, shelter records contain identifiers that are more commonly used: first name, last name, and date of birth. This avoids the complications and potential pitfalls of different approaches to matching on address.
Despite the low-match rate for evictions and Medicaid data, we were able to construct a sizeable study group of 216 children who appeared in all three datasets. Importantly, 71% of these children were enrolled in Medicaid for at least a portion of
27
Age Group N % Birth - 5 84 19% 6 - 10 65 15% 11 - 18 67 15% 19 - 30 78 18% 31 - 50 110 25% 51+ < 35 < 10% Missing < 10 < 2% Total 440
Table 2. Individuals Indicated by All Three Data Sources by Age Group
each year considered in this study. This suggests an adequate opportunity to test hypotheses on the pathway from eviction to shelter for families, and consider patterns of health and healthcare contained in Medicaid claims and other data. Consistent with past research,10 children from Black race groups were drastically overrepresented (75%) in this group, also suggesting the possibility of important programs of research focused on addressing inequity.
LIMITATIONS
This study has important limitations. First, it is primarily an analysis of record linkage and was not thoughtfully designed to rigorously test any other hypothesis or describe any other substantive phenomenon. We urge caution in reading more into this study than originally intended.
Second, our approach does not permit a definitive evaluation of the sensitivity (true positive rate) and specificity (true negative rate) of different linkage methods. Simulation-type studies, for example, allow investigators to manipulate particular aspects of the data to determine sensitivity and specificity of each method under different conditions while the true solution is known. Instead, we explored match rates using different approaches to real-world data where the true solutions are not known with certainty. While the probabilistic method produced a higher number of matches, and these matches were subjected to manual review for confirmation, we cannot make any strong claims about the true positive rate, and less so about the true negative rate. In addition, our match rates can only be as complete as the datasets that we use to inform them. For example, some private shelters and public hotel/motel voucher programs did not contribute to Delaware’s CMIS and, therefore, would not be included in the homelessness data considered here. This coverage gap leaves open the possibility that people we identified as evicted could have also received homeless services that were unrecorded in CMIS. Administrative data systems that are more comprehensive would help ensure that the situations and needs of important subsets of families are included in analyses designed to inform how health and human service systems can better operate. This administrative data match also misses people who were homeless and did not use homeless services, as well as households that were evicted from housing without going through a formal, court-based eviction process.
Future research using integrated data may want to attend to the sequence of these records (e.g., if Medicaid enrollment precedes eviction or a shelter stay, or a shelter stay preceded eviction). We did not attempt to sequence records during the 3-year study period.
PUBLIC HEALTH IMPLICATIONS
Integrated health, housing, and other human service data is a powerful tool for public health surveillance, practice, and policy research. However, evictions data present challenges to usual approaches to integration. Nevertheless, our findings suggest that integrated evictions, Medicaid, and homeless shelter data can produce a sizeable study group that may be appropriate for some research questions. The children identified in this integrated dataset were enrolled in Medicaid during multiple years, suggesting possible studies of health and healthcare utilization among this group. Black children were also drastically overrepresented, suggesting the need for and utility of studies focused on structural inequity.
Tangibly, the current results affirm that researchers can construct a sizeable study group through linking administrative data sources from Medicaid, shelter utilization and, to a degree, evictions records to interrogate questions about health and healthcare utilization among children with and without these experiences, such as whether forced residential displacement contributes to higher rates of chronic disease or differences in either/both routine and non-routine healthcare. Incorporating additional datasets, especially from universal programs (e.g., education), would likely further improve the match while allowing additional tests of whether and how eviction and homelessness interfere with developmental outcomes.
Dr. Cutuli may be contacted at JJ.Cutuli@Nemours.org
REFERENCES
1. Council on Community Pediatrics. (2013, June). Providing care for children and adolescents facing homelessness and housing insecurity. Pediatrics, 131(6), 1206–1210. https://doi.org/10.1542/peds.2013-0645
2. Cutuli, J. J., & Willard, J. (2019). Building early links for learning: Connections to promote resilience for young children in family homeless shelters. Zero to Three, 39(4), 43–50.
3. Herbers, J. E., & Cutuli, J. J. (in press). Homelessness. In M. H.Bornstein & P. E. Shah (Eds.), Developmental behavioral pediatrions and developmental science.
4. Cutuli, J. J., & Herbers, J. E. (2014). Promoting resilience for children who experience family homelessness: Opportunities to encourage developmental competence. Cityscape (Washington, D.C.), 16(1), 113–140.
5. U.S. Department of Housing and Urban Development. (2020). The 2018 annual homeless assessment report (AHAR) to Congress. https://www.huduser.gov/portal/sites/default/files/pdf/2018-AHAR-Part-2.pdf
6. Metraux, S., Solge, J., Mqangi, O., & Culhane, D. P. (2021). An overview of family homelessness in Delaware: A report to Housing Alliance Delaware. https://static1.squarespace.com/static/59ca9d72268b96cb977e74fd/t/ 61520b359e8d026e5e12c9e9/1632766774483/UDCCRS+Family+Homelessness+in+DE+-+Final+Report+v2.pdf
7. B eharry, M. S., & Christensen, R. (2020, April). Homelessness in pediatric populations: Strategies for prevention, assistance, and advocacy. Pediatric Clinics of North America, 67(2), 357–372. https://doi.org/10.1016/j.pcl.2019.12.007
8. Cutuli, J. J., Herbers, J. E., Lafavor, T. L., Ahumada, S. M., Masten, A. S., & Oberg, C. N. (2014, May). Asthma and adaptive functioning among homeless kindergarten-aged children in emergency housing. Journal of Health Care for the Poor and Underserved, 25(2), 717–730. https://doi.org/10.1353/hpu.2014.0099
9. Grant, R., Gracy, D., Goldsmith, G., Shapiro, A., & Redlener, I.E. (2013, December). Twenty-five years of child and family homelessness: Where are we now? American Journal of Public Health, 103(2, Suppl 2), e1–e10. https://doi.org/10.2105/AJPH.2013.301618
10. Desmond, M., An, W., Winkler, R., & Ferriss, T. (2013). Evicting children. Social Forces, 92(1), 303–327. https://doi.org/10.1093/sf/sot047
28 Delaware Journal of Public Health - June 2023
11. Lundberg, I., & Donnelly, L. (2019, February). A research note on the prevalence of housing eviction among children born in US Cities. Demography, 56(1), 391–404. https://doi.org/10.1007/s13524-018-0735-y
12. Hazekamp, C., Yousuf, S., Day, K., Daly, M. K., & Sheehan, K. (2020, October). Eviction and pediatric health outcomes in Chicago. Journal of Community Health, 45(5), 891–899. https:// doi.org/10.1007/s10900-020-00806-y
13. Desmond, M. (2012). Eviction and the reproduction of urban poverty. American Journal of Sociology, 118(1), 88–133. https://doi.org/10.1086/666082
14. Brumley, B., Fantuzzo, J., Perlman, S., & Zager, M. L. (2015, January 1). The unique relations between early homelessness and educational well-being: An empirical test of the continuum of risk hypothesis. Children and Youth Services Review, 48, 31–37. https://doi.org/10.1016/j.childyouth.2014.11.012
15. Cutuli, J. J., & Herbers, J. E. (2019, September). Housing interventions and the chronic and acute risks of family homelessness: Experimental evidence for education. Child Development, 90(5), 1664–1683. https://doi.org/10.1111/cdev.13041
16. Palmer, A. R., Piescher, K., Berry, D., Dupuis, D., HeinzAmborn, B., & Masten, A. S. (2023, January). Homelessness and child protection involvement: Temporal links and risks to student attendance and school mobility. Child Abuse & Neglect, 135, 105972.
https://doi.org/10.1016/j.chiabu.2022.105972
17. Collinson, R., & Reed, D. (2018). The effects of evictions on low-income households. Unpublished Manuscript.[Google Scholar], 1-82.
18. Schwartz, G. L., Feldman, J. M., Wang, S. S., & Glied, S. A.(2022, February). Eviction, healthcare utilization, and disenrollment among new york city medicaid patients. American Journal of Preventive Medicine, 62(2), 157–164. https://doi.org/10.1016/j.amepre.2021.07.018
19. Richter, F. G.-C., Coulton, C., Urban, A., & Steh, S. (2021). An integrated data system lens into evictions and their effects. Housing Policy Debate, 31(3-5), 762–784. https://doi.org/10.1080/10511482.2021.1879201
20. Cutuli, J. J., Torres Suarez, S., Truchil, A., Yost, T., & Green, C. (under review). Strategies to better identify student homelessness using data in an urban school district.
21. Metraux, S., Mwangi, O., & McGuire, J. (2022, August 31). Prior evictions among people experiencing homelessness in Delaware. Delaware Journal of Public Health, 8(3), 34–38. https://doi.org/10.32481/djph.2022.08.009
22. DMMA. (nd). Medicaid. Retrieved from https://dhss.delaware.gov/dhss/dmma/medicaid.html
23. Centers for Disease Control and Prevention. (n.d.). Link Plus Retrieved from https://www.cdc.gov/cancer/npcr/tools/registryplus/lp.htm
24.Metraux, S., & Guterbock, A. (2020). Eviction and Legal Representation in Delaware-An Overview.V
Delaware Journal of Upcoming Issues
Public Health
Each year, the Delaware Journal of Public Health publishes five different theme issues. Article submissions are accepted on a rolling basis, and the editorial board considers all submissions, both those connected directly to a theme issue, and non-thematic submissions. The editorial board reserves the right to include non-thematic submissions in each issue.
The working publishing calendar and thematic issues for 2023 are as follows:
If you have questions about submissions, ideas for an article, or suggestions for a future theme issue, please email Liz Healy: ehealy@delamed.org
All submissions can be submitted via the online submission portal: https://www.surveymonkey.com/r/2DSQN98
Submissions guidelines can be found at: https://djph.org
29
Issue Submission Publication Oral Health March 2023 April 2023 Homelessness April 2023 May 2023 Neurological Impairment/Stroke July 2023 September 2023 Bio Tech/Research September 2023 October 2023 Health Policy/Ethics November 2023 December 2023
Housing in Delaware for the Intellectual and Developmental Disabilities Population
Jody A. Roberts, Ph.D. Delaware Division of Developmental Disabilities
Ankita Mohan Johns Hopkins Bloomberg School of Public Health
ABSTRACT
Individuals with intellectual and developmental disabilities (IDD) encounter numerous barriers in attempting to access housing. Those barriers – financial, physical, and cultural in nature – have been exacerbated by the COVID-19 public health emergency and the related, or co-occurring, shifts that have characterized the housing market in the United States, and Delaware specifically, over these last three years. In this brief introductory research report, we examine the system of housing supports and their availability to individuals with IDD through a subset of those served by the state’s Division of Developmental Disabilities Services through interviews with representatives across the housing support system. Our findings fall into four areas of work: scale and scope; housing availability; housing assistance; and housing supports. We find that: the estimated scale of the housing crisis (in terms of homelessness and insecurity) affecting this population is much greater than the general population, but in line with other national estimates for individuals with IDD; there is limited available housing that is accessible to individuals with IDD available in the state; there is limited assistance available for navigating the housing that might be available; and that there are too few options for providing more supports for individuals living, or trying to live, independently. We conclude with a few suggested recommendations that could provide more reliable data and tracking of need and a call for research that connects housing for individuals with IDD into the growing body of research looking at the relationship between access to housing and health.
BACKGROUND
Issues related to housing – including availability, costs, and access to adequate supports – have been greatly exacerbated by the COVID-19 pandemic and the associated public health emergency. The Consumer Financial Protection Bureau published a report on Housing insecurity and the COVID-19 pandemic. They found that as of December 2020, 11 million renter and homeowner households were experiencing difficulty keeping up with housing payments. As of March 2021, the 11 million households doubled, emphasizing the impact of the pandemic on housing stability.1 The urgency around housing access and stability has not disappeared since the peak of the pandemic. While the height of the pandemic came with increased funding for housing supports and holds on evictions, as the pandemic relief funds and eviction moratoriums end, more people are being put into a position to experience new or prolonged housing instability. Nationally, housing affordability has steadily decreased since 2019, with rents increasing by 12% and home prices rising an additional 20.6% from March 2021 to March 2022 alone.2 The rapid rise in rent and home prices is being accompanied by a record level of housing shortages, exacerbating the stresses on an already fragile system and drawing continued attention to the importance of increased efforts to support housing stability.2
These broader shifts in housing have exacerbated already existing inconsistencies and inequities in our housing system, especially for those populations consistently at risk for housing insecurity and homelessness. Marginalized groups such as communities of color have been disproportionately impacted by the effects of COVID-19 on the housing market, with Black and Hispanic
households more than twice as likely to be behind on rent or mortgage payments.2
Among those populations impacted by these housing market forces are individuals with disabilities – a population that already faces a complex mixture of lack of accessibility to consistent housing as a result of physical, financial, and cultural barriers. Malcolm Harrison and Cathy Davis write that people with a disability are disproportionately less likely to find suitable housing –housing encompassing adequate costs, accommodations, and nearby resources.3 For an individual with a disability, then, seeking out accessible home options in an already strained housing market means confronting both financial and physical barriers simultaneously. Aging housing stock and rental units that are historically inaccessible combine with new housing that has not been designed for accessibility and may be disconnected from reliable community amenities and services. Therefore, often the housing environment itself can hinder factors such as selfmanagement and can aggravate an individual’s condition.3
Most individuals with disabilities, and especially those with intellectual and developmental disabilities, are supported by Medicaid for access to their service supports, which effectively locks many of these individuals into situations of financial poverty, foreclosing on access to available housing options. For instance, 70% of Native Hawaiian, 67% of Hispanic, 63% of people who are under 18, and 59% of people living in a metro area who are enrolled in Medicaid are living in inadequate or unaffordable homes.4
Further, individuals with disabilities, especially those with intellectual and developmental disabilities (IDD), face the
30 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.007
additional barrier of significant and persistent bias in society, which can manifest itself in an unwillingness by some to rent or sell to an individual with IDD, by preventing access to all amenities at a housing or apartment complex beyond the specifically designated “accessible” housing unit, or by creating hostile environments within the communities where these individuals live.
While according to The Americans with Disabilities Act, it is illegal to refuse to rent a property to an individual solely based on their disability status, landlords can refuse to rent based on credit history, income level, and prior evictions, all of which put people in the disability community at a disadvantage.5
While the features of this broader problem are well known anecdotally, it is not well understood in terms of its scope or scale, or in the specific ways in which it operates, which inhibits effective policy to be developed to address these ongoing and persistent barriers.
The research outlined in this paper looks at the ways in which the current housing crisis is manifesting itself within the IDD community in Delaware in an effort to ground our discussions in more empirical observations. It is also a way to begin disentangling – or, at least, highlighting the entanglements – of the ways in which our terminology, e.g., housing, can obscure the more complicated features of housing, housing security, and housing supports that are all in play, but in different ways. The informational interviews conducted for this work provide some sense of the system that will need to be contended with as we move forward. Our hope is to find a way past anecdote to inform and support data-informed approaches to housing that also stay grounded in a commitment to equity in the face of complexity.
HOUSING AND INTELLECTUAL & DEVELOPMENTAL DISABILITIES
For the disability community, accessibility is both a common and complex refrain. As we know from housing and health research more generally, housing has a direct impact on health outcomes.6 The situation is no different for those with disabilities. The ways that a property accommodates an individual with a disability impacts their health outcomes. Research dating back to the time of the passing of the Americas with Disabilities Act (ADA) have demonstrated how housing adaptations have positive effects on the ability of people with disabilities to live independently.7 For example, modifications such as walk-in showers, handrails, and lowered kitchen counters can enhance daily activities and mobility for people with IDD. Additionally, the significance of modifications that foster social inclusion, such as creating shared meal spaces or communal areas for socializing is large. By increasing accessibility and inclusivity, housing adaptations can improve the quality of life and independence for people with IDD, allowing them to more fully participate in their communities.7 More recent research has expanded the notion of the home to include the importance of the “home environment,” or the social and physical contexts that shape the quality of life in the home, and its role in well-being for individuals with disabilities.8
We also know that individuals with disabilities aren’t only disabled, but are often over-representative of other historically marginalized groups, especially when it comes to housing.
The application of an intersectional lens both highlights, and complicates, the challenges that individuals with intellectual and developmental disabilities face when it comes to securing stable housing, avoiding or emerging from homelessness, or accessing housing in an environment that can provide access to overall health and well-being. That is, when considering housing and health outcomes we need to be mindful not only of disabilities, but also of, for example, the individual’s race, gender, and income, as important factors shaping both experience and what may be “accessible” for an individual.9 For instance: according to the Centers for Disease Control and Prevention (CDC), people who are Black are more likely to have a disability, with a rate of 25% compared to the 20% disability rate for Non-Hispanic Whites.10 We also know that individuals who are Black make up 39% of people experiencing homelessness and more than 50% of homeless families with children.11 In asking questions, then, of access to housing for a Black individual who also has disabilities, we cannot chose between data sets, but instead, must grapple with the intersection and overlap of these factors.
Focusing specifically on intellectual and developmental disabilities, the association between IDD and poverty has been established in the literature and more recent research has found that IDD is both a risk factor for homelessness and an additional barrier for those experiencing homelessness.12
In Delaware, a few state entities directly handle the housing assistance process, specific to the disability community. There are five housing authorities in the state of Delaware: the Delaware State Housing Authority, the Wilmington Housing Authority, the New Castle County Housing Authority, the Dover Housing Authority, and the Newark Housing Authority. The housing authorities exist, as the Delaware State Housing Authority states, “to efficiently provide, and assist others to provide, quality, affordable housing opportunities and appropriate supportive services to low- and moderate-income Delawareans.”13 This responsibility includes the management of state and federal assistance programs to homeowners and renters. For rental assistance programs, federal programs such as 811 Rental Assistance and Mainstream Vouchers are applied for by the housing authorities and distributed to those needing housing supports. The State Rental Assistance Program (SRAP) and other state-run assistance programs are allocated based on state funds. The housing authorities’ main responsibilities are to provide financial backing, management, and organization.
Ultimately, the system mainly relies on voucher programs to support the housing needs of individuals in the state. For the distribution of vouchers and rental assistance for the developmental disabilities community, individuals within the Delaware Department of Health and Social Services’ Division of Developmental Disabilities Services (DDDS) manage the distribution of the available vouchers to the individuals being served by the division. Community Navigators, who provide targeted case management to many of the individuals served by DDDS, directly communicate with, assist, and work with individuals served by the division and their families. In relation to housing, these individuals are responsible for adding individuals to housing waitlists, locating available and affordable housing, finding solutions for those experiencing housing instability or homelessness, and communicating this information with individuals at DDDS. Individuals who are able to obtain a
31
voucher, sometimes working with their case manager, are then tasked with finding units that fit their needs and have availability. Details related to obtaining housing with a voucher are outlined in the findings.
METHODOLOGY
This study aims to establish a better understanding of the housing landscape in Delaware and the systems that exist in the state to assist individuals with IDD in navigating the housing system. We conducted a small set of exploratory, semi-structured interviews with individuals involved in three areas of the housing ecosystem:
1. A representative from the Delaware State Housing Authority;
2. A representative of Housing Alliance Delaware;
3. A supervisor in case management within the Division of Developmental Disabilities Services; and
4. Six county-wide case management supervisors overseeing targeted case management to individuals with intellectual and developmental disabilities that include assistance in identifying community housing resources.
These eight interviews provided additional insights and an understanding of how access to housing resources for individuals with intellectual and developmental disabilities works from policy to practice. Based on this information, we outline some sense of how the housing system of supports works for those with intellectual and developmental disabilities.
FINDINGS AND DISCUSSION
Findings from the interviews have been placed into four categories: scope and scale, housing availability, housing assistance, and housing supports (table 1).
Table 1: Summary of Findings: Scope and Scale of Housing Insecurity Impacting Individuals with IDD in Delaware
Scope Housing Availability Housing Assistance Housing Supports
the context of the interviews was taken to mean an individual is currently housed, but the stability of this housing is now, or may be in the future, at risk due to financial, safety, or personal concerns. These numbers reflect homeless and housing insecurity experienced by individuals currently receiving services from the Division and do not reflect the total, estimated number of individuals with IDD in the state. While these numbers appear extraordinary, they are in line with data available nationally for individuals with IDD.
1. The Scope: Based on conversations with the six Community Navigator Supervisors, an estimate of those experiencing homelessness and housing instability was established. On average, at any given point, between 2-5% of service recipients are experiencing homelessness and between 8 and 15% are experiencing housing instability. If validated, these rates would far exceed measures for homeless and housing insecurity generally, but would match those of other at-risk populations, such as those individuals who are on the Sex Offender Registry in Delaware.14
2. Housing Availability: A main takeaway from the interviews was the limited infrastructure that exists to accommodate the housing needs of all people living with a developmental disability in Delaware. Further, the resources that are available are concentrated in more populated counties such as New Castle County and Kent County. This leaves those living in Sussex County without many resources and forces them to relocate, often away from family, to where there is availability. In addition to the scarcity of housing, the location of available housing is also a concern. Community Navigator Supervisors consistently pointed to the environmental components of the available housing as reasons why service recipients turn down housing. Issues such as crime, violence, drug abuse, and physical and emotional abuse were cited as reasons service recipients chose to turn down available housing in specific areas.
Homelessness:
1.6%-5% Resource Allocation Closed Waitlists Supports in Independent Living Preparedness
Housing Instability: 8% Environmental Factors Years Long Waitlists
Limited Housing Infrastructure and Development
Transitional Housing with Supports
Lack of Housing Options Support Built into New Developments
All of the county-wide case supervisors were asked to provide estimates of homelessness and housing insecurity experienced on a routine basis for all clients they serve. While there was variation based on location/county and specific subsets of individuals being served, all reported numbers within a range of 1.6%-5% experiencing homelessness and between 8 and 15% experiencing housing insecurity at any given time. Housing insecurity in
3. Housing Assistance: Apart from the lack of housing infrastructure, we found that the housing assistance programs in Delaware are not efficient. As of March 2022, the DE State Housing Authority closed its rental assistance waitlist. For those already on a waitlist, it takes years to be given a voucher. Further, for those who do have a voucher, the lack of infrastructure from the previous finding impacts the individual’s success. With a lack of rental units available, even those with vouchers struggle to find stable housing, often having a voucher expire before housing is found.
4. Housing Supports: This category of findings encompasses support for individuals through the entire process of finding housing. Based on the interviews with participants, it was found that for individuals who may even be able to afford housing independently, there is a lack of training, information given, and support to help them transition to independent living. Beyond this initial support, for those who are temporarily or chronically experiencing homelessness or housing instability, it was identified that specific transitional housing that would provide temporary housing along with residential support for those who needed it, was lacking. Finally, participants identified the need for residential support within new housing infrastructure that was developed in order to best accommodate those with intellectual and developmental disabilities.
32 Delaware Journal of Public Health - June 2023
RECOMMENDATIONS
While the research here is quite preliminary, it does suggest some immediate options for action that include opportunities to begin making corrections while we learn more about the scale, scope, and impact of housing insecurity and homelessness on the IDD service population in Delaware. Here, we offer three areas to pursue while this conversation grows.
BETTER DATA TRACKING WITHIN DDDS
Homelessness and housing insecurity with the population served by DDDS is persistent and ongoing. Efforts, not surprisingly, are focused on the pressing and immediate need of the individual or family being served. And while some data is tracked internal to both the division and the divison’s targeted case management entity, the Columbus Organization, an effort to systematize this data could create an opportunity for better tracking. Tracking could elucidate more about the need, but also about what works (or doesn’t) and help to bring effort and investment in best practices or identification of gaps in the system.
INCOMPLETE PICTURES
Tracking data on housing insecurity and homelessness provides an incomplete picture at best. We also need a better, consistent, and reliable source of information on housing needs more broadly. This broader housing needs survey would provide a more complete picture of housing – actual built infrastructure –needed to allow a growing population of those with intellectual and developmental disabilities, as well as those with other physical disabilities, acquired disabilities, or those seeking to age in place as their physical abilities change, to live in homes and communities across the state. Such an effort presents us with the opportunity to be both comprehensive and proactive, identifying key demographic shifts already underway and expected that will shape the future of needs for community life in Delaware. More importantly, this housing need must be situated within, not exist separate from, our larger efforts to study, anticipate, and invest in meeting our state’s housing needs. Simply tracking needs related to housing insecurity and homelessness for this with intellectual and developmental disabilities without this companion effort would be akin to creating a hospital with only an emergency department – and then building a separate emergency department for those with IDD.
MORE RESEARCH NEEDED
We also need more research on the connections between housing and health outcomes for those with intellectual and developmental disabilities. Despite a growing body of research within this area, there is scant attention to including individuals with IDD in this effort that seeks to see housing as a core component of the social determinants of health. There is a critical need to address the historical exclusion and invisibility of individuals with IDD from these larger research efforts. Doing so would reaffirm that the intellectual and developmental disabilities an individual may have are not/not the only challenges one may face in the pursuit of good health. It may shed light on options and opportunities to overcome systemic barriers to a healthy life. And, critically, it ensures that we see individuals with IDD with the same gaze as others – challenged by a lack of access to a consistent home or home life, but also able to thrive when given access to the same supportive home environment that we already know supports the health outcomes of others.
Dr. Roberts may be contacted at jody.roberts@delaware.gov
REFERENCES
1. Consumer Financial Protection Bureau. (n.d.). Housing insecurity and the COVID-19 pandemic. Retrieved from: https://www.consumerfinance.gov/data-research/research-reports/ housing-insecurity-and-the-covid-19-pandemic/
2. Cost of Home. (n.d.). 2022 State of the nation’s Housing Report: 4 key takeaways for 2022. Retrieved from: https://www.habitat.org/costofhome/2022-state-nations-housing-reportlack-affordable-housing
3. Harrison, M., & Davis, C. (2001). Disability and housing. Housing, Social policy and difference: disability, ethnicity, gender and housing, 1st ed., Bristol University Press, pp. 113–40.
4. Corallo, B. (2021, Sep). Housing affordability, adequacy, and access to the internet in homes of medicaid enrollees. Kaiser Family Foundation. Retrieved from:
https://www.kff.org/medicaid/issue-brief/housing-affordabilityadequacy-and-access-to-the-internet-in-homes-of-medicaid-enrollees/
5. Stewart, M. (2021, Jun). Legal and illegal reasons landlords may turn rental applicants down. Nolo. Retrieved from https://www.nolo.com/legal-encyclopedia/free-books/renters-rightsbook/chapter1-2.html
6. Krieger, J., & Higgins, D. L. (2002, May). Housing and health: Time again for public health action. American Journal of Public Health, 92(5), 758–768.
https://doi.org/10.2105/AJPH.92.5.758
7. Dunn, P. A. (1990). The impact of the housing environment upon the ability of disabled people to live independently. Disability, Handicap & Society, 5(1), 37–52.
https://doi.org/10.1080/02674649066780031
8. Cho, H. Y., MacLachlan, M., Clarke, M., & Mannan, H. (2016, August 17). Accessible home environments for people with functional limitations: A systematic review. International Journal of Environmental Research and Public Health, 13(8), 826 https://doi.org/10.3390/ijerph13080826
9. Columbia Law School. (2017, Jun). Kimberlé Crenshaw on intersectionality, more than two decades later. Columbia Law School, https://www.law.columbia.edu/news/archive/ kimberle-crenshaw-intersectionality-more-two-decades-later
10. Centers for Disease Control and Prevention. (2020, Sep). Infographic: adults with disabilities: ethnicity and race.” Centers for Disease Control and Prevention.
https://www.cdc.gov/ncbddd/disabilityandhealth/materials/infographicdisabilities-ethnicity-race.html
11. National Alliance to End Homelessness. (2021, Apr). Homelessness and racial disparities.
https://endhomelessness.org/homelessness-in-america/what-causeshomelessness/inequality/
12. Mercier, C., & Picard, S. (2011, April). Intellectual disability and homelessness. J Intellect Disabil Res, 55(4), 441–449. https://doi.org/10.1111/j.1365-2788.2010.01366.x
13. Delaware State Housing Authority. (n.d.). State of DelawareSearch and Services/Information. ABOUT DSHA.
http://www.destatehousing.com/DirectorsOffice/aboutAgency.php
14 University of Delaware. (n.d.). Joseph R. Biden, Jr. School of Public Policy & Administration.
https://www.bidenschool.udel.edu/
33
Homelessness Among Persons on Delaware’s Sex Offender Registry
Stephen Metraux, Ph.D. and Alexander C. Modeas, M.A. Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
ABSTRACT
This study provides an in-depth analysis of homelessness among people on the Delaware Sex Offender Registry (SOR) between 2021 and 2023. Delaware’s SOR, as a publicly accessible database, offers a uniquely comprehensive window into an unsheltered population among a group that is, collectively, at high risk of experiencing homelessness. We retrieved data from the Delaware SOR on two separate dates, which allowed us to track homelessness among offenders within the state over time. On November 15, 2021, 4.6 percent of the persons on the SOR were homeless. Fifteen months later, this homeless prevalence rate was 5.5 percent. Of the 120 people who reported homelessness on the November date, 56 of them (46.7 percent) were either still homeless or again homeless fifteen months later. This prevalence is significantly higher than rates among the general population, and, once homeless, a substantial proportion remained homeless for extended periods of time. The high rate of unsheltered homelessness among people on the Delaware SOR emphasizes the shortcomings in Delaware’s ability to supply shelter for homeless individuals, as well as the additional restrictions people on the SOR experience in their ability to receive these services, which creates hardship for these individuals and reduces communal public safety by increasing the frequency of absconding.
INTRODUCTION
The homeless population is notoriously challenging to count and characterize, as they are difficult to identify and locate, and often wish to keep the circumstances of their lack of housing private. Estimates of homeless population size such as the annual, nationwide point-in-time count are widely used to gauge the year-to-year dynamics of the homeless population despite acknowledgment that they leave many persons experiencing homelessness uncounted. More generally, efforts to collect data that is representative of homeless populations, or can accurately assess the prevalence and correlates of homelessness in more general populations, have been challenged by the vexing set of circumstances endemic to this formidable problem. This study presents exploratory results from a widely available dataset that offers exceptions to some of the major obstacles to getting accurate assessments of homelessness that were just mentioned and focuses on a group that is among those who are at the highest risk of becoming homeless. Delaware, like all states, maintains a publicly accessible sex offender registry (SOR) containing information on the whereabouts of people convicted of sex crimes. One of the features of Delaware’s SOR is that it identifies who among those on the registry are currently experiencing homelessness.1 All persons on Delaware’s SOR must promptly report their homelessness to the Delaware State Police under the threat of criminal penalty if they fail to do so. As such, Delaware’s SOR provides useful information for understanding the dynamics of homelessness, as people whose homelessness would otherwise be unrecognized instead report and regularly update their housing circumstances and face legal sanction if they fail to do so.
Having a conviction for a sex offense substantially increases a person’s risk of becoming and staying homeless.2,3 The stigma that such a conviction carries leads to difficulty in securing employment and housing.4,5 Among other things, this has led many localities to proscribe people convicted of sex offenses from living in “buffer zones” around places that feature concentrations of children, such as schools and parks, further circumscribing their housing options despite the lack of evidence that such restrictions are effective.6,7 The dynamics of racial segregation magnify the impact of residency restrictions for African Americans who are on the SOR, such that they are at particularly high risk for experiencing homelessness.8 Once homeless, people on the SOR face additional constraints that lead to increased difficulty in exiting homelessness as, either by law, by policy, or by practice, many homeless services and much of the already scarce affordable, subsidized, and supportive housing are off limits to them.9
There continues to be substantial political support for maintaining SORs as a tool to manage the presence in the community of people convicted of sex offences, despite the lack of research that links SORs with any significant public safety benefits.10 This surveillance is both predicated upon stringent reporting requirements and on making information that is typically kept confidential for other populations, on such topics as personal identity and housing status, publicly available. In Delaware, for example, homelessness (as well as residential address for those who have housing) is specifically indicated on individually identified SOR records. Furthermore, experiencing homelessness increases the burden of verification requirements so that homeless Tier II (moderate risk level) offenders must report, in-person, to a designated state police office every 30 days (compared to every 90 days when housed), and homeless Tier III (high risk level) offenders must report every seven days (instead of every 30 days).11 This renders information on homelessness
34 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.008
among people on the SOR to be more available, comprehensive, and current than any other data in Delaware containing individual records and information on homelessness.
Finally, three other studies look at homelessness using SOR data. Harris et al.’s overview of SORs from 42 states and 2 US territories (Delaware declined to participate) found that 30 states and one territory tracked homelessness among those on their registries, with a combined overall rate of homelessness (for all on the registries) at 3.0 percent, and with individual state rates as high as 5.7 percent in California and 4.8 percent in Maine. Byrne et al. matched individual SOR records from 19 states with records from the US Department of Veterans Affairs and found that among a veteran population seeking VA health care, being on the SOR was associated with an 80 percent higher risk of experiencing homelessness.3 Two studies drawing from Florida SOR records, found that 3.2 percent of registered persons who were in Florida communities reported homelessness, with a disproportionate presence in counties with a larger number of local-level residence and/or other restrictions, higher population density, and expensive housing costs2; and with individual characteristics including age, minority status, victim type (minor vs. adult), risk level, supervision status, and prior failure to register convictions also associated with increased homelessness risk.12
DATA AND METHODS
The data source for this study was the Delaware Sex Offender Central Registry (i.e., Delaware’s SOR), a publicly accessible, searchable website maintained by the Delaware State Police that contains information, including name and residence information, for people whose conviction mandates them to be included on Delaware’s SOR. The online registry allows for querying records based upon the dichotomous indicator of whether or not the person reports currently experiencing homelessness. The statutes regarding the sex offender registry in the Delaware code are not specific in defining homelessness beyond situations in which “the offender is unable to secure an anticipated place of future residence.” Looking at specific locations mentioned as residences by those denoted as homeless on the registry, this means living in outdoor locations, in shelters and other temporary housing provided by social service organizations, and staying in hotels or motels.
Individual records with homeless indicators on Delaware’s SOR were identified and manually copied to an Excel database. The data collection was initially limited to all those who were on the SOR on November 15, 2021, and a follow-up sample was collected on February 16, 2023. Automated processes for “scraping” data were not available for this study, so data on the overall population in Delaware’s SOR were limited to what was available by manipulating the registry’s search engine. In both homeless and overall cases, for each of the two data collections we limited the study group to the records of those who were not incarcerated and had an in-state residence on the day of collection. The analyses are limited to reports of prevalence and descriptive statistics that aggregate the data collected from the registry.
The University of Delaware Institutional Review Board determined that this study was exempt from review. Although all the data used for this study were publicly available at the time they were collected, it is not possible now to collect data on people on the registry at previous points in time. Given this, we report our findings in a manner that would preclude the identification of individual records based upon the results that we report and as though the data were not publicly available.
RESULTS Prevalence of Homelessness
Table 1 reports the total numbers of persons living in Delaware communities (i.e., not out of state or incarcerated), and those in these populations reporting homelessness, at two discrete points in time: November 15, 2021 and February 16, 2023. On the former date, 120 of 2,613 people (16.7 percent) on the SOR reported homelessness. Fifteen months later, 140 people reported homelessness (a 16.7 percent increase), among 2,531 people (a 3.1 percent decrease) on the SOR.
Table 1. Persons on Delaware’s SOR Who Reported Homelessness at Two Points in Time
Adjusted for population differences, this amounts to a 20.4 percent increase in homelessness among people on the SOR on the 2023 date. This indicates that the increase in homelessness across the two dates that are shown on Table 1 is not just a function of 20 more people becoming homeless on the 2023 date, it also reflects a higher rate of homelessness (5.5 percent compared to 4.6 percent) on that date as well.
Fifty-six people were identified as being among those reporting homelessness on both of the days on which the data collection occurred. This means that 46.7 percent of the 120 who were homeless on the 2021 date either remained or again became homeless on the 2023 date. Conversely, 40 percent of those identified as homeless on the 2023 date were also among those who reported homelessness on the 2021 date. Others may have been homeless on both dates, but were not on the SOR on both dates.
Geography of SOR homelessness
Homelessness among people on the SOR is a geographically concentrated phenomenon, regardless of whether it is measured by county, city, or zip code. Table 2 displays these distributions. On the county level, half of those who were on the SOR and reported homelessness reported from New Castle County. This rate is not disproportionately high when considering that New Castle County contains 56.9 percent of the overall state population. However, 7.1 percent of all New Castle County residents on the SOR reported homelessness, a rate substantially higher than the corresponding rates for Kent (5.1% and Sussex 4.0%) counties.
Concentrations of homelessness among those on the SOR are even more apparent when looking at distributions by city and by zip code. Six cities contain 59% of those on the SOR who report homelessness, and Wilmington and Dover
35
Nov. 15, 2021 Feb. 16, 2023 % Change Total Homeless 120 140 16.7 Total on SOR 2,613 2,531 -3.1 Percent Homeless 4.6 5.5 20.4 Total on SOR & Homeless on Both Dates 56 56 n/a Repeat Homeless as a % of Total Homeless 46.7 40.0 n/a
alone, Delaware’s two largest cities, account for half of those reporting homelessness. There is a similar pattern when looking at the distribution by zip code in 2023, where most of Wilmington’s homeless persons (33 of 42) are from two zip codes (19801 and 19805) and all of Dover’s homeless (29) also are from two zip codes (19901 and 19904). With the exception of New Castle, these cities and zip codes all have rates of homelessness well above the statewide 5.5 percent rate, with the highest homelessness rate occurring in 19801, at 11.5 percent.
People on the SOR, regardless of housing status, are required to provide a specific street-level address for where they reside. Less than ten of these addresses clearly indicate shelters, and none of these records indicate any stay at the largest men’s overnight shelter, which is located in Wilmington (19801). Less than ten records refer to other homeless service locations that don’t provide overnight accommodations (these may serve as a mailing address), and less than ten contained references to various motels. Much more common were “street addresses” that indicated sleeping in outdoor locations: references to convenience stores, “big box” stores, and other commercial establishments that did not provide
housing; intersections and street addresses in non-residential locations; and specific references to tents, woods, and encampments. Beyond such impressions, it is difficult to categorize these locations more specifically.
Individual Characteristics and Circumstances
There are a limited number of individual characteristics and circumstances pertaining to demographics, employment status, and legal history that were available on the SOR.
Table 3 provides summary measures of key indicators on these topics. Data on these topics were collected only for the group that reported homelessness on November 15, 2021. We expect the distributions in Table 3 would not be substantially different for those who were homeless in early 2023.
Demographics. The median age for the 120 people reporting homelessness on Delaware’s SOR was 42, with 31.6 percent of the group over age 50. Everyone in the group was listed in the SOR as either White or Black, notwithstanding that the “race” indicator also reported a few (i.e., less than ten people) also had “Hispanic” or “Asian” in parentheses. The majority in the group (59.2 percent) were Black. Finally, the homeless subpopulation was almost exclusively male, with a small number (less than ten) of women reporting homelessness.
* “Rate of homelessness” refers to the percent of those on the SOR reporting from a particular geographic area who report experiencing homelessness. Data is not available to calculate this for the 2021 study group.
** Exact numbers are suppressed to maintain individual record anonymity as cell values are less than 10.
36 Delaware Journal of Public Health - June 2023
November 15, 2021 February 16, 2023 N % total N % total rate of homelessness* County Kent 36 30.0 39 27.9 5.1 New Castle 61 50.8 70 50.0 7.1 Sussex 23 19.2 31 22.1 4.0 City Wilmington 34 28.3 42 30.0 7.7 Dover 26 21.7 29 20.7 7.6 New Castle 10 8.3 11 7.9 4.4 Newark ** ** 13 9.3 6.1 Georgetown ** ** 10 7.1 7.5 Remainder in other cities 36 30.0 35 25.0 3.5 Zip 19901 (Dover) 19 15.8 15 10.7 6.5 19801 (Wilmington) 17 14.2 20 14.3 11.5 19805 (Wilmington) 11 9.2 13 9.3 7.7 19720 (New Castle) 10 8.3 11 7.9 4.4 19904 (Dover) ** ** 14 10.0 7.0 19947 (Georgetown) ** ** 10 7.1 7.4 All other ZIPS 49 40.8 57 41.0 4.2 Total 120 140 5.5
Table 2. Geographical Distribution of People on Delaware’s Sex Offender Registry Reporting Homelessness
Table
DISCUSSION
The main finding of this exploratory study underscores how pervasive and persistent homelessness is among people on Delaware’s SOR. Specifically, on November 15, 2021, 4.6 percent of the persons on the SOR were homeless. Fifteen months later, this homeless prevalence rate was 5.5 percent. Furthermore, of the 120 people who reported homelessness on the November date, 56 of them (46.7 percent) were either still homeless or again homeless fifteen months later. These prevalence rates are orders of magnitude higher than rates among the general population, and, once homeless, a considerable proportion remained so for extended periods of time.
While these numbers are stark, they are not surprising given the volume of research linking sex offense convictions with elevated homelessness risk. More novel are the findings showing how, among sex offenders, homelessness is concentrated (in the 2023 count) to five cities that collectively contain 75 percent of those on the SOR reporting homelessness and, more specifically, to six zip codes that collectively contain 59 percent of this subgroup. The SOR further indicates how, for people on the SOR, homelessness is most commonly experienced in unsheltered settings. This highlights both the shortfall in shelter bed supply for homeless individuals and the additional restrictions people on the SOR face in accessing these beds. Ironically, while the latter group has a harder time getting a shelter bed, they are much more likely to have their homelessness recorded, via the SOR, than the rest of the unsheltered population. This is due both to their reporting requirements and the haphazard nature of enumerating the more general unsheltered homeless population in Delaware. This leads to a perverse situation where roughly 130 people on the SOR appear to have been unsheltered on a night in February 2023, while only 154 people were counted as unsheltered in the statewide Point in Time (PIT) count that was conducted in February 2022.13 This juxtaposition shows how the PIT count, which is the most comprehensive enumeration of the homeless population in Delaware, drastically undercounts the unsheltered homeless population and how as a result most of Delaware’s unsheltered population is invisible to service providers and policymakers.
Employment. The SOR reports, for those on the registry who are employed, specific work locations. Forty percent of those reporting homelessness gave employment information, indicating they had some employment, which presumably includes fulltime, part-time, and temporary jobs. One logistical issue related to employment is automobile ownership, with 28% (of all 120 people) reporting they had a vehicle.
Sex Offender Registry Dynamics. An overwhelming proportion (88.3 percent) of those on Delaware’s SOR reporting homelessness were not repeat offenders. Just under three-quarters (70.8 percent) had their risk assessment level as tier 2 (moderate risk), with the rest at tier 3 (high risk). People at tier 1 (low risk) are not included on Delaware’s publicly accessible SOR. Just under two-thirds (65.0 percent) have been listed on the SOR for over a decade. The median time listed on the SOR is 12 years. Finally, 17.5 percent are listed as “wanted,” meaning that they have violated the terms of their release or have not met SOR reporting requirements.
The reason why Delaware’s SOR can provide a much more comprehensive count of homelessness than the PIT count can provide for the more general homeless population is that the SOR is a surveillance program with legally mandated participation. Its frequently updated, comprehensive roster of names and locations of homeless persons also amounts to a “by name list” that social and health care workers can use to coordinate efforts to target the housing and services needs of this population.13The use of by-name lists is a best practice approach14 that has contributed to the elimination of homelessness among veterans in Delaware15 and in other localities across the US.16 The data available on the SOR similarly lies ready to use as the basis for eliminating homelessness among those who have sex offense convictions. Seen more broadly, the SOR can also function as a surveillance system in the public health sense, in which data is collected to prevent and ameliorate diseases and other health-related problems. Seen from this perspective, there are clear ethical questions, mentioned earlier in this study, about the public dissemination and the lack of confidentiality around this
37
N % total Demographics Age 18-29 10 8.3 30-39 31 25.8 40-49 41 34.2 50-65 34 28.3 65+ 4 3.3 Median age 43 years Race Black 71 59.2 White 49 40.8 Employment & Car Ownership Employed 48 40.0 Own a Car 34 28.3 Legal Dynamics Repeat offender Yes 14 11.7 No 106 88.3 Risk Assessment Level Tier 2 85 70.8 Tier 3 35 29.2 Years on Registry less than 1 year 4 3.3 1-2 years 7 5.8 3-5 years 10 8.3 5-10 years 21 17.5 10+ years 78 65.0 median length of time 12 years Listed as “Wanted” 21 17.5
3. Demographics, Employment Status, and Legal History for Persons on the SOR Reporting Homelessness on November 16, 2021
surveillance data. Those notwithstanding, there are also further ethical considerations inherent to there being a surveillance system that provides specific parameters for intervening in a public health emergency that makes this homelessness publicly visible but summarily ignored. In effect, this situation goes against the adage that “one must count something for it to count,” as in the current situation homelessness among people on the SOR still does not seem to count.17
This also has implications from a criminal justice perspective. Our findings show high rates of people on the SOR who reported homelessness as having absconded (17.5 percent), meaning they have stopped reporting to the authorities charged with their supervision. This raises a collateral concern about whether their lack of stable housing creates a threat to public safety. This higher rate of absconding is not surprising, as homeless both triggers more frequent reporting requirements and creates more logistical difficulties in fulfilling reporting requirements. This creates concerns, however, about how the lack of adequate housing creates a potential public safety threat. Delaware’s SOR highlights this problem (and might even contribute to it through its reporting requirements), but even this appears to do little to spur action to address housing needs among this population.
As mentioned earlier, this is an exploratory study with data that is publicly available. The results reported here indicate an acute housing problem among a population that is at once deeply stigmatized and unusually well-defined. The findings reported here represent a beginning, as they raise numerous further questions that demand additional research. But, more immediately, they also represent a call to action that has to date gone largely unheeded, both to address homelessness in a specific context under extremely challenging circumstances, as well to address the urgent need for more accurate surveillance data (in the public health sense, and in accordance with ethics guidelines) as a first step to better defining the true scope of homelessness and to implementing solutions commensurate to the actual size of the problem.
Dr. Metraux may be contacted at metraux@udel.edu.
REFERENCES
1. Delaware State Police. (n.d.). Delaware Sex Offender Registry. State Bureau of Identification. Retrieved from: https://sexoffender.dsp.delaware.gov/
2. Socia, K. M., Levenson, J. S., Ackerman, A. R., & Harris, A. J. (2015, December). ‘Brothers under the bridge’: Factors influencing the transience of registered sex offenders in Florida. Sexl Abuse, 27(6), 559–586. https://doi.org/10.1177/1079063214521472
3. Byrne, T., Cashy, J., Metraux, S., Blosnich, J. R., Cusack, M., Culhane, D. P., Montgomery, A. E. (2022, April). Association between registered sex offender status and risk of housing instability and homelessness among veterans. Journal of Interpersonal Violence, 37(7-8), NP5818–NP5829.
https://doi.org/10.1177/0886260520959646
4 Grossi, L. M. (2017). Sexual offenders, violent offenders, and community reentry: Challenges and treatment considerations. Aggression and Violent Behavior, 34, 59–67
https://doi.org/10.1016/j.avb.2017.04.005
5 Tewksbury, R. (2012). Stigmatization of sex offenders. Deviant Behavior, 33, 606–623.
https://doi.org/10.1080/01639625.2011.636690
6. Parra, E. (2015, Apr). Delaware debate: Should towns ban sex offenders? Delaware News-Journal. Retrieved from: https://www.delawareonline.com/story/news/local/2015/04/10/ delaware-debate-towns-ban-sex-offenders/25593553/
7. Levenson, J. S. (2008). Collateral consequences of sex offender residence restrictions. Criminal Justice Studies, 21(2), 153–166
https://doi.org/10.1080/14786010802159822
8 Suiter, E., & Andersen, T. S. (2022). Residency restrictions, race, and homelessness among registered sex offenders. Criminal Justice Studies, 35(2), 132–144.
https://doi.org/10.1080/1478601X.2022.2026352
9 Rolfe, S. M., Tewksbury, R., & Schroeder, R. D. (2017, December). Homeless shelters’ policies on sex offenders: Is this another collateral consequence? International Journal of Offender Therapy and Comparative Criminology, 61(16), 1833–1849
https://doi.org/10.1177/0306624X16638463
10. Levenson, J. S., Ackerman, A. R., Socia, K. M., & Harris, A. J. (2015). Where for art thou? Transient sex offenders and residence restrictions. Criminal Justice Policy Review, 26(4), 319–344
https://doi.org/10.1177/0887403413512326
11. State of Delaware. (n.d.). Delaware Code. Title 11, Chapter 41, §4121(k). Retrieved from:
https://delcode.delaware.gov/title11/c041/sc03/index.html
12 Housing Alliance Delaware. (2023). Point in time count & housing inventory count: 2022 report. Retrieved from https://www.housingalliancede.org/_files/ugd/9b0471_ b4f4bc93e75c4923a891bc0d33fb4dbd.pdf
13. Supportive Services for Veteran Families Program. (2016). Overview: the master list. U.S. Department of Veterans Affairs. Retrieved from:
https://www.va.gov/homeless/ssvf/docs/master_list_overview_ march2016.pdf
14 Solutions, C. (2021). What is a By Name List? Retrieved from:
https://login.builtforzero.org/what-is-a-by-name-list/
15 Delaware State Housing Authority. (2017). Achieving an End to Veteran Homelessness in Delaware: A Report from the State Working Group. Author. Accessed April 6, 2023 at: http://destatehousing.com/vets/media/vet_report.pdf
16 U.S. Interagency Council on Homelessness. (2017). 10 Strategies to End Veteran Homelessness. Author. Accessed April 6, 2023 at: https://www.usich.gov/resources/uploads/asset_library/TenStrategies-to-End-Veteran-Homelessness-v3.pdf
17 Fairchild, A. L., Haghdoost, A. A., Bayer, R., Selgelid, M. J., Dawson, A., Saxena, A., & Reis, A. (2017, August). Ethics of public health surveillance: New guidelines. The Lancet. Public Health, 2(8), e348–e349 https://doi.org/10.1016/S2468-2667(17)30136-6
38 Delaware Journal of Public Health - June 2023
Financial Aid
2023 Workforce Initiative
Application open until funds are depleted
Eligibility:
• U.S. Citizen or permanent resident (I-151 or I-551 card)
• One year of residency in the State of Delaware
• Enrolled in an approved degree-granting program or certificate in Nursing, Medical Assistant, Dental Assistant, Physician Assistant, Behavioral Health or Allied Health

Requirements:
• Completed online application
• Online self-certification form
• Copy of most recent signed Delaware tax return (personal and/or parents, if dependent)
• Proof of Delaware residency (driver’s license, vehicle registration, voter’s registration card)

• Letter of Acceptance
• Promissory Note and Loan Agreement
Funding:
• Funded by the Delaware American Rescue Plan Act (ARPA) for shortages in the healthcare field due to the COVID-19 pandemic
• Loan amount averages between $2,500 to $15,000 annually
Repayment:
• Interest-free while enrolled in an approved degree program
• Repayment begins 6 months after graduation depending on the length of the degree program
• Repayment plan options will depend on the degree type
- Certification programs: 1 to 3-year plans
- Associates, Bachelors, or Masters Degree programs: 5 to 7-year plans
- Doctoral (Ph.D.) programs: 7 to 11-year plans
Note: Terms of repayment of loans are covered through the promissory note and loan agreement
To apply, visit: https://delamed.org/student-financial-aid/
Contact: Giselle Bermudez, MS, Student Financial Aid Coordinator
email: gbermudez@delamed.org
phone: 302-733-1122
This program is supported by State and Local Fiscal Recovery Funds thru the Department of Treasury and State of Delaware [SLFRP0139].
39
From the Delaware Division of Public Health June 202




The Delaware Diabetes Wellness Expo is June 20 at Delaware Tech in Dover
The public is invited to the 21st Annual Diabetes Wellness Expo on June 20, 2023 at Delaware Technical Community College’s Terry Campus in Dover The free event will be held from 9:00 a.m. to 3:00 p.m. in the Del-One Conference Center, located at 100 Campus Drive. Lieutenant Governor Bethany Hall-Long will speak at noon.
The Expo is hosted by the Delaware Diabetes Coalition (DDC) and sponsored by the Division of Public Health's (DPH) Diabetes and Heart Disease Prevention and Control Program and the Physical Activity, Nutrition and Obesity Prevention Program. Bronze sponsors are AmeriHealth Caritas Delaware, Anodyne Pain & Wellness Solutions, Beebe Healthcare, Delaware First Health, and Tidal Health.
People with diabetes and pre-diabetes, caregivers, employers, and health professionals are encouraged to attend to learn how to prevent diabetes complications such as kidney failure, heart disease, stroke, lower-limb amputations, and adult blindness. Progression to type 2 diabetes can be prevented or delayed by losing weight, engaging in at least 150 minutes of physical activity weekly, and improving one's diet.
More than 30 exhibitors and educational seminars will provide information about diabetes management, nutrition, exercise, medication adherence, hearing, and mental health. Diabetes and blood pressure screenings, hearing screening, stress assessment, COVID-19 testing, and vaccinations are offered at no cost. Screenings are provided by DPH’s Kent County Mobile Unit, Beebe Healthcare, Delaware State University, Mast Audiology Services, PACE Your LIFE. A complimentary lunch is included for registered attendees. Register at https://www.dediabetescoalition.org/wellness-expo/ For event information, contact DDC at 302-519-6767 or director@dediabetescoalition.org Click here for diabetes resources or call 302-744-1020.
Advancing healthy lifestyles discussed



Nearly 300 public health policymakers, educators, health care providers, researchers, and nonprofit advocates of health and wellness attended the inaugural Advancing Healthy Lifestyles Conference on May 18, 2023 at Delaware State University. It was sponsored by the Division of Public Health’s (DPH) Physical Activity, Nutrition and Obesity Prevention Program and many community partners.
National, regional, and local leaders participated, including Dominique Dawes, who won gold on the 1996 U.S. Olympics gymnastics team, and Dalton Paxman, Regional Health Administrator for the U.S. Department of Health and Human Services. The theme of the conference was “Improving Health Through Equity.” Learn more at https://www.healthydelaware.org/CommunityPartners/Advancing-Healthy-Lifestyles
40 Delaware Journal of Public Health - June 2023
U.S. Olympian Dominique Dawes spoke at the May 18 Advancing Healthy Lifestyles Conference at Delaware State University (DSU) Photo by Carlos Holmes, DSU.
Ella M. Burton of Wilmington, Cynthia Newton of Frederica, and Sequoia Rent of DPH participate in a roundtable discussion. Photo by Donna Sharp.
After-school initiative teaches health
In January 2021, the Division of Public Health’s (DPH) Physical Activity, Nutrition and Obesity Prevention Program (PANO) launched its Advancing Healthy Lifestyles (AHL) initiative to reduce obesity and other chronic conditions, and to achieve health equity for schools, communities, and workplaces.
The AHL initiative fosters connections between youth-serving organizations and schools to support the health and well-being of youth and to strengthen community partnerships. The Centers for Disease Control and Prevention highlighted partnerships between school and providers of out-of-school-time programs such as before-school, after-school, and summer programs – to address health and educational inequities that widened during the COVID-19 pandemic.
Triple Play is a national Boys and Girls Club (BGC) healthy lifestyle program that focuses on the three components of a healthy self: mind, body, and soul. During 2022, the BGC of Delaware successfully implemented the Triple Play curriculum at nine sites throughout the state that provided healthy after-school activities to 507 youth Grades kindergarten to second grade were the focus in the fall of 2022; older children in grades 3 to 5 were the focus during the winter/spring of 2023 Data collection and a survey indicated that most participants reported gaining new knowledge and skills to live healthy lifestyles.
An example of Triple Play’s over 150 lessons for ages 6 to 18 is an “around the world” card activity that teaches youth the five MyPlate food groups. Another lesson has youth create a group dance to improve locomotor, acrobatic, and teamwork skills. Read the Triple Play Summary and Infographic on the Advancing Healthy Lifestyles webpage.

U.S. Surgeon General warns social media use can harm teens’ mental health
“We are in the middle of a national youth mental health crisis, and I am concerned that social media is an important driver of that crisis – one that we must urgently address,” said U.S. Surgeon General Dr. Vivek Murthy. Dr. Murthy issued the May 23 advisory, Surgeon General’s Advisory on Social Media and Youth Mental Health - PDF
Up to 95% of youth ages 13 to 17 report using a social media platform. A critical stage of brain development occurs during adolescence and childhood, making young people more vulnerable to social media’s harms such as violent and sexual content, bullying, and harassment.
The advisory cites research showing that adolescents who spend more than three hours per day on social media face double the risk of experiencing poor mental health outcomes, such as symptoms of depression and anxiety. Social media may also perpetuate body dissatisfaction, disordered eating behaviors, social comparison, and low selfesteem, especially among adolescent girls. Fortysix percent of adolescents aged 13-17 said social media makes them feel worse about their body image. Further, 64% of adolescents are “often” or “sometimes” exposed to hate-based content through social media. Studies have also shown a relationship between social media use and poor sleep quality, reduced sleep duration, sleep difficulties, and depression among youth. Social media use also compromises their sleep and valuable in-person time with family and friends.
Dr. Murthy advises parents and caregivers to establish tech-free zones to foster inperson relationships, teach kids about responsible online behavior and model that behavior, and report problematic content and activity. Children and adolescents should limit time on platforms, block unwanted content, be careful about sharing personal information, and reach out if they or a friend need help or see harassment or abuse on the platforms.

41 The DPH Bulletin – June 2023 Page 2 of 4
DelDOT’s bike rodeos teach safety to kids
The Delaware Department of Transportation (DelDOT) organizes bike rodeos for young cyclists in grades 3 to 5 at schools and community events. The bicycle safety clinics feature helmet fitting, a safety lecture about the rules of the road and what to always check on your bike before riding, and a ride on a miniature course set up in a parking lot.
To request a bike rodeo, contact John Fiori, DelDOT Bicycle Coordinator, at john.fiori@delaware.gov

Bike partners offer safety checkpoints
Beginning June 1, 12 bicycle safety checkpoints will be held this summer near Lewes and Rehoboth Beach The Delaware Department of Transportation (DelDOT) provides free helmets with courtesy fittings and free bicycle lights with courtesy installation for all ages Basic bike repairs can be completed
The checkpoints are sponsored by DelDOT, the Delaware State Police, Delaware Bicycle Council, and Sussex Cyclists. Click here for the schedule.
State law requires bicycle helmets for children under age 18. The public can purchase at-cost youth bike helmets from the Nemours Safety Store, located at the Alfred I. duPont Hospital for Children in the Anthony N. Fusco, Sr. Atrium, 1600 Rockland Road, Wilmington, Delaware. Bike helmets sell for $15 (instore purchases only). The store is generally open Monday through Friday, 10:00 a.m. to 3:00 p.m. Call 302-651-5279 for more information.
For safety information, visit the Delaware Bike Council, Safe Kids World Wide at www.safekids.org, and the Delaware Safe Kids Coalition at https://www.dhss.delaware.gov/dhss/dph/ems/safekids.html
Bicycle events, safety videos, and route maps
Delaware Bike Council https://deldot.gov/Programs/bike/biking_in_dela ware/index.shtml
Follow Delaware bicycle laws
Bicyclists of all ages must follow Delaware’s bike safety laws, including these:
• Use designated hand signals for left turns, right turns, and slowing down or stops



• Obey all traffic signs and signals, and ride in the same direction as traffic.
• Ride far enough to the right as judged safe by the bicyclist except when turning left. A bicycle may be ridden near the left-hand edge of the roadway only on one-way highways with two or more lanes and less than a 30 mile per hour posted speed limit.
• Children under 18 years must wear a properly fitted and fastened bicycle helmet while operating or riding on a bicycle on any property open to the public or used by the public for walking or driving motor vehicles. Bicycle helmets are recommended for all ages.
• Bicyclists must not wear ear coverings, including headsets, over both ears.
• A bicycle must only carry the number of persons that it was designed to carry.
• Bicyclists must have both hands available to operate the bicycle, with at least one hand on the handlebars at all times.
• A bicycle must be fitted with a rear, red reflector visible from at least 600 feet from a motor vehicle with lawful low beams

• When riding at night, a bicycle must be equipped with reflective material visible from both sides for at least 600 feet by a motor vehicle using low beams; or the rider must be visible from both sides for at least 500 feet if equipped with a lighted lamp.
To read Delaware bicycle laws, visit Title 21. Delaware Code, Chapter 41, Subchapter XII. Section 4198P pertains to the operation of electric bicycles.
For bicycling news, maps, and safety tips, visit the Delaware Bike Council at www.deldot.gov/Programs/bike
42 Delaware Journal of Public Health - June 2023
The DPH Bulletin – June 2023 Page 3 of 4
DelDOT
DelDOT
June celebrates LGBTQIA+ pride

June is LGBTQIA+ Pride Month, a historical and transformative celebration of individuality LGBTQIA+ stands for persons identifying as lesbian, gay, bisexual, transgender, queer or questioning, intersex, asexual, and more. These terms describe sexual orientation or gender identity.
The Centers for Disease Control and Prevention (CDC) is clear that the stigma, discrimination, and violence faced by the LGBTQIA+ community have devastating impacts on health. It can affect the ability to maintain relationships and feel safe. Bodies respond to long-lasting stress by raising stress hormones and keeping them raised, resulting in high blood pressure or a faster heart rate.
Discrimination and stigma devastate mental health, particularly when youth are rejected by their families or not affirmed by them When these youth are rejected or forced out of their homes, they become homeless, placing them at risk of poverty, poor health, and violence. According to the CDC, 40% of homeless youth identify as LGBTQIA+ Youth who face strong rejection from their families are eight times more likely to attempt suicide, six times more likely to develop high levels of depression, three times more likely to use illegal drugs, and three times more likely to engage in risky sexual practices Studies show that good social support for gay and bisexual young men leads to higher self-esteem and more positive mental health, the CDC reports For more information about LGBTQIA+ health, visit https://www.cdc.gov/msmhealth/stigma-anddiscrimination.htm. For LGBT health, visit https://www.cdc.gov/lgbthealth/transgender.htm. Crime victims can find resources at delawarevictimservices.org.
Parents and guardians of LGBTQIA+ individuals can find positive parenting practices at https://www.cdc.gov/healthyyouth/protective/positive parenting.htm.
Know Delaware’s fireworks law before July Fourth
When planning Fourth of July celebrations, citizens should leave fireworks operations to the professionals. Attempting to use fireworks can lead to serious consequences such as burns and property damage. The Delaware State Fire School reminds the public not to let children play with fireworks.

According to Delaware’s fireworks law (Title 16, Chapter 69), no person can store, sell, offer for sale, or possess any fireworks, firecrackers, rockets, torpedoes, Roman candles, fire balloons, or other fireworks without a permit. Exempt individuals are those established and manufacturing fireworks and those scaring birds away from agricultural crops.
Associations or companies seeking to have a public fireworks display must get a permit from the Office of the State Fire Marshal 30 days prior to the display. Discharging guns and explosive devices in, on, or into public streets or public spaces is prohibited
It is legal for individuals age 18 and older to use permitted fireworks during the “days of allowed use”: July 4, the third day of Diwali, New Year’s Eve, and New Year’s Day. Permitted fireworks are:
• Wood stick or wire sparklers coated with not more than 100 grams of pyrotechnic mixture per item
• Hand-held or ground-based sparkling devices which are nonexplosive and nonaerial and sometimes produce crackling or whistling sounds, and which contain 75 grams or less of pyrotechnic mixture per tube or a total of 500 grams or less for multiple tubes
• Toy pistols, toy canes, and toy guns, including those that use paper caps “manufactured in accordance with the United States Interstate Commerce Commission regulations”
• Snakes, glow worms, and smoke devices which contain 20 grams or less of pyrotechnic mixture
• Trick noisemakers such as party poppers, snappers, and drop pops, each containing 16 milligrams or less of pyrotechnic mixture.
Only individuals age 18 years and older can sell the above-listed fireworks only during the 30 days prior to the days of allowed use.
43 The DPH Bulletin – June 2023 Page 4 of 4
An Overview of Poverty in Delaware
Erin Nescott, M.S., Janice Barlow, M.P.A. and Miranda Perez-Rivera KIDS COUNT in Delaware, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
ABSTRACT
Delaware’s 2017-2021 five-year average poverty rate was 11.4%, which is lower than the rate of 12.6% throughout the United States as a whole. Poverty rates by race and ethnic background show disparities. Black Delaware residents were more than twice as likely to live in poverty as white Delawareans, with poverty rates of 17.8% and 8.4%, respectively, while Asian individuals had a poverty rate of 10.5%. Hispanic or Latino/x individuals of any race were the most likely to experience poverty and had a five-year average poverty rate of 18.2%. Tracking the overall poverty rate (most commonly through the American Community Survey 5-Year Averages) is valuable when studying trends over time but lacks the power to display the true economic status of individuals and families. Access: work, income supports, shelter, food, and healthcare all complete each whole person. Level of access within each of these sectors of life determines well-being, and varies based on race and ethnic background, geography, and age. A new challenge is now faced as the Public Health Emergency (PHE) has ended, repealing a multitude of supports with the risk of putting individuals and families into a new phase of crisis.
INTRODUCTION
This overview of poverty presents basic parameters of the complex problem of poverty in the state of Delaware. The definition of poverty status is explored in-depth. Additional data describing conditions related to poverty status are described in order to provide context to supplement official poverty rate data. According to the Department of Health and Human Services’ Federal Poverty Guidelines, the poverty threshold for a family with one parent and two children was $23,030 in 2022.1 Income that counts towards this threshold includes earnings, unemployment compensation, workers’ compensation, Social Security, Supplemental Security Income, and public assistance. Noncash benefits such as food assistance are not included. The full population count of the census, from which the American Community Survey data is derived, takes place every ten years, with the most recent one in 2020. For many estimates, Census data allows for proportion estimation and standardization for comparison on indicators across the region.
The COVID-19 pandemic has and will continue to greatly influence future discussions about poverty. Reportable data today show that several policies promoted economic security through meeting of basic needs. The American Rescue Plan Act of 2021 (ARPA) increased the value of the Child Tax Credit (CTC), made the credit fully refundable, and sent Americans with children advance payments on the tax credit starting in July 2021.2 The CTC decreased the number of children living in poverty by roughly 40 percent nationwide.3 This credit was a temporary measure that didn’t carry through to 2022. Additionally, the credit did not extend to nearly two million American children – 85 percent of them U.S. citizens – living in poverty with an unauthorized immigrant parent.4
The Public Health Emergency (PHE) provided enhanced social support to residents across the nation, with each state having some flexibility in implementation. Much of this brief will explore if the data reflect residents’ experiences throughout the pandemic, discussing the financial impact of
COVID-19 on Delawareans. The PHE improved access income and employment supports, shelter, food, and healthcare. The federally declared Public Health Emergency expired May 11, 2023,5 however, there are a variety of end dates associated with the multiple PHE-related safety net programs which were put into place to combat the pandemic.
POVERTY OVERVIEW
The Census Bureau uses a variety of dollar value thresholds that vary by family size and composition to determine who is in poverty.6 The poverty measure was established in 1964 based on research indicating that families spent about one-third of their income on food. A family is officially classified as poor if its cash income (wages, pensions, social security benefits, and all other forms of cash income) falls below the poverty threshold. While the thresholds are updated each year for inflation, the measure is widely acknowledged to be outdated because today, food comprises a much lower percentage of an average family’s expenses than it did in the sixties, while the costs of housing, child care, health care, and transportation have increased substantially. Additional criticism of the federal poverty threshold is that the measure does not take into account non-cash resources available to struggling American families including SNAP, tax credits, or housing and child care subsidies. The measure also does not vary by geographic region. To address these limitations, the U.S. Census Bureau publishes a Supplemental Poverty Measure (SPM) which provides decision makers with another way to evaluate the effects of anti-poverty programs. Data from this measure show that social safety net programs were responsible for much of a 59 percent decline in child poverty from 1993 to 2019.7 Using Census survey data for “Poverty Status in The Past 12 Months,” Delaware’s 2017-2021 five-year average poverty rate was 11.4%, which is lower than the rate of 12.6% throughout the United States as a whole. When compared to other states in the region for the same measure, Delaware’s poverty rate was higher than either Maryland (9.2%) or New Jersey (9.8%) but lower than Pennsylvania (11.8%).8
44 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.009
Delaware’s five-year average poverty rate has increased up until recently. When the ACS began reporting five-year averages (2006-2010 estimates), the state’s poverty rate was 11.0%. It reached 11.8% for the 2015-2019 estimates. The 2016-2020 and 2017-2021 estimates showed a decline in the state for the first time in over 15 years, with Delaware’s average poverty rate holding at 11.4%. Following the same trend, the U.S. poverty rate has declined since the 2010-2014 average of 15.6%, with the most recent being 12.8% for 2016-2020 and 12.6% for 2017-2021.8
Examining by age groups for this same measure reveals that Delaware’s children (under 18 years old) had the highest rate of poverty at 17.3%, followed by adults in their working years (1864) at 13.8%. Seniors (65 and older) had the lowest poverty rate of any age group at 6.3%.9
Households with children under age 18 had a higher rate of poverty than households without children. Families with a female head of household had the highest five-year poverty rate at 21.3%; when broken down, the rate is 29.6% for female families with children under 18 and 36.5% if the children are under age 5.9
Poverty rates by race and ethnic background also show disparities. Black Delaware residents were more than twice as likely to live in poverty as white Delawareans, with poverty rates of 17.8% and 8.4%, respectively, while Asian individuals had a poverty rate of 10.5%. Hispanic or Latino/x individuals of any race were the most likely to experience poverty and had a five-year average poverty rate of 18.2%.9
By geographic analysis at the county level, the overall poverty rate was highest in Kent County (13.3%), whereas New Castle County (10.6%) and Sussex County (12.1%) were closer to the state average of 11.4%.8 Census county divisions (CCDs) are statistical geographic entities established cooperatively by the Census Bureau and officials of state and local governments; these smaller units, broken down by age group, assist in further understanding of Delaware’s poverty distribution. The map in figure 1 provides further detail. Based on 2017-2021 estimates, the five CCDs with the highest rates of poverty for children under age 18 are Wilmington (41%), Laurel-Delmar (33%), Bridgeville-Greenwood (32%), Seaford (27%), and Dover (27%).
For adults, the breakdown is as follows: Wilmington (19%), Seaford (17%), Greater Newark (16%), Dover (13%), and Kenton (13%).9
Individuals living in poverty are defined as those with incomes under 100% of the poverty level. However, individuals living in near-poverty (defined as 101%-124% of the poverty level) also experience economic hardships. Children were the most likely to live in near-poverty; while 17.3% were living in poverty, an additional 4.9% were living in near-poverty. Adults 65 and older were the next likely to live in near poverty, at 3%, followed by adults 18-64 at 2.9%.8
Solely referencing poverty rates does not tell the whole story about the economic situation of Delawareans. Factors including accessibility of employment opportunities, income support, shelter, food, and healthcare indicate the level of economic hardship for a community. We must consider the status of all basic needs for Delaware families.
BASIC NEEDS Access to Work and Income Supports
For the 2020-current timeframe, the peak unemployment rate for the U.S. was April 2020 at 14.7% unemployment, and for Delaware was in May 2020 at 13.4% unemployment. In January of 2021 the U.S. rate was 6.3%, the Delaware rate at 5.7%. Latest available data are for February 2023, charting the U.S. rate at 3.6%. The Delaware rate has held steady at 4.6% since December of 2022.10
During the pandemic, all citizens collecting unemployment insurance benefits in a week also received $600.00 per week from the Federal Pandemic Unemployment Compensation (FPUC) program, up through the end of July 2020.11 Delaware issued Pandemic Unemployment Assistance (PUA) from March to December 2020, with the maximum per person allowance at 39 weeks.11
Cash public assistance is an important resource to those living in poverty. Cash assistance programs include Temporary Assistance to Needy Families (TANF),12 which provides federal assistance to families with minor children, and state General Assistance (GA) funds, which help low-income people who may not qualify for other federally funded programs.6 As of October 2022, in Delaware, a four person family must have a maximum net monthly income below $1,735 to be eligible for TANF.13 Average annual temporary cash assistance (which totals TANF and GA) was as follows for the region: New Jersey with the highest at $4,430, followed by Maryland at $3,830, then Pennsylvania at $2,857 and Delaware the lowest with $2,510. New Jersey is the only state with an average above the national, which is $3,875.9
Delaware’s Division of Social Services issued emergency cash benefits beginning in March 2020. Households with open TANF and GA cases who were not already receiving the maximum benefit amount received an emergency cash benefit. TANF has specific work requirements to receive benefits, but during the pandemic these were lifted. Benefits will go back to pre-pandemic operation starting in June 2023. TANF and GA clients will have to submit a new health assessment form to be eligible for a medical exemption after their current exemption expires or the public health emergency ends.14
Additional cash assistance flowed because of the COVID-19 pandemic. At the federal level, the Internal Revenue Service issued first, second and third Economic Impact Payments.15
At the state level, House Bill 360 created the 2022 Delaware Relief Rebate Program. This legislation created a “relief rebate,” which is a direct payment of $300 per adult Delaware resident.16
Childcare costs also play into a the budget of a family. One form of support is Purchase of Care (POC). To be financially eligible for child care assistance, a family’s gross monthly income must be at or below 185% of the FPL for the family size. POC vouchers cover a portion of the cost of care, and pre-COVID, many families paid co-pays to supplement. These co-pays were waived during the pandemic, starting in April 2020, but will restart in June 2023.
Access to Shelter
Delaware’s yearly PIT (Point in Time) count provides the most up to date information on the state of housing and homelessness in Delaware. On the night of the 2022 PIT Count, 2,369 people were experiencing homelessness, the highest PIT Count in Delaware to-date. The number of total people counted more
45

46 Delaware Journal of Public Health - June 2023
Figure 1. Delaware’s Poverty Distribution9
than doubled since the count in January 2020, and the number of households with children experiencing homelessness has almost tripled since 2020, from 136 families to 389 families. One in three people experiencing homelessness was a child under the age of 18, the number of veterans experiencing homelessness increased to 93 households in 2022, the highest number since 2016. Sixty-one percent of people experiencing homelessness identified as Black/African American; Delawareans who are Black/African American are 3.5x more likely to experience homelessness than white residents.
The pandemic brought a shortage of emergency shelter beds (due to social distancing safety protocols), putting stress on Delaware’s citizens who were facing record unemployment and a continued public health crisis. Starting in 2020, vouchers for non-congregate hotel/motel sheltering were given as a safe alternative to traditional group shelter setups. In 2022 there was a major increase in the number of year-round Emergency Shelter beds due primarily to the opening of the NCC Hope Center. The majority of the overflow beds in 2022 were emergency hotel/ motel vouchers.17 However, this program was always meant to be temporary. The Delaware Department of Health estimates that over 14,600 people in the state have used such vouchers. Funds for this relief ran out over the summer of 2022.18
For those housed but at risk of homelessness, the Delaware State Housing Authority created the Delaware Housing Assistance Program (DEHAP) in early 2020. The program provides emergency housing assistance to renters specifically, in light of the COVID-19 pandemic. Demand was very high for this program, and due to that (and recent U.S. Treasury policy changes) DEHAP is now closed to new applications and recertifications.19
Access to Food
The Supplemental Nutrition Assistance Program (SNAP) provides assistance to households with incomes at 200% or below the Federal Poverty Level. In Delaware, 2016-2020 estimates recorded that 10.6% of people received temporary cash assistance, and for the 2017-2021 estimates that dropped slightly to 10.5%. This was nearly two percentage points lower than the national statistic of 12.4%. Per COVID-19 assistance legislation, Delaware households currently receiving SNAP benefits benefited from waived work requirements and were eligible to receive at least $95 in extra benefits at the end of each month. Future data will reflect the impact of work requirement reinstatement and this decrease of resources has on families, but there is great concern that this will substantially increase food insecurity as SNAP provides the foundation for low-income households’ health and well-being, lifting participants out of poverty.13
The Special Supplemental Nutrition Program for Women, Infant and Children (WIC), is a federal nutrition program (through the United States Food and Drug Administration (USDA)) that specifically helps pregnant women, new mothers, and young children. In 2022, Delaware saw an average of 3,664 women, 2,678 infants, and 9,848 children participate.20 WIC is a financial support that is set in the context of nutrition and health guidance for families.
Nationally, There has been a 1.2 percent increase in WIC participation overall and a 8.7 percent increase in WIC participation among children (February 2020 to February 2022).21
As the PHE unwinds, there are coverage risks to consider. WIC providers have relied on COVID waivers for service delivery adjustments, primarily to provide certifications via remote health. In February 2023, the USDA ruled to let WIC agencies keep using remote certification models, if necessary health data is collected within 60 days of the remote appointment. When considering WIC programming, in October 2022, Delaware had a cash value benefit increase for fruits and vegetables: $49 for breastfeeding women, $44 for pregnant and postpartum women, and $25 for children.22
Access to Healthcare
Enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) can be an indicator of the economic well-being of the state’s population. Throughout the pandemic, the PHE guidelines prohibited disenrollment of Medicaid recipients,23 therefore the 2021 numbers are higher across the region than we would typically see. Disenrollment was allowed when a person asked specifically to be taken off rolls, if a person died, or if a person moved out of state. The Delaware Medicaid program covers individuals living at or below 138% of the poverty level, and CHIP covers children below 200% of the poverty level who are not covered by Medicaid. However, eligibility criteria for Medicaid and CHIP coverage varies by state. When considering December 2021 enrollment numbers, Delaware is highest with 28.3% enrolled, followed by Pennsylvania at 27.2%, then Maryland at 25.7%. New Jersey is the only state with enrollment below a quarter of their population, at 22.4%. United States in total is at 26.3%, making Delaware the only state in the region to exceed the national statistic.24
Medicaid unwinding began on April 1st, 2023. Medicaid saw over a 25% increase in recipients between April 2020 and February 2023. An administrative lift exists as members will need to renew their Medicaid over the course of the unwinding period during the unwinding period (through June 2024). Unfortunately, this will allow for some automatic end of coverage, with the exception of a few protected populations.25 Loss of secure health coverage can have catastrophic impacts on overall wellbeing; paying out of pocket for health expenses has the unfortunate potential to put individuals and families at risk of poverty.
Predictions were made regarding loss of coverage, and data will soon show the true impact of unwinding. Groups who experienced the greatest growth, including children, will experience the biggest enrollment declines. Estimates say that more than of 6.7 million children- disproportionately children of color- could lose their Medicaid/CHIP coverage”26 A big concern is disenrollment because of administrative churn occurs, which occurs when state is missing information to confirm eligibility.23
Medicaid meets a basic need by providing critical health insurance (which through the marketplace can become a high cost burden, and the ripple effect is of high concern as well; Medicaid eligibility commits eligibility for SNAP and school lunch programs.27
47
CONCLUSION
Understanding this established foundation of poverty is essential for a reference baseline. Initiatives exist27–31 which seek to quantify alternate measures of poverty. These consider the experience of households with income above the FPL, but below the basic cost of living, survival (or basic needs) budgets, expenditure points at the minimum for basic needs, thresholds of financial survival considering geographical location, and an index that captures poverty through three dimensions of well-being – monetary poverty, education, and basic infrastructure service. The end of the Public Health Emergency ruling32 will have an impact on financial stability, and monitoring of the extent of impact will be necessary for service delivery. Delawareans are encouraged to call or text Delaware 21133 for free support on accessing fundamental resources. Data such as the Household Pulse Survey34 will enable “close to real-time” updates on the status of basic need acquisition for families, specifically including the following queries: paying for childcare and cost, experienced loss of employment income, employment status, applying for and receiving unemployment benefits, food sufficiency, and health insurance status. Examining corresponding trends for each table can predict the financial wellbeing of Delawareans. All of the aforementioned supports to citizens (accessibility of employment opportunities, income support, shelter, food, and healthcare indicate the level of economic hardship for a community) are woven together to determine their poverty experience.
Ms. Nescott may be contacted at eplynch@udel.edu
REFERENCES
1. Office of the Assistant Secretary for Planning and Evaluation (ASPE). (2022). 2022 Poverty guidelines: 48 contiguous states (all states except Alaska and Hawaii). Retrieved from: https://aspe.hhs.gov/sites/default/files/ documents/4b515876c4674466423975826ac57583/Guidelines-2022.pdf
2. Center on Poverty & Social Policy. (2021, Nov 30). October child tax credit payment kept 3.6 million children from poverty. Colombia University. Retrieved from: https://www.povertycenter.columbia.edu/news-internal/monthlypoverty-october-2021
3. Robinson, J. R., & Welch, A. (2022, Jan 14). Just taxes blog: The compelling data and moralcase for continuing the child tax credit expansion. Institute on Taxation and Economic Policy. Retrieved from: https://itep.org/the-compellingdata-and-moral-case-for-continuing-thechildtax-credit-expansion/
4. Suro, R., & Findling, H. (2021, September 2). Tax equity for immigrants: The indispensable ingredient for remedying child poverty in the United States. Journal on Migration and Human Security, 9(4). https://doi.org/10.1177/23315024211034836
5. U.S. Department of Health & Human Services. (2023, Feb). Fact sheet: COVID-19 public health emergency transition roadmap. Retrieved from: https://www.hhs.gov/about/news/2023/02/09/fact-sheet-covid-19public-health-emergency-transition-roadmap.html
6. United States Census Bureau. (n.d.). American Community Survey and Puerto Rico Community Survey 2021 subject definitions. Retrieved from: https://www2.census.gov/programs-surveys/acs/tech_docs/subject_ definitions/2021_ACSSubjectDefinitions.pdf
7. Thomson, D., Ryberg, R., Harper, K., Fuller, J., Paschall, K., Franklin, J., & Guzman, L. (2022). Lessons from a historic decline in child poverty. Child Trends. Retrieved from: https://www.childtrends.org/publications/lessons-from-a-historicdecline-in-child-poverty
8. United States Census Bureau. (n.d.). American Community Survey. Table S1701: Poverty status in the past 12 months
9. United States Census Bureau. (n.d.). American Community Survey. Table DP03: Selected economic characteristics
10. Delaware Department of Labor. (n.d.). Local area unemployment statistics. Retrieved from: https://labor.delaware.gov/divisions/oolmi/laus/
11. Delaware Department of Labor. (n.d.). Unemployment benefits. Retrieved from: https://labor.delaware.gov/divisions/ unemployment-insurance/unemployment-benefits-faqs/peuc/
12. Delaware Health and Human Services. (n.d.). Temporary assistance to needy families. Retrieved from: https://dhss.delaware.gov/dss/tanf.html
13. Center on Budget and Policy Priorities. (2021, Jul). More adequate SNAP benefits would help millions of participants better afford food. Retrieved from: https://www.cbpp.org/research/food-assistance/more-adequate-snapbenefits-would-help-millions-of-participants-better
14. Delaware Department of Health and Human Services. (n.d.). Important changes in benefit programs in response to COVID-19. Retrieved from: https://www.dhss.delaware.gov/dhss/dss/COVID19.html
15. Internal Revenue Service. (n.d.). Economic impact payments. Retrieved from: https://www.irs.gov/coronavirus/economic-impact-payments
16. Delaware Department of Finance. (n.d.). The 2022 Delaware relief rebate program has ended. Retrieved from: https://finance.delaware.gov/2022-delaware-relief-rebate-program/
17. Delaware Continuum of Care. (2022). Point in time count & housing inventory count, 2022 Report. Retrieved from: https://static1.squarespace.com/static/59ca9d72268b96cb977e74fd/t/ 6282429bd806ef23da3ffa7c/1652703901307/2022_PIT+Report_ w+attachments_FINAL.pdf
18. Metraux, S., Solge, J., Mwangi, O., & Culhane, D. (2021). An overview of family homelessness in Delaware: A report to Housing Alliance Delaware. University of Delaware Center for Community Research and Service
19. Delaware Housing Assistance Program (DEHAP). Rental assistance - frequently asked questions. Retrieved from: https://decovidhousinghelp.com/frequently-asked-questions/
20. USDA Food and Nutrition Service. (2023, Mar). WIC agency level monthly spreadsheets. Retrieved from: https://www.fns.usda.gov/sites/default/files/resource-files/ WICAgencies2022ytd-3.xlsx
21. Food Research & Action Center. (2022, October). WIC during COVID-19. Retrieved from: https://frac.org/wp-content/uploads/wic-during-covid-19-2022.pdf
22. Delaware Health and Social Services. (n.d.). Let WIC buy your fruits and vegetables. Retrieved from: https://delaware.wicresources.org/wp-content/uploads/sites/4/2022/10/ DE_WIC_Insta.pdf
48 Delaware Journal of Public Health - June 2023
23 First Focus on Children. (2023, Feb). Fact sheet: Medicaid unwinding: How to protect children from losing coverage.
Retrieved from:
https://firstfocus.org/resources/fact-sheet/medicaid-unwinding-how-toprotect-children-from-losing-coverage
24. Medicaid.Gov. (n.d.). Monthly Medicaid & CHIP application, eligibility determination, and enrollment reports & data.
Retrieved from:
https://www.medicaid.gov/medicaid/national-medicaid-chip-programinformation/medicaid-chip-enrollment-data/monthly-medicaid-chipapplication-eligibility-determination-and-enrollment-reports-data/ index.html
25. Delaware Health and Social Services. (2023, Feb). Delaware’s plan for unwinding from the COVID-19 public health emergency. https://dhss.delaware.gov/dhss/dmma/files/covid19_phe_ unwind_20230220.pdf
26. Brooks, T. (2022, Aug). An estimated 3.8 million eligible children could lose Medicaid due to administrative churn during the unwinding. Georgetown University Health Policy Institute, Center for Children and Families. Retrieved from: https://ccf.georgetown.edu/2022/08/22/millions-of-eligible-childrencould-lose-medicaid-due-to-administrative-churn-during-the-unwinding/ 27 United for ALICE. (n.d.). https://www.unitedforalice.org/
28 National Center for Children in Poverty. (n.d.). Basic needs budget calculator. http://frs.nccp.org/tools/frs/budget.php
29 Economic Policy Institute. (n.d.). Family budget calculator. https://www.epi.org/resources/budget/?gclid=CjwKCAjwge2iBhBBEi wAfXDBR-N7-3Qru4AfJqxKL9JaIP9HV1hrILO28ziG087yUUIKQ9 KCiJ0HhxoCXSYQAvD_BwE
30. Fitzgerald, J., & Moffitt, R. A. (2022, Mar). The supplemental expenditure poverty measure. Johns Hopkins University. https://www.brookings.edu/bpea-articles/the-supplemental-expenditurepoverty-measure-a-new-method-for-measuring-poverty/
31. The World Bank. (n.d.). Multidimensional poverty measure. https://www.worldbank.org/en/topic/poverty/brief/multidimensional-poverty-measure
32 Ashbrook, A. (2023, Mar). Medicaid unwinding will hurt families struggling to put food on the table. Food Research & Action Center. Retrieved from: https://frac.org/blog/medicaid-unwinding
33. Delaware 211. (n.d.). Retrieved from: https://delaware211.org/
34. United States Census Bureau. (n.d.). Household pulse survey. Retrieved from: https://www.census.gov/programs-surveys/household-pulse-survey/data.html
LOWERING YOUR HIGH BLOOD PRESSURE IS EASIER THAN YOU THINK. There are FREE classes to help you get healthier and stay that way. HealthyDelaware.org/HealthyHeart 302-208-9097 49
Considering the Benefits Cliff Embedded in the Relationship between Housing and Health
Dorothy Dillard, Ph.D.
Director, Center for Neighborhood Revitalization and Research, Delaware State University Bianca Mers, M.C.R.P.
Community Investment Analyst, REACH Riverside
ABSTRACT
This Commentary introduces the reality of the benefits cliff into the housing and health relationship. Improving both housing and health requires addressing the benefits cliff facing extremely low- and low-income people. Those living below the poverty line are at greatest risk of poor, inadequate, and unhealthy living conditions. They are also the group most at risk for losing benefits and economic supports on their journey toward economic self-sufficiency. Addressing the housing crisis in Delaware demands that we recognize the benefits cliff looming on the horizon for extremely low- and low-income families struggling toward self-sufficiency. Effective policies and interventions, at a minimum, need to be informed by the experiences of those struggling to navigate the benefits cliff and achieve economic mobility and need to be integrated across housing, economic benefits, and health care.
Research has established that housing is a health issue and that the worse the housing situation, the worse the impact on health. Those experiencing homelessness, particularly chronic homelessness, for instance, experience high rates of physical health issues, chronic diseases, substance abuse, and mental health challenges. Furthermore, health issues cause as well as are exacerbated by homelessness.1 Housing that is poor quality or in disrepair increases the incidence of injuries, asthma, cancer, cardiovascular disease, and other health issues. Living in unhealthy housing also worsens mental health, in part due to the stress of living in unsafe and unhealthy environments. Conversely, affordable housing reduces negative health outcomes, because a lower proportion of income is dedicated to housing and greater proportion is available for food and health care.2
Accessing healthy living conditions is an economic issue for those most likely to be living in poor housing conditions that negatively impact health. To improve health and housing conditions for extremely low- and low-income families requires addressing both the availability and the access to healthy housing. According to the Housing Alliance Delaware report,3 Delaware is short more than 21,000 additional affordable housing units to meet the needs of extremely low-income families. Second, affordable housing must be affordable. Low income and extremely low-income Delawareans need to work more than two minimum wage jobs to afford a Fair Market Rent apartment. Even if this was reasonable, the path to attaining affordable and quality housing is interrupted by the benefits cliff.
The benefits cliff, in simple terms, is the point on the economic mobility path where those dependent on governmental benefits and entitlements increase income but not enough to cover the additional expenses associated with the loss of benefits. The benefits cliff emerged as an unanticipated consequence of implementing the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA), commonly referred to as Welfare to Work. The welfare reform legislation aimed to reduce dependency on government assistance and to increase self-sufficiency. Initial studies on the impact of PRWORA showed significant increases in employment among welfare recipients;
however, the employment was unstable and temporary.4 Studies looking at the impact of individual benefit programs on work show that food stamps5 and housing6 have negative effects on incentives to transition from welfare to work. On the other hand, several studies show that although childcare assistance appears to have the most positive impact, it also has the largest cliff effects.4 An extensive study in Colorado shows how families dependent on government benefits “strategize” to avoid the benefits cliff and identify the most reasonable and least risky path toward selfsufficiency.7 Prenovost and Youngblood documented the stress created trying to navigate the benefits cliff.8
Significant attention has been given to identifying the point where work pays off, referred to as the effective marginal tax rate (EMTR).4,9 The EMTR is the percentage of any additional earned income that a household pays in taxes or loses in government benefits. As Dolan notes, the EMTR creates a poverty trap where the risks and gains of working become disincentives and barriers to self-sufficiency and economic mobility.9 EMTR analyses have produced various models of economic mobility out of welfare to self-sufficiency, including modeling combining various types of benefits.4,9 Typically, however, EMTR modeling fails to take into account factors associated with the readiness for work. As Hauan and Douglas point out, most welfare recipients face at least one barrier and many encounter multiple barriers preventing readiness for stable and sustainable work.10 They identified the most common barriers, in order of most frequently identified, as not having earned a high school diploma or GED, unmet childcare needs, mental health issues, transportation issues, limited work experience, unstable housing, and physical health problems.
This research suggests that navigating the benefits cliff requires welfare recipients meet a set of criteria considered necessary for stable and sustainable work, a status necessary to access healthy housing. Assisting residents dependent on government assistance become eligible and prepared to cross the benefits cliff to become economically self-sufficient and eligible for housing that does not negatively affect health has become a critical issue in comprehensive revitalization efforts. Clearly, building new,
50 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.010
healthy housing is not enough. Extremely low- and low-income families need significant assistance becoming economically eligible for the housing. REACH Riverside’s experience demonstrates the interconnected relationship among poverty, health, and housing.
The REACH Riverside Development Corporation was formed in 2017 to remove the barriers to prosperity and well-being facing residents of Wilmington’s Riverside neighborhood, a community experiencing the devastating impacts of decades of racial discrimination and disinvestment. REACH is the managing partner of The WRK Group, a group of three nonprofits (REACH Riverside, Kingswood Community Center, and The Warehouse) working together to implement the Purpose Built Communities model, a holistic approach focused on housing, education and health initiatives. REACH is leading a comprehensive revitalization of the Riverside community in NE Wilmington, which includes creating 700 units of mixed-income housing (Imani Village) along with education and health oriented initiatives. Phase one of Imani Village (74 units) was completed in December 2022. Construction of Phase two was finished in May 2023, bringing another 67 units on stream. Five hundred fifty two more rental units are planned in Phases three through seven, along with about 100 homes for ownership. In support of this transformation in the built environment, REACH works closely with service partners Kingswood Community Center and The Warehouse to provide social service programs for all ages. This has included creating a cradle-to-college/career pipeline between Kingswood’s Early Learning Academy, EastSide Charter School, and The Warehouse as well as providing on-site medical services to the community through a partnership with ChristianaCare.
As with all the WRK Group efforts, the new housing plan prioritizes current residents living in Wilmington Housing Authority (WHA) housing. In assessing eligibility for the new housing, approximately 40% of the WHA families were not eligible primarily as the result of past due rent and utility bills. REACH worked with Kingswood Community Center to enroll residents in Kingswood’s EMPOWER program. EMPOWER assists residents of Riverside and surrounding neighborhoods obtain economic self-sufficiency. At intake, EMPOWER clients with assistance from their navigational coach complete a comprehensive assessment. A 2023 analysis of intake assessment data showed that over half of the EMPOWER clients’ income situation, employment situation, and/or food situation were assessed as in crisis or vulnerable. The credit situation for one third of the clients was in crisis or vulnerable and one fourth were living in housing that was assessed as in crisis or vulnerable. The large majority of EMPOWER clients are WHA residents and for them in crisis or vulnerable housing situations indicates that they are at risk of eviction. The intake assessment data underscores the multiple programming needs of extremely low- and lowincome families. One of the biggest barriers faced by EMPOWER staff and clients in developing plans to achieve economic selfsufficiency to meet the inter-related and multiple needs is the benefits cliff. EMPOWER clients, like many extremely low- and low-income families, cannot simply work more or obtain better paying jobs to become economically independent because they risk losing benefits, most significantly those related to childcare and healthcare. This barrier to economic stability and self-sufficiency also creates barriers to accessing the new healthy housing designed specifically for Riverside residents. The EMPOWER staff and the REACH leadership are actively
exploring options for bridges across the benefits cliff but these bridges are, in part, dependent on policy changes. Programmatic developments without complimentary and supportive policy changes will be ineffective and possibly infeasible.
Policies to avoid the benefits cliff or mediate its negative effect on the transition to self-sufficiency are limited and vary greatly by state. The National Conference of State Legislatures (NCSL)11 and the Federal Reserve12 produced reports defining and describing the benefits cliff. The Alliance for Strong Families and Communities categorizes policy efforts into four categories: 1) policies modeling or adapting the Earned-Income Tax Credit; 2) policies ensuring continued access to benefits; 3) policies eliminating some assets, such as cars and savings accounts, in deciding benefits levels; and 4) policies excluding portions of income in benefits calculations.13 The NCSL report provides an overview of state level efforts addressing the benefits cliff. The report notes that 16 states enacted legislation to mitigate the impact of the benefits cliff. Delaware was not one of those states and to date has not proposed benefits cliff mitigation legislation The most comprehensive initiative, undertaken by five New England states, piloted both policy and program level changes to mitigate the negative effects of the benefits cliff.14
Most state level efforts continue to address welfare policies individually when the reality is recipients must navigate the benefits cliff considering all sources of assistance. Dolan9 and Richardson and Blizard4 suggest that the current benefits system, rather than policies, is structured in a way that discourages participants from becoming fully self-sufficient, prohibiting economic mobility. Dolan highlights the need to create individualized approaches because there is a matrix of benefits, income sources, and personal factors that must be considered for a family to traverse the benefits cliff.9 Richardson and Blizard are bolder in their recommendations, suggesting terminating all social programs as an option.4 Other options included creating a longer glide path, universal basic income, and private sector creation of non-taxable fringe benefits, such as childcare assistance.
Addressing the housing crisis in Delaware as well as improving health and economic stability demands that we address the benefits cliff looming on the horizon for extremely low- and low-income families struggling toward self-sufficiency. Effective policies and interventions, at a minimum, need to be informed by the experiences of those struggling to navigate the benefits cliff and achieve economic mobility. In other words, policies need to data driven. And, effective policies and interventions must be integrated. Siloed policy development will not effectively address the benefits cliff preventing economic self-sufficiency and access to affordable, healthy housing. There is not a single pathway from dependence on government assistance to self-sufficiency. Similarly, there is not a linear continuum of housing options paralleling a linear continuum of economic mobility. Multiple entrance ramps with varying lengths across the benefits cliff need to be created in collaboration with housing, social services, healthcare, educational, workforce, government, and private sector partners. Given our size and promising comprehensive revitalization efforts, Delaware has an opportunity to model integrated policy changes that bridge the benefits cliff and support extremely low- and low-income Delawareans on their journey toward economic self-sufficiency, health, and affordable, quality housing.
Dr. Dillard may be contacted at ddillard@desu.edu.
51
REFERENCES
1. Medline Plus. (n.d.). Homelessness and health. Retrieved from https://medlineplus.gov/homelessnessandhealth.html
2. Pew Trusts. (2018). Health impact project. Robert Wood Johnson Foundation. Retrieved from https://www.pewtrusts.org/ en/projects/health-impact-project/health-impact-assessment
3. Housing Alliance Delaware. (2021). Housing and homelessness in Delaware: Crisis to recovery. Retrieved from https://www.housingalliancede.org/_files/ ugd/9b0471_4e6ce9e787774669884d62bab9a6200e.pdf
4. Richardson, C., & Blizard, Z. (2022). Benefits cliffs, disincentive deserts, and economic mobility. Journal of Poverty, 26(1), 1–22. https://doi.org/10.1080/10875549.2020.1869665
5 Hoynes, H. W., & Schanzenbach, D. W. (2012). Work incentives and the food stamp program. Journal of Public Economics, 96(1–2), 151–162. https://doi.org/10.1016/j.jpubeco.2011.08.006
6 Jacob, B. A., & Ludwig, J. (2012). The effects of housing assistance on labor supply: Evidence from a voucher lottery. The American Economic Review, 102(1), 272–304 https://doi.org/10.1257/aer.102.1.272
7. East, J. F., & Roll, S. J. (2010). Child care and low income families: Coping with the cliff effect. The Women’s Foundation of Colorado. Retrieved from: https://www.wfco.org/document.doc?id=58
8. Prenovost, M. A., & Youngblood, D. C. (2010). Traps, pitfalls, and unexpected cliffs on the path out of poverty. Poverty & Public Policy, 2(2), 239–268. https://doi.org/10.2202/1944-2858.1053
9 Dolan, E (2020). New research revives debate over a poverty trap. Niskanen Center. Retrieved from https://www.niskanencenter.org/new-research-revives-debate-over-a-poverty-trap/

10 Hauan, S., & Douglas, S. (2004). Potential employment liabilities among TANF recipients: A synthesis of data from six state TANF caseload studies. U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Retrieved from: http://aspe.hhs.gov/hsp/leavers99/emp-liab04/index.htm
11. National Conference of State Legislatures. (2022, Nov). Introduction to benefits cliff and public assistance programs. Retrieved from https://www.ncsl.org/human-services/introduction-to-benefits-cliffsand-public-assistance-programs
12. Chiarenza, G. (2022, Dec). A hand up, not a hand out, to cross the benefits cliff. Retrieved from https://fedcommunities.org/stories/benefits-cliffs-hand-up-not-handout/
13. Alliance for Strong Families and Communities. (2022). Finding policy solutions to the benefits cliff. Retrieved from https://www.alliance1.org/web/news/2020/jan/finding-policy-solutionsbenefits-cliff.aspx
14. Aspen Institute. (2018, Dec). Whole family approach to jobs: 6 state policy brief addressing benefit cliffs. Retrieved from https://ascend.aspeninstitute.org/wp-content/uploads/2020/12/wholefamily-approach-to-jobs-6-state-policy-brief-addressing-benefit-cliffs.pdf
52 Delaware Journal of Public Health - June 2023
IT’S TIME TO SCHEDULE A COLON CANCER SCREENING.
You should talk to your health care provider about a colon cancer screening if:
You’re 45 or older.
Are experiencing symptoms, including bloody stools, cramping, and weight loss.
Don’t have a health care provider?
A screening nurse navigator can help you schedule a screening at no extra cost.
Have a family history of colon cancer.

If you’re uninsured or underinsured, you could be eligible for a free screening through the Division of Public Health’s Screening for Life program.
To learn more, visit HealthyDelaware.org/Colon or call 2-1-1.
53
Gauging and Responding to the Need for Home Repair Assistance in Delaware
Katharine Millard, M.S.P.P.M. Sussex County Habitat for Humanity
Stephen Metraux, Ph.D.
Joseph R. Biden, Jr. School of Public Policy & Administration, University of Delaware
ABSTRACT
We review the extent of the need for home repair assistance for low-income homeowners in Delaware, and steps being taken to address this need. Delaware contains an estimated 25,000 homes owned by low-income households that need repair, of which an estimated 5,000 are in substandard condition. There is an estimated $96 million total cost associated with this home repair need, with eighty percent of this cost ($76 million) coming from the twenty percent (5,000) of these homes that are in substandard condition. In order to address this need for repair assistance, Delaware’s three Habitat for Humanity organizations have designed the Statewide Healthy Homes Program, which centers on the intersection of health and housing. The vision of the Habitat for Humanity Statewide Healthy Homes Program is to increase capacity for home repair assistance across Delaware. Additionally, the program seeks to include partnerships with healthcare providers to ensure a holistic approach to home repairs, improving each resident’s quality of life.
INTRODUCTION
In December 2022, Delaware’s three Habitat for Humanity (HFH) organizations commissioned a group of researchers from the University of Delaware (UD) to assess the need for home repair assistance among low-income homeowner households.1 Homeownership becomes less common as household income drops, but low-income households that do own homes face heightened challenges with upkeep. Compared to their higher income counterparts, low-income homeowners typically face higher repair costs, and have less means to pay for these repairs.2 This creates conditions where, when needed repairs and maintenance are not made, physical and structural problems in the home accumulate to the point where the home is considered “substandard,” in that it “poses a risk to the health, safety or physical well-being of occupants, neighbors, or visitors.”3 Substandard housing, insofar as it leads to and exacerbates health problems, can incur health costs in addition to home repair costs, thereby impairing employment and ultimately increasing risk for mortgage default, foreclosure and abandonment.4,5
The problem of unmet home repair needs among low-income homeowners goes beyond individual households. Deteriorating housing systematically impacts health, on a population level, to where housing is considered to be a key social determinant of health.6,7 Deteriorating housing also negatively impacts the surrounding neighborhood, creating conditions associated with higher levels of crime and decreased levels of social connectivity.8 Finally, when housing for low-income households deteriorates to the point where dwellings become uninhabitable, it decreases the stock of affordable housing, which is already at critically low levels in Delaware and nationwide.9
In the next section of this article, we draw upon key findings from this needs assessment1 to provide an overview of home repair need among low-income homeowners in Delaware, and describe the subsequent efforts of Delaware’s HFH organizations to build upon this study and increase the statewide capacity for providing such repair assistance. In the last section, we then provide a roadmap for preserving existing affordable housing stock in Delaware, underscoring how home repairs represent a key component in Delaware’s efforts to address an affordable housing shortage that has taken on crisis proportions.9
REPAIR NEED AMONG HOMES OWNED BY LOW-INCOME HOUSEHOLDS IN DELAWARE
According to the best, most current data available, there are 74,410 housing units that are owned and occupied by low-income households. This housing is distributed across Delaware’s three counties in rough proportion to the distribution of owner-occupied housing more generally, and accounts for between 27 percent and 30 percent of each county’s total owner-occupied housing. “Low income” here means that household income is at or under 80 percent of the HUD area median family income (HAMFI). This income amount is substantially higher than what is typically considered “poor,” as 30% of HAMFI roughly corresponds to the federal poverty income guidelines. It does, however, include all poor homeowner households along with others who often earn too much to qualify for many assistance programs while they still have difficulty in paying their monthly expenses.10 Eighty percent of HAMFI is also the income limit under which households are eligible for the home repairs programs in two of the three Delaware Habitat for Humanity organizations.
54 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.011
Extent and Costs of Repair Need
Delaware contains an estimated 25,000 homes owned by lowincome households that need repair. This number reflects 33.6 percent of the estimated 74,410 units of homes owned by lowincome households in Delaware. The number of total homes comes from the US Department of Housing and Urban Affairs’ Comprehensive Housing Affordability Strategy (CHAS) data and the estimate of homes in need of repair is derived from more general estimates and other data specific to Delaware.1,2,10 The majority of the 25,000 homes in need of repairs would have repairs that would not render the housing substandard by most measures. Many of these needed repairs are non-urgent. There is much year-to-year turnover in the specific homes that comprise the repair need estimate, as homeowners manage to make repairs on many of these homes on their own. However, homes among these 25,000 represent the pool which would be eligible for home repair assistance programs.
An estimated 5,000 of these 25,000 homes owned by lowincome households are in substandard condition, based again upon applying more general estimates to Delaware specific data. Substandard, here loosely defined, means housing in need of either major or multiple repairs, or repairs that would cost upwards of $5,000. These repairs, if unaddressed, would present substantial health risks to the occupants, either imminently or over time. Such housing represents a relatively small proportion, 7 percent, of all low-income, owner-occupied homes in Delaware.
We estimate a $96 million total cost associated with the 25,000 homes in need of repair. About eighty percent of this estimated cost ($76 million) comes from the twenty percent (5,000) of these homes that are in substandard condition. In short, the repair needs of a minority of homes represent a disproportionate amount of the total repair costs. Targeting repairs for these “worst cases” would be more likely to preserve homes that would otherwise become permanently uninhabitable and mitigate those homes that present the greatest health risks. However, the higher repair costs presented by such worst-case homes would limit the number of homes that are able to be assisted.
In the UD needs assessment, the average repair cost for one of these substandard homes was estimated at $15,000, a value that is almost certainly conservative. Assigning a dollar value to the needed home repairs provides another means by which to demonstrate the magnitude of need for home repair assistance and to provide a comparison point for the funds actually allocated toward such assistance. There are no estimates for average repair costs for the 5,000 substandard units beyond that the minimum repair cost is $5,000 and, at most, the repair cost would not exceed the cost of replacement construction. Key informants assess amounts spent on repair assistance from Delaware organizations to typically range between $3,000 and $20,000 per home, providing a maximum cap that is more reflective of resource constraints than repair need.
These estimates, while conservative, plausible and empirically based, are more indicative of the scope of the aggregate repair need in Delaware than a precise number of homes in need of repair and corresponding costs. These estimates, as key informants pointed out, go far beyond the collective capacity of organizations currently providing home repair assistance in Delaware. Precise numbers are difficult to come by, but currently
a loose network of approximately eight organizations provide repair assistance to, as can be best assessed, less than 200 homes annually, compared to the thousands of homes in need of repair.
Key informants confirmed this assessment, reporting a lack of resources to meet demand for assistance (if they provide repairs directly) or facing challenges in helping households find such assistance. Waitlists and turning eligible households away were also mentioned. As a result there are often urgent situations where homes require extensive repairs that are left unaddressed and likely to deteriorate further.
Socio-Geographic Factors Related to Repair Need
No comprehensive inventory exists of where this repair need is located, but indications are that a variety of areas have concentrations of homes owned by low-income households and would benefit from home repair assistance. Each of Delaware’s three counties has different dynamics related to where its supply of low-income, owner-occupied housing is located. For example, while New Castle County has much larger numbers of older homes than Kent and Sussex counties, these two southern counties are more rural and have higher numbers of manufactured housing. The variation in these and other characteristics necessitate that different approaches toward addressing housing need be taken in each of the Counties.
The areas with the most acute need for home repair assistance are two inner-city Wilmington areas, each made up of four contiguous census tracts, that have the state’s highest concentrations of low-income, owner-occupied housing. These areas also showed high levels of older housing, poverty, and Black and Latino populations, all of which are factors correlated with the presence of substandard housing. These factors are interconnected. Age of a structure is one of the most direct indicators of its need for physical improvements and repairs.11 As homes age, they become more prone to depreciation in value as they physically deteriorate or are in locations that become less desirable. This is reflected in a process called “filtering,” in which once-higher priced homes over time become more available to lower-income households.12 In this way, the US housing market allows aging housing to be a primary means of creating lowincome housing.13
However, while this filtering of older housing makes them affordable to an expanded number of homebuyers, these lower income households may have less means and ability to properly maintain this housing at the same time that aging housing requires more upkeep.13 Low-income homeowners face housing problems at more than twice the rate of higherincome homeowners, while repairing their homes less often and spending less on repairs. While low-income homeowners can be resourceful in coming up with ways to make needed repairs, this also creates situations where housing problems are left unattended and housing conditions deteriorate.14–17
Wilmington also provides an example of how, in the wake of persistent and ongoing racial discrimination and segregation, “older, more crowded, and structurally inadequate” homes in economically depressed, inner-city areas tend to filter down disproportionately to Black and Latino households. This contributes to racially segregated neighborhoods that differ substantially on a variety of indicators from segregated, predominantly White neighborhoods. Segregated Black
55
neighborhoods are characterized by less adequate municipal services and amenities, which limits these neighborhoods’ ability to contact services that can deal with the problems of the built environment.18 Latino homeowners also face discrimination, higher costs and more difficulty related to securing credit, gain less equity in their homes, and other “challenges to healthy, sustained homeownership” comparable to White (non-Latino) homeowners, although Latinos face disparities that are less pronounced than are present in Black-White homeowner comparisons.19 Targeting home repair assistance to areas such as the two identified in Wilmington, with high numbers of lowincome Black and Latino homeowners, provides an opportunity to assist not only individual households but also, if the repair assistance is provided to sufficient scale, can have a positive impact on community-level conditions.
There is a second type of area in Delaware, present in all three counties, that appears to have high levels of home repair need by virtue of a presence of high numbers of low-income, owneroccupied homes. These areas also have large, and growing, non-White populations, but in contrast to the Wilmington neighborhoods just mentioned, these areas show indicators of economic stability. More specific socio-economic dynamics related to these characteristics are unclear, and call for further research. However, targeting home repair assistance to these areas could bolster this ongoing economic stability and help maintain minority homeownership.
A third type of area, again present in all three Delaware counties, that showed particular need for home repair assistance were rural in nature, but, while they were sparsely populated, they had high levels of low-income, owner-occupied housing. Concentrated areas of poverty and substandard housing are often hidden can be hidden and easily overseen in these areas. Older manufactured housing is at particular risk for taking on substandard conditions, and manufactured home parks with high rates of low-income households in rural, unincorporated areas are examples of smaller, hidden concentrations of substandard housing. The disproportionate demand for home repairs made by owners of manufactured homes was often mentioned by key informants, especially where the manufactured housing was of older stock and there was a question of whether replacement was more feasible than repair.
A final feature salient to home repair need among low-income households is that repair burden often falls upon elderly households. Homeownership can be an important source of financial security and housing stability among older adults. While only 3% of older adults live in structurally inadequate housing, keeping up with maintaining a home becomes increasingly more challenging as people age and confront physical and financial limitations, the latter of which includes living on fixed, retirement incomes.20 As maintenance efforts decline and homeowners age, the needs for modifications to the home increase if these homeowners are to maintain a healthy living environment. This included modifications that help elderly homeowners “age in place” in their homes despite disabilities and infirmities. Key informants stated that, in Delaware, a majority of home repair assistance went to elderly households. In New Castle County, for instance, an estimated 87% of repair services went to seniors. Elderly homeowners seem to be more integrated into the general population than other
targeted homeowner groups, as our data found no significant correlation between concentrations of elderly population and higher levels of low-income, owner-occupied housing.
Home Repair as Health Promotion
Home repair assistance not only helps keep housing affordable, it also can transform a house from merely a shelter to a space that supports a state of complete physical, mental, and social health and well-being.21 In recent years much attention has been paid to “healthy homes,” the idea that safe, decent, and sanitary housing is a means for preventing disease and injury, both on individual and population levels.22 The clear and intuitive messages that improved housing quality also improves health, while substandard housing causes or contributes to negative health outcomes, have become focal points for efforts to expand the provision of home repair assistance in Delaware. This has led to healthcare systems engaging with repair organizations, with the object of improving the housing quality to which recovering patients can return and continue recovery, thereby reducing rehospitalizations and improving patients’ health and well-being. Tying together home repair assistance and health care links lets organizations bundle home repair assistance with other types of assistance, and care can increase the effectiveness of home repair assistance as it targets high priority populations such as elderly homeowner households.
MOVING AHEAD: EXPANDING HOME REPAIR ASSISTANCE IN DELAWARE
Home repair is not an unknown or unfamiliar issue in the State of Delaware. Prior needs assessments have focused solely on housing condition with little thought to how housing relates to other aspects of life. In this manner, home repair assistance has focused on physical issues instead of the home’s condition in relation to quality of life as a whole. This way of thinking is changing. The Centers for Disease Control and Prevention now recognizes housing as a social determinant of health.23,24 A home is no longer just a place where you rest your head at night, but the foundation to a healthy, prosperous and happy life.
Trying to bridge the gap between home and health, Habitat for Humanity of New Castle County, Central Delaware Habitat for Humanity, and Sussex County Habitat for Humanity commissioned the recent University of Delaware home repair needs study1 to help design a statewide home repair program that centers on the intersection of health and housing. Originally armed with anecdotal information, the three Habitat affiliates began to conceptualize a Statewide Healthy Homes Program in 2020. Each affiliate has decades of experience in the community, and consistently sees the immense needs of low-income homeowners. The COVID-19 pandemic exacerbated these needs, increasing the number of inquiries for each affiliate’s home repair program, straining already insufficient resources. The first step in creating a healthy homes program was to better understand what was seen on the ground and put a number to the amount of assistance needed by low-income homeowners in Delaware, specifically by county.
The results of this study exceeded even what housing providers knew: the need for home repairs far outpaces the current capacity to complete repairs - specifically for low- and moderate income households. Limited resources, including funding and providers, restricts repairs for low-income homeowners to less
56 Delaware Journal of Public Health - June 2023
than 1,000 per year, nowhere near the approximately 25,000 total affected homes. The vision of the Habitat for Humanity Statewide Healthy Homes Program is to increase capacity to complete more home repairs across Delaware and supplement the repair programs already in place. Additionally, the program will include partnerships with healthcare providers to ensure a holistic approach to home repairs, improving each resident’s quality of life. The statewide approach is also expected to bring additional funding for home repairs from local, state, federal, and national resources. The program, while statewide, will be administered in each county to ensure the different needs across the state are understood, and met.
Targeting health outcomes will inherently change the way home repairs are conducted –including assessments and scope of work creation. Initial assessments will focus on the safety, energy efficiency, and accessibility of each home, and how these conditions affect the health of the residents. Expected repairs include, but are not limited to, repairing or replacing doors, windows, roofs, flooring, sheetrock, electrical and plumbing systems, and more; installing accessibility improvements such as wheelchair ramps, tub cuts, and lighting improvements; and referrals to ensure mold remediation, lead abatement, and other important health issues are remedied appropriately.
Even with program expansion, this issue is much larger than one program alone. Many organizations are starting to realize the benefits of prioritizing health outcomes in home repair programs. Energize Delaware recently launched a pilot program, the Energy Resilient and Healthy Homes Grant, that is expected to launch in each county in Summer 2023. The innovative nature of this program includes a partnership between a healthcare institution and a housing provider to create the repair scope of work. The emerging Statewide Healthy Homes Program also aims to supplement existing statewide repair programs such as the Statewide Emergency Repair Program (SERP), Weatherization Program, Pre-Weatherization Program, Septic System Replacement Program, Water, Waste Water and Structural Repairs, and home repair programs administered by New Castle County, Kent County, and Sussex County, among many others. SERP, administered by Milford Housing Development Corporation, is an important service that addresses immediate needs such as heating and cooling and other important repairs that are emergent in nature. The Statewide Weatherization and Pre-Weatherization Programs are offered statewide, and help homeowners weatherize their homes to ensure a comfortable and stable indoor temperature. Stabilizing indoor temperatures may help alleviate cardiac conditions, asthma, and other respiratory disease as well as reduce the incidence of mold in homes with air and water infiltration.
Outside of nonprofit entities and local and county jurisdictions, there is limited attention to home repair needs. Ultimately, more must be done. All Delawareans should advocate for additional funding for healthy housing, including increases in state and federal dollars aimed at funding home repair programs. Hospital and healthcare organizations and home repair organizations should partner more frequently to ensure these programs functionally rely on health outcomes for every project completed. And finally, this study can act as a blueprint for future program development across the state. Understanding the need is the first step. Creating an action plan to address this need is now the next. Ms. Millard may be contacted at katie@sussexcountyhabitat.org.
REFERENCES
1. Metraux, S., Hesketh, R., O’Neill, S., Rayl, M., & Modeas, A. C. (2022). A needs assessment for repairs to low-income owneroccupied housing in Delaware. The Tri-County Habitat for Humanity Organizations in Delaware. Retrieved from: https://www.sussexcountyhabitat.org/wp-content/uploads/2022/12/ FINAL-H4H-healthy-housing-needs-assessment.pdf
2. Divringi, E., Wallace, E., Wardrip, K., & Nash, E. (2019). Measuring and understanding home repair costs: A national typology of households. Federal Reserve Bank of Philadelphia and Policy Map. Retrieved from: https://www.philadelphiafed.org/community-development/housingand-neighborhoods/measuring-and-understanding-home-repair-costs
3. Thompson, V. (2018) What is substandard housing? Home Guides: SFGATE/San Francisco Chronicle. Retrieved from: https://homeguides.sfgate.com/substandard-housing-55618.html
4. Cutshaw, C. A., Woolhandler, S., Himmelstein, D. U., & Robertson, C. (2016). Medical causes and consequences of home foreclosures. International Journal of Health Services, Planning. Int J Health Serv, 46(1), 36–47.
https://doi.org/10.1177/0020731415614249
5. Houle, J. N., & Keene, D. E. (2015, April). Getting sick and falling behind: Health and the risk of mortgage default and home foreclosure. Journal of Epidemiology and Community Health, 69(4), 382–387.
https://doi.org/10.1136/jech-2014-204637
6. Shaw, M. (2004). Housing and public health. Annual Review of Public Health, 25(1), 397–418.
https://doi.org/10.1146/annurev.publhealth.25.101802.123036
7 Krieger, J., & Higgins, D. L. (2002, May). Housing and health: Time again for public health action. American Journal of Public Health, 92(5), 758–768.
https://doi.org/10.2105/AJPH.92.5.758
8. South, E. C., MacDonald, J., & Reina, V. (2021, July 1). Association between structural housing repairs for lowincome homeowners and neighborhood crime. JAMA Network Open, 4(7), e2117067.
https://doi.org/10.1001/jamanetworkopen.2021.17067
9. Housing Alliance Delaware. (2022). Housing and homelessness in Delaware: Crisis to Recovery. Retrieved from:
https://www.housingalliancede.org/housing-alliance-publications
10. United Way of Delaware. (2021). ALICE in Delaware: A financial hardship study. Retrieved from:
https://www.unitedforalice.org/state-overview/delaware
11. Kutty, N. (1999). Determinants of structural adequacy of dwellings. Journal of Housing Research, 10(1), 27–43.
https://doi.org/10.1080/10835547.1999.12091943
12. Bier, T. (2001). Moving up, filtering down: Metropolitan housing dynamics and public policy. Brookings Institution, Center on Urban and Metropolitan Policy. Retrieved from:
https://www.brookings.edu/wp-content/uploads/2016/06/bier.pdf
13. Liu, L., McManus, D., & Yannopoulos, E. (2022). Geographic and temporal variation in housing filtering rates. Regional Science and Urban Economics, 93, 103758.
https://doi.org/10.1016/j.regsciurbeco.2021.103758
57
14. Louie, J., Belsky, E. S., & McArdle, N. (1998). The housing needs of low-income homeowners. Joint Center for Housing Studies, Harvard University. Retrieved from: https://www.jchs.harvard.edu/research-areas/working-papers/housingneeds-lower-income-homeowners
15. Van Zandt, S., & Rohe, W. M. (2011). The sustainability of low-income homeownership: The incidence of unexpected costs and needed repairs among low-income home buyers. Housing Policy Debate, 21(2), 317–341.
https://doi.org/10.1080/10511482.2011.576525
16. Acquaye, L. (2011). Low-income homeowners and the challenges of home maintenance. Community Development (Columbus, Ohio), 42(1), 16–33.
https://doi.org/10.1080/15575330.2010.491154
17. Joint Center for Housing Studies. (2021). Improving America’s housing: 2021. Harvard University. Retrieved from: www.jchs.harvard.edu/improving-americas-housing-2021
18. Williams, D. R., & Collins, C. (2001, Sep-Oct). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep, 116(5), 404–416.
https://doi.org/10.1016/S0033-3549(04)50068-7
19. Kuebler, M. (2013). Closing the wealth gap: A review of racial and ethnic inequalities in homeownership. Sociology Compass, (8): 670–685.
https://doi.org/10.1111/soc4.12056
20. Molinsky, J., & Herbert, C. (2020). Homeownership among older adults: Source of stability or stress? Innovation in Aging, 4(Suppl 1), 691.
https://doi.org/10.1093/geroni/igaa057.2417
21. World Health Organization. (2018). WHO housing and health guidelines. World Health Organization. Retrieved from: https://www.who.int/publications/i/item/9789241550376
22. U.S. Department of Housing and Urban Development. (n.d.). Making homes healthier for families. Retrieved from: https://www.hud.gov/program_offices/healthy_homes/healthyhomes
23. Lipshutz, J. A., Hall, J. E., Penman-Aguilar, A., Skillen, E., Naoom, S., & Irune, I. (2022, March-April 01). Leveraging social and structural determinants of health at the Centers for Disease Control and Prevention: A systems-level opportunity to improve public health. J Public Health Manag Pract, 28(2), E380–E389.
https://doi.org/10.1097/PHH.0000000000001363
24. Habitat for Humanity. (2021). How does housing impact health? Habitat for Humanity International. Retrieved from: https://www.habitat.org/media/7071/view
Even the best rider is at the mercy of other drivers. If you go too fast, they may cut you off, change lanes, or make turns before they see you coming.
SO WATCH YOUR SPEED, WATCH OUT FOR OTHER DRIVERS, AND STAY SOBER.

ArriveAliveDE.com/Respect-The-Ride Life'stooshorttogo too fast 58 Delaware Journal of Public Health - June 2023
Detect it early.
A lung cancer screening detected my cancer early, when it was most treatable. It could do the same for you.
Talk with your health care provider to schedule a lung cancer screening today. If you don’t have one, a nurse navigator can help — whether you have insurance or not.
You’re eligible for a lung cancer screening if you:
• Are between age 50 and 80; and

• Smoked a pack a day for 20+ years in the last 15 years; or
• Smoked two packs a day for 10+ years in the last 15 years.
Call 2-1-1 or scan the QR code to visit HealthyDelaware.org/Lung.

59
The Perilous Intersection of Housing Precarity and Climate Change in Delaware
Victor W. Perez, Ph.D.
Department of Sociology and Criminal Justice, University of Delaware
William Swiatek, M.A., A.I.C.P.
Wilmington Area Planning Council
One particularly hazardous form of housing precarity is homelessness. The State of Delaware has seen an upward trend in homelessness since 2019, increasing from a point-in-time count of 921 that year to 2,369 in the year 2022.1 In 2022, 43% of the homeless were in New Castle County, followed by 34% in Sussex County, and 23% in Kent County.1 The total county population breakdown in Delaware is 58% in New Castle County, 24% in Sussex, and 18% in Kent, reflecting a slightly higher skew in homelessness in the southern counties.2 The vast majority (93%) of homeless live in emergency shelters in Delaware, while 7% are unsheltered.1
Though official counts of death among the homeless are not done by the federal government and estimates are based on regional and other assessments that can vary widely, the homeless experience increased risk of mortality and various types of morbidity compared to the general population, including higher rates of diabetes and cardiovascular disease, while also suffering from the co-existence of psychological disorders, substance use, and infectious diseases at rates higher than the general population.3,4
In the coming decades across the state of Delaware, scientific forecasts suggest a variety of continued climate change consequences, such as additional sea level rise and stronger storm surges. Another notable climate change outcome is rising temperature. In Delaware, “average temperatures…are projected to be 3.5 to 8 degrees F warmer by 2100 compared to the same base period of 1981 to 2010. In addition to average temperatures rising, extreme temperature events are also projected to become more frequent.”5 This change in temperature has the potential to worsen the existing urban heat island effect in places like Wilmington, Dover, Newark, and other heavily developed areas lacking green space. Heat islands are urban areas characterized as “highly efficient at absorbing and storing heat from the sun, a lack of vegetation limiting the cooling effect of evaporation from the soil and plant transpiration (evapotranspiration), and trapping of heat released by human activities (e.g., transport, lighting, air conditioning).”6
When urban homelessness and climate change outcomes converge, the potential for deadlier weather to create and exacerbate long- and short-term health conditions that disproportionately affect the homeless comes into clear and calamitous view. Urban heat islands are associated with a variety of negative health outcomes, including heat-related illnesses like exhaustion and heat stroke,7 worsening asthma due to poorer air quality,8 and increased risk of hospitalization or death.9 Moreover, the unsheltered and those utilizing emergency and temporary shelters can be disproportionately affected by more frequent and intense storms and storm surges.10 The need to examine these specific issues in Delaware is paramount.
Projects that redevelop existing urban landscapes offer generational opportunities to both adapt to global warming and lessen our carbon footprint. Examples include housing, commercial, park and open space, and transportation system redevelopment projects that mitigate urban heat and flooding impacts. Such efforts not only make cities more livable for current and future residents, but they combat unsustainable suburban sprawl by supporting a more concentrated infill land development. These efforts, illustrations of which are provided below, both directly and indirectly alleviate climate change burdens (such as rising temperatures and increased flooding) that can disproportionately impact homeless residents.
The transportation sector, the largest contributor to Delaware’s greenhouse gas emissions, is an instructive example. While the decarbonization of our vehicle fleets and selecting more heat and flood-resistant pavements are important steps to reduce emissions and adapt to warming, so too, simply, is street design. City streets account for more than a quarter of land used in North American cities.11 During the past century, Delaware’s streets were largely designed to prioritize fast and efficient vehicular movements. This has led, however, to the proliferation of impervious surfaces that exacerbate heat and flooding concerns and a worsening public health crisis in road safety. A more nuanced approach to street design exchanges some existing pavement for green landscaping, community art, and bicycle lanes. These more “complete streets” also result in reduced vehicle travel speeds, reducing the number and severity of crashes.12
Along the Route 9 corridor, between Wilmington and the City of New Castle, a pair of projects are taking this approach. The Route 9 Master Plan, adopted by the Wilmington Area Planning Council (WILMAPCO) in 2017, calls for the strategic removals of travel lanes in favor of more green space and separated, safer, pathways for people to walk and bike.13 Another WILMAPCO-led effort, the Southbridge Transportation Action Plan, is currently examining the extension of Route 9’s planned “road diet” northwards into the City of Wilmington through traffic modeling and community engagement.14
While the state department of transportation is very supportive of both efforts, and recently received a $6 million federal grant to kickstart additional outreach and design work to realize the Route 9 project, it currently does not have the policy, funding, or staff to support the maintenance of the planned intensive landscaping. A local body, such as a municipal government or community group, must agree to do so before the first tree is planted along the state’s right-of-way. While a pair of small community development corporations along the Route 9 corridor are examining the feasibility of their entering into such an agreement, reversing this policy to
60 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.012
allow for state maintenance of more intensive landscaping may help Delaware maximize the greening potential of its streets and highways.
Two other major transportation projects in the City of Wilmington are also examples of urban greening and climate resilience. The I-95 Cap project aims to construct a new park on top of I-95 between 6th Street and Delaware Avenue, reconnecting neighborhoods split by the interstate’s construction in the 1960s. The project would cover the sunken highway with a public green, community amphitheater, gardens, pathways, a dog park, and 500 trees -- increasing area softscape by a dozen acres. The 12th Street Connector, meanwhile, would build a new roadway connection between Northeast Boulevard and 16th Street, facilitating both infill redevelopment, new park space, and better shoreline protection along the Brandywine River. Both projects15,16 are currently unfunded. If they proceed, while their climate benefits are clear, care must also be given to ensure they do not inadvertently result in green gentrification, or the eventual displacement of current residents when the value of real estate, rents, and other costs of living increase because of the renewed environmental conditions in the area.17
As a coastal state with several urban centers connected by commercial corridors and flanked by sprawling suburbs, the state of Delaware is and will continue to experience many of the most notable, devastating climate change impacts. These repercussions will affect different areas, infrastructure, and social groups in both general and more acute ways, as will negative health consequences depending on race, age, veteran status, and other significant socio-demographic characteristics of the homeless. Throughout the region and the state, we need to bolster a commitment to the well-being of the housing precarious and help protect them from climate change consequences and the worsening health outcomes associated with them. We are hopeful that the policy and land use recommendations provided in this commentary will ameliorate negative health impacts of climate change on the homeless throughout the state.
Dr. Perez may be contacted at victorp@udel.edu
REFERENCES
1. Housing Alliance Delaware. (2022). Point in time count & housing inventory count 2022 report. Retrieved from: https://www.housingalliancede.org/coc-reports
2. United States Census Bureau. (2022). B01001 Sex by age. 2021 American Community Survey 5-Year Estimates. U.S. Census Bureau, American Community Survey Office. http://www.census.gov/
3. McCormick, E. (2022, Feb). Homelessness is lethal: US deaths among those without housing are surging. The Guardian. Retrieved from https://www.theguardian.com/us-news/2022/feb/07/homelessnessis-lethal-deaths-have-risen-dramatically
4. Fazel, S., Geddes, J. R., & Kushel, M. (2014, October 25). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet, 384(9953), 1529–1540. https://doi.org/10.1016/S0140-6736(14)61132-6
5. Delaware Department of Natural Resources and Environmental Control. (2021). Delaware’s Climate Action Plan. Retrieved from https://documents.dnrec.delaware.gov/energy/Documents/Climate/ Plan/Delaware-Climate-Action-Plan-2021.pdf
6. Tong, S., Prior, J., McGregor, G., Shi, X., & Kinney, P. (2021, October 25). Urban heat: An increasing threat to global health. BMJ (Clinical Research Ed.), 375(2467), n2467. https://doi.org/10.1136/bmj.n2467
7. Environmental Protection Agency. (2022). Climate change indicators: Heat-related illnesses. Retrieved from https://www.epa.gov/climate-indicators/heat-related-illnesses
8. ClimateXChange. (2021). Heat waves, urban heat islands, and the inequitable impacts of a warming climate. Retrieved from https://climate-xchange.org/2021/08/06/heat-waves-urban-heatislands-and-the-inequitable-impacts-of-a-warming-climate/
9. Heaviside, C. (2020). Urban heat islands and their associated impacts on health. Oxford Research Encyclopedia of Environmental Science. https://doi.org/10.1093/acrefore/9780199389414.013.332
10. The Climate Reality Project. (2019). Homelessness and the climate crisis. Retrieved from https://www.climaterealityproject.org/blog/homelessness-andclimate-crisis
11. United Nations Human Settlements Programme. (2013). Streets as public spaces and drivers of urban prosperity. Retrieved from https://unhabitat.org/sites/default/files/2020/08/streets_as_public_ spaces_and_drivers_of_urban_prosperity.pdf
12. Fields, B, & Renne, J. L. (2021). Adaptation urbanism and resilient communities: Transforming streets to address climate change. Routledge: New York.
13. WILMAPCO. (2017). The Route 9 Master Plan http://www.wilmapco.org/route9/
14. WILMAPCO. [forthcoming]. Southbridge Transportation Action Plan. http://www.wilmapco.org/southbridge/
15. WILMAPCO. (n.d.). Bridging I-95: Reconnecting the community. I-95 cap feasibility study. Retrieved from http://www.wilmapco.org/i95cap/
16. WILMAPCO. (n.d.). 12th Street connector transportation improvement study. Retrieved from: http://www.wilmapco.org/12thstreetconnector/
17. Perez, V W., &Swiatek, W. (2022, August31). Greening, revitalization, and health in South Wilmington, DE. Delaware Journal of Public Health, 8(3), 78–84. https://doi.org/10.32481/djph.2022.08.013
61
Caring for kids (and their moms) in Suriname…p. 5
Caring for kids (and their moms)
Caring for kids (and their moms) in Suriname…p. 5
in Suriname…p. 5
New study finds dementia in India underestimated
dementiainIndia
New study finds dementia in India underestimated
By Susan Scutti
New study finds dementia in India underestimated
New study finds dementia in India underestimated
By Susan Scutti
By Susan Scutti
By 2050, over 75% of cases of Alzheimer’s disease and related dementias (ADRD) are expected to occur in low- and middle-income countries. Yet, most of the current knowledge of ADRD is based on findings from high-income countries. This fact prompted economics professor Jinkook Lee and her colleagues to design a study, funded in part by the National Institute on Aging, to estimate dementia prevalence in India, home to 18% of the world’s population. “In India, prior estimates were based on samples from selected communities and so inadequately represented the population,” noted the director of the Program on Global Aging, Health, and Policy at the University of Southern California’s Center for Economic and Social Research.
By 2050, over 75% of cases of Alzheimer’s disease and related dementias (ADRD) are expected to occur in low- and middle-income countries. Yet, most of the current knowledge of ADRD is based on findings from high-income countries. This fact prompted economics professor Jinkook Lee and her colleagues to design a study, funded in part by the National Institute on Aging, to estimate dementia prevalence in India, home to 18% of the world’s population. “In India, prior estimates were based on samples from selected communities and so inadequately represented the population,” noted the director of the Program on Global Aging, Health, and Policy at the University of Southern California’s Center for Economic and Social Research.
By Susan Scutti
By 2050, over 75% of cases of Alzheimer’s disease and related dementias (ADRD) are expected to occur in low- and middle-income countries. Yet, most of the current knowledge of ADRD is based on findings from high-income countries. This fact prompted economics professor Jinkook Lee and her colleagues to design a study, funded in part by the National Institute on Aging, to estimate dementia prevalence in India, home to 18% of the world’s population. “In India, prior estimates were based on samples from selected communities and so inadequately represented the population,” noted the director of the Program on Global Aging, Health, and Policy at the University of Southern California’s Center for Economic and Social Research.
By 2050, over 75% of cases of Alzheimer’s disease and related dementias (ADRD) are expected to occur in low- and middle-income countries. Yet, most of the current knowledge of ADRD is based on findings from high-income countries. This fact prompted economics professor Jinkook Lee and her colleagues to design a study, funded in part by the National Institute on Aging, to estimate dementia prevalence in India, home to 18% of the world’s population. “In India, prior estimates were based on samples from selected communities and so inadequately represented the population,” noted the director of the Program on Global Aging, Health, and Policy at the University of Southern California’s Center for Economic and Social Research.
To begin, Lee and her colleagues recruited more than 4,000 seniors (ages 60 and older) from the Longitudinal Aging Study in India (LASI), the largest national health and retirement study in the world. Participants were interviewed and underwent a series of neuropsychological tests. Next, a panel of experts rendered a collective diagnosis for a subsample of participants. Then Lee and her colleagues constructed a logistic regression model, a type of statistical model frequently used to predict outcomes, to deduce the dementia status for all other LASI seniors, a total of 28,949 people.
To begin, Lee and her colleagues recruited more than 4,000 seniors (ages 60 and older) from the Longitudinal Aging Study in India (LASI), the largest national health and retirement study in the world. Participants were interviewed and underwent a series of neuropsychological tests. Next, a panel of experts rendered a collective diagnosis for a subsample of participants. Then Lee and her colleagues constructed a logistic regression model, a type of statistical model frequently used to predict outcomes, to deduce the dementia status for all other LASI seniors, a total of 28,949 people.
To begin, Lee and her colleagues recruited more than 4,000 seniors (ages 60 and older) from the Longitudinal Aging Study in India (LASI), the largest national health and retirement study in the world. Participants were interviewed and underwent a series of neuropsychological tests. Next, a panel of experts rendered a collective diagnosis for a subsample of participants. Then Lee and her colleagues constructed a logistic regression model, a type of statistical model frequently used to predict outcomes, to deduce the dementia status for all other LASI seniors, a total of 28,949 people.
To begin, Lee and her colleagues recruited more than 4,000 seniors (ages 60 and older) from the Longitudinal Aging Study in India (LASI), the largest national health and retirement study in the world. Participants were interviewed and underwent a series of neuropsychological tests. Next, a panel of experts rendered a collective diagnosis for a subsample of participants. Then Lee and her colleagues constructed a logistic regression model, a type of statistical model frequently used to predict outcomes, to deduce the dementia status for all other LASI seniors, a total of 28,949 people.
Lee’s team gauged that dementia prevalence in India is 7.4% among adults over the age of 60—meaning about 8.8 million Indians are currently living with dementia. “This is greater than the Dementia in India 2020 Report estimate of 5.3 million,” Lee told Fogarty in an email, and is closer to dementia rates in both the U.S. (8.6%) and the U.K. (7.1%). The team also saw significant cross-state variation.
Lee’s team gauged that dementia prevalence in India is 7.4% among adults over the age of 60—meaning about 8.8 million Indians are currently living with dementia. “This is greater than the Dementia in India 2020 Report estimate of 5.3 million,” Lee told Fogarty in an email, and is closer to dementia rates in both the U.S. (8.6%) and the U.K. (7.1%). The team also saw significant cross-state variation.
Lee’s team gauged that dementia prevalence in India is 7.4% among adults over the age of 60—meaning about 8.8 million Indians are currently living with dementia. “This is greater than the Dementia in India 2020 Report estimate of 5.3 million,” Lee told Fogarty in an email, and is closer to dementia rates in both the U.S. (8.6%) and the U.K. (7.1%). The team also saw significant cross-state variation.
Lee’s team gauged that dementia prevalence in India is 7.4% among adults over the age of 60—meaning about 8.8 million Indians are currently living with dementia. “This is greater than the Dementia in India 2020 Report estimate of 5.3 million,” Lee told Fogarty in an email, and is closer to dementia rates in both the U.S. (8.6%) and the U.K. (7.1%). The team also saw significant cross-state variation.
“Our findings provide critical new information for the estimation of the global prevalence of dementia,” said Lee. The new survey corresponds to “other health and
“Our findings provide critical new information for the estimation of the global prevalence of dementia,” said Lee. The new survey corresponds to “other health and
“Our findings provide critical new information for the estimation of the global prevalence of dementia,” said Lee. The new survey corresponds to “other health and
“Our findings provide critical new information for the estimation of the global prevalence of dementia,” said Lee. The new survey corresponds to “other health and




•A
•
•
While 7.4% is the estimated dementia prevalence rate for adults aged 60 and older in India as a whole, this map shows it is unevenly distributed across Indian states.
While 7.4% is the estimated dementia prevalence rate for adults aged 60 and older in India as a whole, this map shows it is unevenly distributed across Indian states.
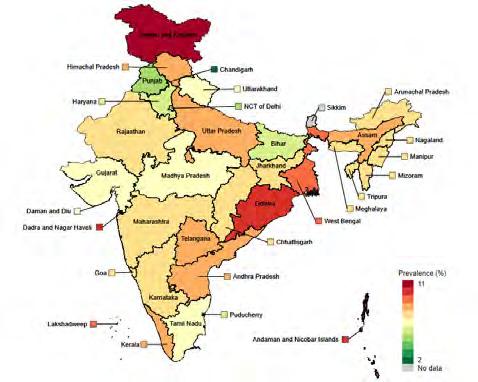
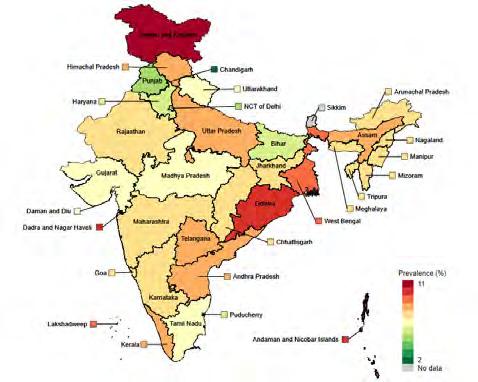
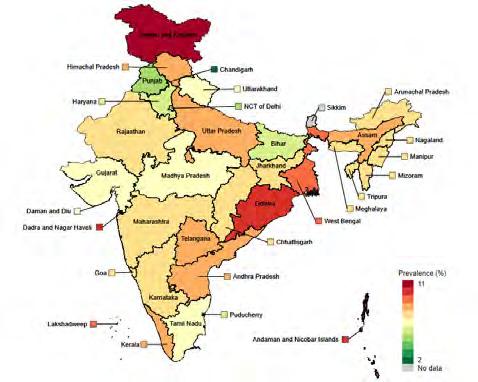
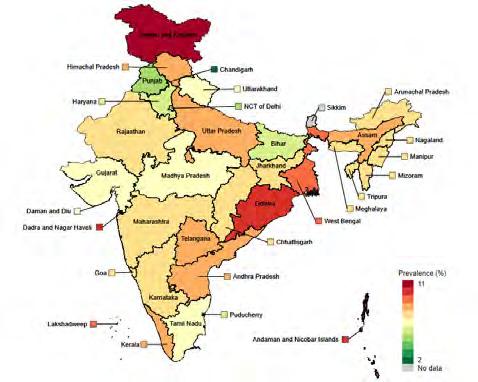
retirement studies around the world, enabling cross-country comparisons,” she added. “Further, there are several research teams in other low- and middle-income countries like Kenya, Nepal, and Pakistan, following our research protocol in establishing a study cohort and conducting community-based interviews.”
retirement studies around the world, enabling cross-country comparisons,” she added. “Further, there are several research teams in other low- and middle-income countries like Kenya, Nepal, and Pakistan, following our research protocol in establishing a study cohort and conducting community-based interviews.”
retirement studies around the world, enabling cross-country comparisons,” she added. “Further, there are several research teams in other low- and middle-income countries like Kenya, Nepal, and Pakistan, following our research protocol in establishing a study cohort and conducting community-based interviews.”
retirement studies around the world, enabling cross-country comparisons,” she added. “Further, there are several research teams in other low- and middle-income countries like Kenya, Nepal, and Pakistan, following our research protocol in establishing a study cohort and conducting community-based interviews.”




By 2050, India’s share of seniors is projected to increase to nearly 20% of its population—319 million individuals, according to Lee and her co-authors. With age the strongest risk factor for ADRD, India faces an alarming potential increase in the number of people with dementia. An accurate estimate of dementia prevalence is essential to comprehend the magnitude of the challenge the country is facing, she said.
By 2050, India’s share of seniors is projected to increase to nearly 20% of its population—319 million individuals, according to Lee and her co-authors. With age the strongest risk factor for ADRD, India faces an alarming potential increase in the number of people with dementia. An accurate estimate of dementia prevalence is essential to comprehend the magnitude of the challenge the country is facing, she said.
By 2050, India’s share of seniors is projected to increase to nearly 20% of its population—319 million individuals, according to Lee and her co-authors. With age the strongest risk factor for ADRD, India faces an alarming potential increase in the number of people with dementia. An accurate estimate of dementia prevalence is essential to comprehend the magnitude of the challenge the country is facing, she said.
By 2050, India’s share of seniors is projected to increase to nearly 20% of its population—319 million individuals, according to Lee and her co-authors. With age the strongest risk factor for ADRD, India faces an alarming potential increase in the number of people with dementia. An accurate estimate of dementia prevalence is essential to comprehend the magnitude of the challenge the country is facing, she said.
Conducting research beyond national borders is also crucial. “A global perspective enables us to think through which aspects of aging are universal and which are not.”
Conducting research beyond national borders is also crucial. “A global perspective enables us to think through which aspects of aging are universal and which are not.”
Conducting research beyond national borders is also crucial. “A global perspective enables us to think through which aspects of aging are universal and which are not.”
Conducting research beyond national borders is also crucial. “A global perspective enables us to think through which aspects of aging are universal and which are not.”
Read more on pages 6 – 9
Read more on pages 6 – 9
62 Delaware Journal of Public Health - June 2023 www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue GLOBAL
FOCUS MAR/APR 2023 Global Health Fellows & Scholars at 20 •A look back •One program, global impact •A for mer Fellow’s perspective Read more on pages 6 – 9 Caring for kids (and their moms) in Suriname…p. 5
HEALTH MATTERS
Image courtesy of Jinkook Lee
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue GLOBAL HEALTH
FOCUS MAR/APR 2023 Global Health Fellows & Scholars at 20
A look back
One program, global impact
former Fellow’s perspective
MATTERS
•
•
•A
While 7.4% is the estimated dementia prevalence rate for adults aged 60 and older in India as a whole, this map shows it is unevenly distributed across Indian states. Image courtesy of Jinkook Lee
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue GLOBAL HEALTH MATTERS FOCUS MAR/APR 2023 Global Health Fellows & Scholars at 20 • A look back • One program, global impact • A former Fellow’s perspective
more on pages 6 – 9
Read
Image courtesy of Jinkook Lee
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue GLOBAL HEALTH MATTERS FOCUS MAR/APR 2023 Global Health Fellows & Scholars at 20
look back
One program, global impact
A for mer Fellow’s perspective
While 7.4% is the estimated dementia prevalence rate for adults aged 60 and older in India as a whole, this map shows it is unevenly distributed across Indian states.
Image courtesy of Jinkook Lee
66
More on pages 67-69 INSTITUTESOF • A • A former
Read
Researchers probe HIV-associated stroke
By Susan Scutti
Sub-Saharan Africa shoulders the greatest burden of stroke, which is the leading cause of disability worldwide and the second leading cause of death. The region’s high incidence of stroke is at least partially linked to the twothirds of the world’s population with HIV residing there. Compared to uninfected individuals, people with HIV (PWH) have more than double the risk of stroke.
A team led by Dr. Deanna Saylor at University Teaching Hospital (UTH) in Lusaka, Zambia, are exploring the entwined issues of stroke and HIV. Because the mechanisms leading to excess stroke risk among PWH are poorly understood, the best ways to prevent stroke among these patients have not yet been established. Yet it is data from HIV-uninfected populations that guides primary stroke prevention, acute treatment, and secondary stroke prevention in people with HIV, even though “stroke is very different in people with HIV,” said Saylor.

Features of HIV-associated stroke
“In Zambia, the HIV rate is around 12%, which is pretty high, so we tend to see a lot of patients with HIV presenting with stroke,” said Dr. Stanley Zimba, lead author of a 2021 study, “Risk factors and outcomes of HIV-associated stroke in Zambia.” The study (coauthored by Saylor) retrospectively reviewed charts of all adults admitted to UTH with a diagnosis of stroke between October 2018 and March 2019. The researchers, who wanted “to get a better understanding and to generate data that would be helpful in terms of managing patients,” discovered that participants with HIV were younger than uninfected participants, said Zimba. PWH also tended to lack traditional stroke risk factors, such as hypertension and diabetes; a full third of PWH participants had no other identified risk factor than HIV. Another finding: Deep vein thrombosis was more common during hospitalization amongst PWH though no in-hospital mortality differences were seen when compared to HIV-negative patients.
These findings will help the team develop new strategies for preventing stroke in people with HIV, said Zimba. “Early antiplatelet therapy or use of other medications like statins might be needed to lower stroke risk in this population.” Additional factors that complicate prevention and rehabilitation, including whether
patients are taking antiretroviral therapy (ART), how long they have been on ART, and the presence of opportunistic infections, will also need to be considered.
Overall, Zimba is confident his work will benefit not only Zambia but the globe. “Stroke risk factors, primary prevention, treatment, and rehabilitation in PWH are all very important and cut across various clinical practices— yet none of these features are governed by borders. Stroke can occur anywhere in the world where there is a patient with HIV,” he said.
Exploring possible mechanisms
Saylor’s Fogarty-funded project, Adaptation and Implementation of Clinical Practice Guidelines to Improve Stroke Outcomes in Zambia, seeks to generate new knowledge and help develop new care systems for stroke in Zambia. “Our main focus is to use an evidencebased approach to implementation science in order to adapt stroke guidelines from high-resourced settings to Zambia and to develop a stroke treatment protocol that is applicable in low-resource settings and improves patient outcomes,” Saylor told Fogarty in an email.
While stroke looks different in PWH, “whether the strokes themselves are different is a bit less clear,” said Saylor. Some initial studies suggested HIV-associated strokes were more likely to be large vessel strokes—where blood blockage occurs in one of the main arteries—with poorer outcomes. Yet participants in these studies often had poorly controlled HIV (as it was early in the epidemic), and opportunistic infections had caused their strokes. In contemporary studies, most HIV-associated stroke is unrelated to opportunistic infections, Saylor said.
Yet stroke occurring at younger ages in PWH who lack traditional risk factors still suggests “alternative mechanistic pathways for HIV-associated stroke,” she said.
63 MARCH/APRIL 2023 2
Dr. Deanna Saylor (left) teaches a group of trainee doctors while visiting a patient at University Teaching Hospital in Lusaka, Zambia. Her project seeks to develop new care systems for stroke in Zambia.
Photo courtesy of Deanna Saylor
Benchmarking data science in Africa
Last December, Fogarty brought together African researchers in the fields of data science, bioinformatics, epidemiology, ethics, and biostatistics for a writers’ retreat as part of the development of a collection of scientific papers to be published in the Nature portfolio of journals. The State of Data Science for Health in Africa Writing Project was inspired by the Harnessing Data Science for Health Discovery and Innovation in Africa (DS-I Africa) initiative, a NIH Common Fund program that aims to facilitate the development of a trans-African network of data scientists and increase capacity for data science research in Africa.

The goals of the collection are to provide a benchmark for the state of the field that can be used by data science and health communities to assess progress over the next several years. Importantly, the project is led by African experts and nearly all the authors involved in the project are African. Africa is “poised for a data science revolution,” said Dr. Emile Rugamika Chimusa, Professor of Bioinformatics at Northumbria University and one of the project co-chairs. “We need more data scientists, and we need to benchmark where data science is currently.”
The writing project group first came together in the summer of 2022 to gather input on the content for the collection in terms of gaps and opportunities, emerging areas of importance, and key topics, disciplines, and challenges, as well as gather examples of research that could be featured in the collection. The December 2022 retreat in Nairobi, Kenya, was the first to take place in person since the project was founded. In addition to Chimusa, attendees included the project’s other two cochairs—Dr. Catherine Kyobutungi, Executive Director of the African Population and Health Research Center and Dr. Kofi Amegah, Senior Lecturer of Epidemiology and Biostatistics at the University of Cape Coast— representatives from 15 writing teams, and guests from various organizations, including the Gates Foundation, Wellcome Trust, and the Network of African Medical Librarians.
“It was a privilege to bring together so many diverse experts from across the continent to discuss an exciting and potentially gamechanging tool for

improving health in Africa,” said Fogarty’s Dr. Amit Mistry who helped facilitate the meeting. This and future workshops will aim to improve synergy across teams and iron out issues by consolidating topics or changing the type of original research intended for the various papers. While there is still a lot of work to do on the collection, as one attendee put it, “I came to the retreat with doubts but am leaving here with convictions.”
When completed, this collection will include a mix of commentary articles, scoping reviews, and systematic reviews on a wide range of cross-cutting topics. The collection will be published fully open access and the co-chairs, Fogarty, and partners will plan a variety of dissemination and outreach activities to ensure the collection reaches beyond the academic community to policymakers and decision makers across the health and digital research communities.
“When the collection is published (in 2024), I want to see something we don’t already know,” remarked Kyobutungi. It should “spotlight really great work that has been hidden so far and challenge current narratives.”
64 Delaware Journal of Public Health - June 2023
Photos courtesy of Sheila Mwero
Project co-chair Catherine Kyobutungi speaks at the writers’ retreat. “When the collection is published, I want to see something we don’t already know.”
MARCH/APRIL 2023
Attendees at the State of Data Science for Health in Africa Writing Project retreat in Nairobi, Kenya, the first to take place in person since the project was founded.
PROFILE
Building HIV prevention awareness for mothers in India
Building HIV prevention awareness for mothers in India
By Mariah Felipe
By Mariah Felipe
“Medical school is not going to be enough.” That’s what former Fogarty fellow Dr. Jacqueline Firth said to herself during her first study abroad opportunity in Niger. At the time, she was an undergraduate at Georgetown University shadowing doctors at the national hospital treating a meningitis outbreak. Unfortunately, the hospital was so severely under-resourced that the same needle was used on several patients to do lumbar punctures. Firth says, “I wasn’t even in medical school at this point, but I knew then I needed to pursue a career in public health.”
“Medical school is not going to be enough.” That’s what former Fogarty fellow Dr. Jacqueline Firth said to herself during her first study abroad opportunity in Niger. At the time, she was an undergraduate at Georgetown University shadowing doctors at the national hospital treating a meningitis outbreak. Unfortunately, the hospital was so severely under-resourced that the same needle was used on several patients to do lumbar punctures. Firth says, “I wasn’t even in medical school at this point, but I knew then I needed to pursue a career in public health.”
Firth comes from a family of medicine. Her father was a cardiologist, her mother a nurse, and a family of physicians live back in South Africa, where her father was born. Her family background made the decision to enter the medical field easy, though she had always thought she would take the traditional route.
Firth comes from a family of medicine. Her father was a cardiologist, her mother a nurse, and a family of physicians live back in South Africa, where her father was born. Her family background made the decision to enter the medical field easy, though she had always thought she would take the traditional route.
“Initially, I thought I would take a solely clinical approach to it, but those projects in Niger helped me to see that public health can have as much impact as taking care of patients directly, so I ended up doing both.”
“Initially, I thought I would take a solely clinical approach to it, but those projects in Niger helped me to see that public health can have as much impact as taking care of patients directly, so I ended up doing both.”
Four years later, Firth became a member of Fogarty’s inaugural cohort of Fellows and Scholars in 2004. (Her cousin from South Africa, Dr. Richard Van-Zyl Smit, a pulmonologist, would also join the program a few years later.) During her Fogarty year in Vellore, India, Firth participated in two studies, one focused on surveying HIV exposure among pregnant women and another that tested the water-purifying qualities of moringa, a naturally occurring plant. The survey showed that while there was a low level of HIV among women in India at the time, awareness of HIV prevention methods was low. In her second project studying water purification methods, the team of researchers found that adding moringa did not help water cleanliness levels, though chlorine did. Despite this, the town where they conducted the study had an aversion to chlorinated water and ultimately chose not to use it despite it being the safest and healthiest option.
Four years later, Firth became a member of Fogarty’s inaugural cohort of Fellows and Scholars in 2004. (Her cousin from South Africa, Dr. Richard Van-Zyl Smit, a pulmonologist, would also join the program a few years later.) During her Fogarty year in Vellore, India, Firth participated in two studies, one focused on surveying HIV exposure among pregnant women and another that tested the water-purifying qualities of moringa, a naturally occurring plant. The survey showed that while there was a low level of HIV among women in India at the time, awareness of HIV prevention methods was low. In her second project studying water purification methods, the team of researchers found that adding moringa did not help water cleanliness levels, though chlorine did. Despite this, the town where they conducted the study had an aversion to chlorinated water and ultimately chose not to use it despite it being the safest and healthiest option.

 Jacqueline Firth, PhD
Jacqueline Firth, PhD
Fogarty Fellow: 2004-2005
Fogarty Fellow: 2004-2005
Foreign institution: Christian Medical College, Vellore, India
Foreign institution: Christian Medical College, Vellore, India
U.S. institutions: Tufts University and Brown University
U.S. institutions: Tufts University and Brown University Research topic: Child and maternal health

Research topic: Child and maternal health
Firth worked on the manuscripts for both projects, which took longer than usual because “natural disasters seemed to follow me at that time!” She and her housemate in India were in Sri Lanka when a tsunami devastated the region in 2004. And, after completing her Fogarty year in 2005, she arrived at Tulane University in New Orleans just in time to experience the damage and destruction of Hurricane Katrina sweeping through the region.
Firth worked on the manuscripts for both projects, which took longer than usual because “natural disasters seemed to follow me at that time!” She and her housemate in India were in Sri Lanka when a tsunami devastated the region in 2004. And, after completing her Fogarty year in 2005, she arrived at Tulane University in New Orleans just in time to experience the damage and destruction of Hurricane Katrina sweeping through the region.
Today, Firth serves as the Branch Chief of the Pediatric and Maternal Clinical HIV Branch at USAID. She and her team focus on ensuring that mothers and children enrolled in PEPFAR-funded HIV programs worldwide have robust support systems. They work with teams in other countries to ensure they have access to the latest research and best practices in medication protocols, care, retention, prevention, and testing. Specifically, they work to identify mothers and children that might have been missed during HIV testing which usually occurs before or after the birth of a child. They also support families whose children are in treatment, especially during adolescence, when many HIV-positive patients no longer want to maintain their drug regimens. She also continues her clinical work by volunteering at the Department of Health's Tuberculosis Control Program clinic in Washington, D.C., once a week.
Today, Firth serves as the Branch Chief of the Pediatric and Maternal Clinical HIV Branch at USAID. She and her team focus on ensuring that mothers and children enrolled in PEPFAR-funded HIV programs worldwide have robust support systems. They work with teams in other countries to ensure they have access to the latest research and best practices in medication protocols, care, retention, prevention, and testing. Specifically, they work to identify mothers and children that might have been missed during HIV testing which usually occurs before or after the birth of a child. They also support families whose children are in treatment, especially during adolescence, when many HIV-positive patients no longer want to maintain their drug regimens. She also continues her clinical work by volunteering at the Department of Health's Tuberculosis Control Program clinic in Washington, D.C., once a week.
Firth credits Fogarty and all her experiences from that year with preparing her for today. “Right now, in my USAID role, we help to run programs, but because of the work I did with Fogarty, I know what it takes to run these programs at the other end.”
Firth credits Fogarty and all her experiences from that year with preparing her for today. “Right now, in my USAID role, we help to run programs, but because of the work I did with Fogarty, I know what it takes to run these programs at the other end.”

65 PROFILE
4
4
WILCO ZILJMANS, MD, PHD
Dr. Wilco Zijlmans, head of pediatrics and lecturer at Anton de Kom University of Suriname, also serves as an adjunct full professor at Tulane University School of Public Health and Tropical Medicine. Zijlmans trained in pediatrics at the Academic Medical Center in Amsterdam, the Netherlands, and works at the Diakonessen Hospital in Paramaribo, Suriname, while also consulting for Primary Health Care Medical Mission Suriname. He is a member of the Global Child Health Group, a board member for the National Taskforce Tuberculosis/HIV, and a technical working group member of the Prevention of Mother-to-Child HIV Transmission, among other appointments. In 2015 he co-founded KidsClinic.
What are the findings of your Fogarty project?
Our project looks at maternal exposures to heavy metals and pesticides in different regions of Suriname and the possible effects on pediatric neurodevelopment. We found marked differences among the regions. The women in the interior had elevated mercury and lead levels far above international thresholds and significantly higher than in other regions of the country. This is partly due to their consumption of fish that have been contaminated due to illegal gold mining activities, which use mercury for processing.
Surprisingly, the women also had a lot of lead in their blood. Our colleagues in neighboring French Guiana have seen the same and they believe there's a relationship to consumption of cassava and game (since lead bullets are used to shoot game). When we looked deeper, we saw significant developmental delays at age 1 among the children of mothers with elevated lead levels. The delays continued up to 32 months. We want to follow them as they get older so we’re pursuing different grants to continue this work.
One of our eight Ph.D. students also measured concentrations of protective elements, like selenium and fatty acids, in fish. Selenium can have protective effects, acting as a counter measure to mercury, as do fatty acids. She used questionnaires to understand what and how much fish the women consumed and, once we have that data, we might do tailor-made advice—try to eat this fish, not that fish—though of course their diet depends on what they catch and the other available food sources.
What does public health look like in Suriname?
The government’s Regional Health office has different stations along the coastal area, while Primary Health Care Medical Mission Suriname (which was founded by three churches but is funded by the government) has more than 50 facilities scattered through the interior. The medical

mission, which serves the Amerindian and Maroon peoples, has a nice system of consultation, vaccination and school screenings. A lack of funding and, sometimes, a lack of organization can disrupt these systems. For example, ordering vaccines at the right time doesn’t always happen due to delayed payments, so there can be vaccine shortages.
Our Fogarty project created more awareness of the mercury problem and its impact on public health. Every year during our five-year project, we met with policymakers—the Minister of Health, community advisory boards, all relevant stakeholders—to communicate our findings to those who matter. It’s encouraging that Suriname has signed the Minamata Convention on Mercury, a worldwide treaty on diminishing the use of mercury.
What's ahead for you?
We’re pursuing grants to continue the work we’ve done with our field cohort, including funding from Fogarty, National Institute of Environmental Health Sciences (NIEHS), and interested organizations in the European Union. Currently, I’m also working with the medical mission and the psychiatry department of University of Groningen in the Netherlands on a project investigating mental health among indigenous people in Suriname. Their expression of stress and depression is different from ours and they possess protective qualities that we lack.
We are also working with the medical mission, using school screening data to look at anemia (low red blood cell counts) in children. Low iron levels, which cause anemia, impact neurological performance and achievement in school. The range of anemia is incredibly high both in pregnant women and in children from birth to 14. There’s a 60% rate of anemia among pregnant women, youngsters and school children in Suriname, higher than any other country in the region.
66 Delaware Journal of Public Health - June 2023
5
A&Q
FOCUS FOCUS
Fogarty Fellows and Scholars: A look back
Fogarty Fellows and Scholars: A look back
Fogarty’s Global Health Fellows and Scholars program has grown from its modest beginnings with only 35 scholars at 14 research institutions to supporting over 100 scholars at over 60 research institutions and sites each year. Support for the program also has grown as partners like the Ellison Medical Foundation, U.S. Department of State, and more than 25 NIH institutes, centers, and offices have partnered with Fogarty over the years—a substantial leap from the two partners who helped start the program.
Fogarty’s Global Health Fellows and Scholars program has grown from its modest beginnings with only 35 scholars at 14 research institutions to supporting over 100 scholars at over 60 research institutions and sites each year. Support for the program also has grown as partners like the Ellison Medical Foundation, U.S. Department of State, and more than 25 NIH institutes, centers, and offices have partnered with Fogarty over the years—a substantial leap from the two partners who helped start the program.
Now in its 20th year, the Global Health Fellows and Scholars program has been known by many names, mirroring its evolution in priorities, demand, and opportunities for greater impact. Nevertheless, with each change, the driving force remains the same: to inspire motivated early-career health professionals and researchers worldwide to pursue a career in global health research, strengthen and expand research collaborations between the U.S. and low- and middle-income countries (LMICs), and further enhance research capacity at LMIC research institutions and sites.
Now in its 20th year, the Global Health Fellows and Scholars program has been known by many names, mirroring its evolution in priorities, demand, and opportunities for greater impact. Nevertheless, with each change, the driving force remains the same: to inspire motivated early-career health professionals and researchers worldwide to pursue a career in global health research, strengthen and expand research collaborations between the U.S. and low- and middle-income countries (LMICs), and further enhance research capacity at LMIC research institutions and sites.
In 2003, Fogarty partnered with the Ellison Medical Foundation to establish the Fogarty-Ellison Overseas Fellowship in Global Health and Clinical Research Training. The program was created to inspire students early in their professional training to consider a career in global health research by offering them first-hand exposure to challenging health issues faced by those living in LMICs and an opportunity to forge career-boosting relationships and scientific collaborations. Specifically, the program provided graduate-level U.S. students in the health sciences one year of clinical research training in an LMIC while also strengthening the research capacity in the country of study by supporting a matched or “twin” LMIC student. Fellows were placed at research institutions and sites with active NIH- and Fogarty-funded research and training programs allowing them access to accomplished U.S. and LMIC researchers who served as program mentors.
In 2003, Fogarty partnered with the Ellison Medical Foundation to establish the Fogarty-Ellison Overseas Fellowship in Global Health and Clinical Research Training. The program was created to inspire students early in their professional training to consider a career in global health research by offering them first-hand exposure to challenging health issues faced by those living in LMICs and an opportunity to forge career-boosting relationships and scientific collaborations. Specifically, the program provided graduate-level U.S. students in the health sciences one year of clinical research training in an LMIC while also strengthening the research capacity in the country of study by supporting a matched or “twin” LMIC student. Fellows were placed at research institutions and sites with active NIH- and Fogarty-funded research and training programs allowing them access to accomplished U.S. and LMIC researchers who served as program mentors.
The recruitment, selection and matching of trainees were managed through a collaboration with the Association of
The recruitment, selection and matching of trainees were managed through a collaboration with the Association of
American Medical Colleges (AAMC) and the Association of Schools of Public Health (ASPH). After submission, applications were reviewed by an AAMC review panel, followed by the Fogarty-Ellison program steering committee. Selected semi-finalists were then invited to the NIH campus to present their research proposals, learn more about the global health research funded by NIH, and interview with representatives from the LMIC institutions and sites.
American Medical Colleges (AAMC) and the Association of Schools of Public Health (ASPH). After submission, applications were reviewed by an AAMC review panel, followed by the Fogarty-Ellison program steering committee. Selected semi-finalists were then invited to the NIH campus to present their research proposals, learn more about the global health research funded by NIH, and interview with representatives from the LMIC institutions and sites.
Final selection of the U.S. trainees depended on the rank matching of finalists and LMIC site representatives, research priorities of funders, and availability of funds. The LMIC institutions and sites underwent their own rigorous application and selection processes to match the U.S. trainees with a host-country trainee with similar research interests.
Final selection of the U.S. trainees depended on the rank matching of finalists and LMIC site representatives, research priorities of funders, and availability of funds. The LMIC institutions and sites underwent their own rigorous application and selection processes to match the U.S. trainees with a host-country trainee with similar research interests.


Trainee projects initially focused mainly on HIV and other infectious diseases. With additional financial support from NIH partners, the range of research topics has broadened to include areas like nephrology, heart disease, neurological disorders, mental health and cancer, to name a few. However, before being embedded into well-established research teams, the U.S. and matched LMIC trainees began their program year with an orientation at NIH. This event, a favored tradition still held every year, is an opportunity to meet the new cohort of program participants, discuss important topics in global health, and energize and inspire the trainees before beginning their “Fogarty” year.
Trainee projects initially focused mainly on HIV and other infectious diseases. With additional financial support from NIH partners, the range of research topics has broadened to include areas like nephrology, heart disease, neurological disorders, mental health and cancer, to name a few. However, before being embedded into well-established research teams, the U.S. and matched LMIC trainees began their program year with an orientation at NIH. This event, a favored tradition still held every year, is an opportunity to meet the new cohort of program participants, discuss important topics in global health, and energize and inspire the trainees before beginning their “Fogarty” year.
In 2007, with the anticipated growth in size and complexity of the program, Fogarty changed its structure to become more centralized and awarded a grant to Vanderbilt University with recruitment support from AAMC and ASPH. The program also expanded to include both predoctoral students (scholars) and postdoctoral fellows. The redesigned program, renamed the Fogarty International Clinical Research Scholars and Fellows Program (FICRS-F), bridged the gap in Fogarty’s global health research career pipeline between completion of graduate training and readiness to apply for career development and research grants. Fogarty later partnered with the U.S. Department of State’s
In 2007, with the anticipated growth in size and complexity of the program, Fogarty changed its structure to become more centralized and awarded a grant to Vanderbilt University with recruitment support from AAMC and ASPH. The program also expanded to include both predoctoral students (scholars) and postdoctoral fellows. The redesigned program, renamed the Fogarty International Clinical Research Scholars and Fellows Program (FICRS-F), bridged the gap in Fogarty’s global health research career pipeline between completion of graduate training and readiness to apply for career development and research grants. Fogarty later partnered with the U.S. Department of State’s
67
FOCUS FOCUS
The inaugural cohort at orientation in 2004
The inaugural cohort at orientation in 2004
Bureau of Educational and Cultural Affairs in 2010 to establish additional training opportunities for U.S. graduate students and, for a short time, postdoctorates through the Fulbright-Fogarty Fellowship in Public Health. Although managed like a traditional Fulbright fellowship, the trainees are integrated into the Fogarty-supported research training programs.

The substantial growth of the program over the ensuing years called for another restructuring in 2012. The new Fogarty Global Health Program for Fellows and Scholars supported five consortia, each consisting of four U.S. institutions—including minority serving institutions, for most—plus LMIC research partners. Participating research training institutions and mentors came from the network of established research collaborations between faculty at the consortia’s U.S. institutions and those in LMICs. Each consortium developed its own global health research training program.

The consortia in this phase of the program were VECD, led by Vanderbilt University; NPGH, led by the University of Washington; UJMT, led by the University of North Carolina; GHES, led by the University of California, Berkeley; and GloCal, led by the University of California, San Francisco. In 2017, the renamed Fogarty Global Health Training Program grew to six consortia, welcoming HBNU, led by Harvard University.
Now in its fifth cycle, the program has a name that better reflects its intentions: the Launching Future Leaders in Global Health (LAUNCH) Research Training Program. It retains the consortia structure, with a refocus on training predominately postdoctoral fellows from the U.S. and LMICs and U.S. predoctoral students. LAUNCH emphasizes broadening participation to diverse groups in the U.S. It also aims to ensure a more equitable training experience for LMIC trainees with short-term research training in the U.S. The current consortia include NPGH, UJMT, GHES, GloCal, and HBNU, with the addition of two new consortia, INSIGHT, led by the University of Maryland-Baltimore, and ACHIEVE, led by Washington University in St. Louis.
Over the last 20 years, this program has ‘LAUNCHed’ the careers of hundreds of global health researchers. Trainees have gone on to publish many dozens of articles in peer-reviewed journals, and many have continued their research with subsequent funding from NIH. We have highlighted the achievements of many fellows and scholars over the years, but for every profile you read there are countless more success stories and an immeasurable impact on the field of global health research.

68 Delaware Journal of Public Health - June 2023 FOCUS ON FOGARTY FELLOWS AND SCHOLARS – CELEBRATING 20 YEARS
Dr. Francis Collins poses with trainees at the 2015 orientation.
Photos: Fogarty International Center
Left: Former Fogarty Director Roger Glass (left) poses with fellows at the 2011 orientation, Bottom: The 2014-15 cohort outside the Stone House on the NIH campus.
One program, global impact
One program, global impact
Over the past 20 years, Fogarty’s Global Health Fellows & Scholars program has influenced the careers of hundreds of young scientists, sparking their interest in global health by enabling them to conduct hands-on research in developing countries. Many have emerged committed to pursuing global health careers and with initial study results that have formed the basis for fundable grant applications. The program’s impact has reached around the globe while transforming the lives of many of its over 1,450 alumni.
Over the past 20 years, Fogarty’s Global Health Fellows & Scholars program has influenced the careers of hundreds of young scientists, sparking their interest in global health by enabling them to conduct hands-on research in developing countries. Many have emerged committed to pursuing global health careers and with initial study results that have formed the basis for fundable grant applications. The program’s impact has reached around the globe while transforming the lives of many of its over 1,450 alumni.
A truly global experience
A truly global experience
Forty-eight countries hosted at least one research site from 2004 to 2021. The number of sites and countries expanded during each cohort. The first, the Fogarty-Ellison Overseas Fellowship in Global Health and Clinical Research Training, had sites in 15 countries. Fogarty International Clinical Research Scholars and Fellows Program expanded to 24 countries. In 2012, trainees were scattered across 34 countries. Starting in 2017, this expanded to 39 countries. In the first LAUNCH cohort, alumni trained in 27 countries. Due to economic shifts and NIH requirements, some countries which participated in earlier years have had no fellows or scholars in recent years.
Forty-eight countries hosted at least one research site from 2004 to 2021. The number of sites and countries expanded during each cohort. The first, the Fogarty-Ellison Overseas Fellowship in Global Health and Clinical Research Training, had sites in 15 countries. Fogarty International Clinical Research Scholars and Fellows Program expanded to 24 countries. In 2012, trainees were scattered across 34 countries. Starting in 2017, this expanded to 39 countries. In the first LAUNCH cohort, alumni trained in 27 countries. Due to economic shifts and NIH requirements, some countries which participated in earlier years have had no fellows or scholars in recent years.

Countries that have hosted Fellows & Scholars
Countries that have hosted Fellows & Scholars
• Argentina
• Malaysia
Expanding reach and impact with support from NIH partners
Expanding reach and impact with support from NIH partners
The Fellows & Scholars program grants are leveraged with generous support—financial and otherwise— from many NIH Institutes and Centers, which greatly expands the reach and impact of the program to advance science and build the next generation of global health leaders.
The Fellows & Scholars program grants are leveraged with generous support—financial and otherwise— from many NIH Institutes and Centers, which greatly expands the reach and impact of the program to advance science and build the next generation of global health leaders.

FUNDING TO FELLOWS & SCHOLARS PROGRAM
FUNDING TO FELLOWS & SCHOLARS PROGRAM
Total funding by Fogarty (FIC) and NIH partners in the Global Health Fellows and Scholars/LAUNCH program, 2004-2021
Ensuring an equitable experience
Ensuring an equitable experience
• Bangladesh
• Argentina
• Bolivia
• Bangladesh
• Bolivia
• Botswana
• Botswana
• Brazil
• Brazil
• Cameroon
• Cameroon
• Chile
• Chile
• China
• China
• Columbia
• Columbia
• Costa Rica
• Costa Rica
• Dominican Republic
• Dominican Republic
• Democratic Republic of the Congo
• Democratic Republic of the Congo
• Ecuador
• Ecuador
• Ethiopia
• Ethiopia
• Georgia
• Ghana
• Georgia
• Ghana
• Guatemala
• Guatemala
• Haiti
• Haiti
• Honduras
• Honduras
• India
• India
• Jamaica
• Jamaica
• Kenya
• Kenya
• Liberia
• Liberia
• Malawi
• Malawi
• Mali
• Malaysia
• Mali
• Mexico
• Mexico
• Mozambique
• Mozambique
• Nepal
• Nepal
• Nicaragua
• Nigeria
• Nicaragua
• Nigeria
• Panama
• Panama
• Peru
• Peru
• Russia
• Russia
• Rwanda
• Rwanda
• Samoa
• Samoa
• Senegal
• Senegal
• Sierra Leone
• Sierra Leone
• South Africa
• South Africa
• Sri Lanka
• Sri Lanka
• Suriname
• Suriname
• Tanzania
• Tanzania
• Thailand
• Thailand
• Uganda
As part of Fogarty’s goal to build future leaders in global health research, the Fellows & Scholars program has always included trainees from both the U.S. and low- and middle-income countries (LMICs). In earlier iterations of the program, LMIC participants were only able to work in their country for the duration of their project. To ensure a more equitable training experience, the LAUNCH program now brings LMIC trainees to the U.S. for short-term research training experiences.
As part of Fogarty’s goal to build future leaders in global health research, the Fellows & Scholars program has always included trainees from both the U.S. and low- and middle-income countries (LMICs). In earlier iterations of the program, LMIC participants were only able to work in their country for the duration of their project. To ensure a more equitable training experience, the LAUNCH program now brings LMIC trainees to the U.S. for short-term research training experiences.

• Uganda
• Ukraine
• Ukraine
• Vietnam
• Vietnam
• Zambia
• Zambia
• Zimbabwe
• Zimbabwe
69 FOCUS ON FOGARTY FELLOWS AND SCHOLARS – CELEBRATING 20 YEARS
Percentage Of U.S. and LMIC trainees in the Global Health Fellows and Scholars/LAUNCH program over time
FOCUS ON FOGARTY FELLOWS AND SCHOLARS – CELEBRATING 20 YEARS
n FIC n NIH Partners
Percentage Of U.S. and LMIC trainees in the Global Health Fellows and Scholars/LAUNCH program over time
Total funding by Fogarty (FIC) and NIH partners in the Global Health Fellows and Scholars/LAUNCH program, 2004-2021
n FIC n NIH Partners
n LMIC Trainees n US Trainees
FOGARTY’S LAUNCH PROGRAM HAS BEEN A CRITICAL VEHICLE FOR CONCRETELY DEMONSTRATING NIH’S INTEREST AND INVESTMENT IN GLOBAL HEALTH.” – SATISH GOPAL


CONCRETELY DEMONSTRATING NIH’S INTEREST AND INVESTMENT IN GLOBAL HEALTH.” – SATISH GOPAL
LAUNCHing global health leaders: A former Fellow’s perspective
LAUNCHing global health leaders: A former Fellow’s perspective
LAUNCHing global health leaders: A former Fellow’s perspective
While the program was not called LAUNCH when I began my Fogarty global health fellowship in 2012, the new name is unmistakably appropriate. Indeed, the program has effectively LAUNCHED the careers of countless global health luminaries worldwide who have made and will make seminal contributions to global public health.
While the program was not called LAUNCH when I began my Fogarty global health fellowship in 2012, the new name is unmistakably appropriate. Indeed, the program has effectively LAUNCHED the careers of countless global health luminaries worldwide who have made and will make seminal contributions to global public health.
While the program was not called LAUNCH when I began my Fogarty global health fellowship in 2012, the new name is unmistakably appropriate. Indeed, the program has effectively LAUNCHED the careers of countless global health luminaries worldwide who have made and will make seminal contributions to global public health.
In 2012, the statement “I want to be an oncologist and NIH-supported physician-scientist living and working in Africa” was not easily understood at most cancer centers in the U.S. When I was able to add that I had received some initial NIH funding for this endeavor, thanks to Fogarty and the National Cancer Institute (NCI) as one of the very first Fogarty Global Health Fellows working on cancer, people started to listen. The opportunity created by my fellowship essentially catalyzed the creation of a new faculty position for me for which there was no institutional precedent.
In 2012, the statement “I want to be an oncologist and NIH-supported physician-scientist living and working in Africa” was not easily understood at most cancer centers in the U.S. When I was able to add that I had received some initial NIH funding for this endeavor, thanks to Fogarty and the National Cancer Institute (NCI) as one of the very first Fogarty Global Health Fellows working on cancer, people started to listen. The opportunity created by my fellowship essentially catalyzed the creation of a new faculty position for me for which there was no institutional precedent.
In 2012, the statement “I want to be an oncologist and NIH-supported physician-scientist living and working in Africa” was not easily understood at most cancer centers in the U.S. When I was able to add that I had received some initial NIH funding for this endeavor, thanks to Fogarty and the National Cancer Institute (NCI) as one of the very first Fogarty Global Health Fellows working on cancer, people started to listen. The opportunity created by my fellowship essentially catalyzed the creation of a new faculty position for me for which there was no institutional precedent.
Even after this, and like many of us with global health interests, I often felt adrift during my early career in a largely U.S.-oriented biomedical research enterprise. It is very easy to wonder if such career aspirations are even possible or worthy of pursuit and if a more conventional path is the only way. Connection to the worldwide community of Fogarty supported fellows and investigators is a fantastic antidote to this isolation and can be galvanizing for many of us who
Even after this, and like many of us with global health interests, I often felt adrift during my early career in a largely U.S.-oriented biomedical research enterprise. It is very easy to wonder if such career aspirations are even possible or worthy of pursuit and if a more conventional path is the only way. Connection to the worldwide community of Fogarty supported fellows and investigators is a fantastic antidote to this isolation and can be galvanizing for many of us who
Even after this, and like many of us with global health interests, I often felt adrift during my early career in a largely U.S.-oriented biomedical research enterprise. It is very easy to wonder if such career aspirations are even possible or worthy of pursuit and if a more conventional path is the only way. Connection to the worldwide community of Fogarty supported fellows and investigators is a fantastic antidote to this isolation and can be galvanizing for many of us who
20 YEARS OF GROWTH
20 YEARS OF GROWTH
may not have a robust global health community available to us locally.
may not have a robust global health community available to us locally.
may not have a robust global health community available to us locally.
However, what I consider one of the fellowship’s most important benefits is the access to role models and mentors. Many household names in global health research had come through Fogarty programs before leading the way to foundational discoveries or paradigm-shifting research and this provided me and others with clear role models we could emulate. It is difficult to envision a path you haven’t seen, and LAUNCH made certain that I could always see a path before me.
However, what I consider one of the fellowship’s most important benefits is the access to role models and mentors. Many household names in global health research had come through Fogarty programs before leading the way to foundational discoveries or paradigm-shifting research and this provided me and others with clear role models we could emulate. It is difficult to envision a path you haven’t seen, and LAUNCH made certain that I could always see a path before me.
However, what I consider one of the fellowship’s most important benefits is the access to role models and mentors. Many household names in global health research had come through Fogarty programs before leading the way to foundational discoveries or paradigm-shifting research and this provided me and others with clear role models we could emulate. It is difficult to envision a path you haven’t seen, and LAUNCH made certain that I could always see a path before me.
Since my Fogarty fellowship, I have been fortunate to receive subsequent grants from Fogarty and NCI that allowed me to stay in Malawi and build local capacity while investigating questions of local importance alongside Malawian colleagues and collaborators. I was fortunate to be recruited to NCI in 2020 to direct its Center for Global Health, where we seek to leverage our immense NCI resources and capabilities as the largest funder of cancer research in the world to help address cancer as the urgent global public health problem that it is.
Since my Fogarty fellowship, I have been fortunate to receive subsequent grants from Fogarty and NCI that allowed me to stay in Malawi and build local capacity while investigating questions of local importance alongside Malawian colleagues and collaborators. I was fortunate to be recruited to NCI in 2020 to direct its Center for Global Health, where we seek to leverage our immense NCI resources and capabilities as the largest funder of cancer research in the world to help address cancer as the urgent global public health problem that it is.
Since my Fogarty fellowship, I have been fortunate to receive subsequent grants from Fogarty and NCI that allowed me to stay in Malawi and build local capacity while investigating questions of local importance alongside Malawian colleagues and collaborators. I was fortunate to be recruited to NCI in 2020 to direct its Center for Global Health, where we seek to leverage our immense NCI resources and capabilities as the largest funder of cancer research in the world to help address cancer as the urgent global public health problem that it is.
In sum, my participation in LAUNCH provided the seed investment, support system, and destination guide that made my career possible, as it has done for so many.
In sum, my participation in LAUNCH provided the seed investment, support system, and destination guide that made my career possible, as it has done for so many.
In sum, my participation in LAUNCH provided the seed investment, support system, and destination guide that made my career possible, as it has done for so many.
Fogarty’s Global Health Fellows and Scholars program has grown from its modest beginnings with only 35 scholars at 14 research institutions to supporting over 100 scholars at over 60 research institutions and sites each year.
20 YEARS OF GROWTH
Fogarty’s Global Health Fellows and Scholars program has grown from its modest beginnings with only 35 scholars
Fogarty’s Global Health Fellows and Scholars program has grown from its modest beginnings with only 35 scholars at 14 research institutions to supporting over 100 scholars at over 60 research institutions and sites each year.

Delaware Journal of Public Health - June 2023
“
“
FOGARTY’S
LAUNCH PROGRAM HAS BEEN A CRITICAL VEHICLE FOR
“
FOGARTY’S LAUNCH PROGRAM HAS BEEN A CRITICAL VEHICLE FOR CONCRETELY DEMONSTRATING NIH’S INTEREST AND INVESTMENT IN GLOBAL HEALTH.” – SATISH GOPAL
OPINION
Fellows & Scholars at 20
By Dr. Peter Kilmarx, Acting Director, Fogarty International Center



As Deputy Director of the Fogarty International Center for the last seven years and now as Acting Director, it has always been a pleasure to meet the Fogarty Global Health Fellows and Scholars in their annual orientation or at their research sites around the world. Hearing about their many accomplishments and seeing the impact of former Fellows and Scholars over the years has been truly remarkable.
It is extraordinary to see how a single year can have such a profound, defining influence on one’s life and career. Being exposed to new cultures and seeing up close some of the health care challenges in resourcepoor settings is very inspiring for the U.S. trainees. Seeing the power of research and discovering how to improve health and health systems is highly motivating for all participants. Receiving mentorship and developing networks are also critical aspects of the professional development our trainees get during their “Fogarty year.” Many former trainees describe how they have mentored those who came after them, paying back the benefit to the next generation, like Dr. Gerald Bloomfield, a 200910 Fellow, who mentored Dr. Anubha Agarwal, a Fogarty Fellow in 2017-18.
The mission of the Fogarty International Center is to support and facilitate research, build partnerships, and train the next generation of scientists. Even in the short term, the Fellows and Scholars Program is highly effective in advancing these goals. The career trajectories of former trainees and their leadership roles in global health research, education, programs, and policies affirms that this program is a great long-term investment and a “best buy” for Fogarty that should be continued long into the future.
We are very grateful to the many program leaders, staff, and mentors in the United States and around the world for their vision, commitment, and hard work on behalf of the trainees over these past two decades. The seven consortia in the current Launching Future Leaders in Global Health (LAUNCH) Research Training Program and their global partners may be especially commended for their commitment to including trainees with diverse backgrounds and promoting equity for the international

program participants. We’re thankful for the support of more than a dozen other NIH Institutes, Centers, and Offices. Their funding is important, but perhaps more significant are the linkages with their networks of researchers, mentors, and programs, building global health research capacity, partnerships, and careers across a wide span of scientific disciplines and health specialties.
I also appreciate the many Fogarty staff who have dedicated their professional time and energy to supporting this program, especially those in the Division of International Training and Research and also the Office of Communications, who publicize the successes of the trainees. Of course, we applaud the Fellows and Scholars themselves who dedicated a year of their lives early in their careers to a research training experience, which, with great dedication and effort, in many cases led to lifelong commitments. Finally, we all are indebted to Dr. Roger Glass, who, as the Fogarty Director for 17 of the 20 years of this program, was a tireless champion of the grantees and the trainees, personally connecting with and encouraging them and recruiting support for them from across NIH and around the world.
Congressman John E. Fogarty, for whom our Center was named, was a representative from my home state of Rhode Island and an extraordinarily effective promoter of NIH and international health research and training. He was prescient in his vision, stating, “I think that this matter of expanding research is one, perhaps the one, truly global effort in which all nations can and will join as real partners.” The most compelling and recurring theme in the Fellow and Scholar profiles we have written over the years is how real partnerships were formed through the Fogarty Global Health Fellows and Scholars/LAUNCH Program across borders, institutions, professions, and generations. Congressman Fogarty would be astonished, ecstatic, and very proud.
71
It is extraordinary to see how a single year can have such a profound, defining influence on one’s life and career.
“ ”
CDC names director, deputy director for global health
CDC has selected Dr. Kayla Laserson as director of its Global Health Center. Laserson was formerly CDC’s India country director, director of the Kenya Medical Research Institute (KEMRI)/CDC Research and Public Health Collaboration, and deputy director for infectious diseases and vaccine delivery at the Bill and Melinda Gates Foundation.
Dr. Howard Zucker was recently named the CDC deputy director for global health, overseeing the planning and management of global programs. Previously, he served as Commissioner of Health for New York State and Assistant Director General at WHO and is board certified in six specialties, with experience in pediatrics, anesthesiology, and critical care.
Africa CDC names director general


The African Union appointed Dr. Jean Kaseya, a medical doctor from the Democratic Republic of the Congo (DRC), as the first director general of the Africa Centres for Disease Control and Prevention. Kaseya was a senior advisor to the president of the DRC and previously worked at UNICEF, GAVI Alliance, and WHO.

WHO appoints new malaria program director
Dr. Daniel Ngamije Madandi has been appointed Director of the WHO Global Malaria Programme. Ngamije previously served as the Rwandan Minister of Health and National Programme Officer for Malaria and NTDs at WHO Rwanda. In this role, he will lead efforts to combat malaria and strengthen pandemic prevention and response capacities worldwide.
OAR director transitions to new role
Dr. Maureen M. Goodenow, former director of the NIH Office of AIDS Research (OAR), has transitioned to a new role as senior advisor in the NIH Office of the Director. Goodenow led OAR for nearly seven years and was the first woman to serve in the position since its establishment in 1988.


Former DAIDS director, Ed Tramont passes
Retired Army Colonel, and former director of the Division of AIDS at NIAID, Dr. Edmund Tramont, has passed away. Tramont most recently worked in NIAID's Clinical Research Division, advising researchers on emerging diseases, including COVID-19. He is recognized for significant contributions to the research and development of vaccines and treatments for HIV/AIDS.

NASEM releases guidance on population descriptors
The National Academies of Science, Engineering, and Medicine (NASEM) report, Using Population Descriptors in Genetics and Genomics Research, funded in part by NIH, focuses on understanding the current use of population descriptors in genomics research, examining best practices for researchers, and identifying processes for adopting best practices within the biomedical and scientific communities.
Africa CDC publishes pathogens list
The list will inform strategic planning and help effective resource allocation to manage health emergencies. Publishing the list is viewed as a critical step for effective response to limit the spread of diseases and minimize morbidity and mortality as well as social and economic disruptions.
HIV treatment up 300% thanks to PEPFAR
A CDC report found that the number of people receiving lifesaving HIV treatment through PEPFAR has increased 300 times in under 20 years. The percentage of people receiving HIV treatment through PEPFAR with a viral load test who subsequently tested as virally suppressed also increased from 80% to 95% between 2015 and 2022, the report notes.
Supplement on COVID & inequality published
A special issue of the International Journal for Equity in Health on COVID-19 and inequality includes eight articles spanning topics from immunization to testing, as well as information about software and databases that can aid researchers, analysts and policymakers interested in monitoring health inequalities.
USAID launches framework to prevent child, maternal deaths
The strategic framework lays out an action plan to measurably improve health outcomes for women and children by reducing preventable child and maternal mortality in 25 priority countries. It also aims to increase coverage levels of lifesaving interventions.
72 Delaware Journal of Public Health - June 2023
PEOPLE 11
HEALTH Briefs Global
Funding Opportunity Announcement
International Bioethics Training
D43 Clinical Trial Optional
R25 Clinical Trial Not Allowed
Chronic, Noncommunicable Diseases and Disorders Research Training

Jun 6, 2023
Jul 13, 2023
http://bit.ly/BioethicsTraining
http://bit.ly/NCDtrain
Global Infectious Diseases (GID) http://bit.ly/GID-FIC
Fogarty HIV Research Training
G11 Clinical Trials Not Allowed
D71 Clinical Trial Not Allowed
For more information, visit www.fic.nih.gov/funding
Global Health Matters
March/April 2023
Volume 22, No. 2 ISSN: 1938-5935
Fogarty International Center National Institutes of Health Department of Health and Human Services
Managing editor: Judy Coan-Stevens Judith.Coan-Stevens@nih.gov
Writer/editor: Mariah Felipe Mariah.Felipe@nih.gov
Writer/editor: Susan Scutti Susan.Scutti@nih.gov
Digital analyst: Merrijoy Vicente Merrijoy.Vicente@nih.gov
Designer: Carla Conway
All text produced in Global Health Matters is in the public domain and may be reprinted. Please credit Fogarty International Center. Images must be cleared for use with the individual source, as indicated.
Scan and read this issue online

SUBSCRIBE: www.fic.nih.gov/subscribe
Aug 3, 2023
Aug 22, 2023
http://bit.ly/NIHGlobalHIV
Don’t let a simple mistake cost you a grant
When you submit an application that includes a clinical trial as part of your project, make sure you apply to the correct notice of funding opportunity (NOFO)— the one designated “clinical trial required or optional.” If, by accident, you submit to a NOFO where clinical trials are not allowed, your application will be returned without review. In the past, reviewers could simply label these as “misclassified” and still enter the application into the review process, but in 2018, NIH revised its procedures. Now, these applications are automatically disqualified.
To avoid such a mistake, you should review all requirements to make sure you’re applying to the correct funding opportunity notice. NIH defines a clinical trial as “a research study in which one or more human subjects are prospectively assigned to one or more interventions (which may include placebo or other control) to evaluate the effects of those interventions on health-related biomedical or behavioral outcomes.” More details are available on grants.nih.gov.
The revised process has improved NIH's ability to identify clinical trials, uniformly apply review criteria, and ensure appropriate data collection and reporting. NIH terminology has also changed; the term "Funding Opportunity Announcement" (FOA) has been phased out and "Notice of Funding Opportunity" (NOFO) is now the preferred term.
73 MARCH/APRIL 2023
Photo courtesy of Magaly Blas
Details
Deadline
Remember to review all requirements, especially those around clinical trials, to make sure you’re applying to the correct funding opportunity notice.
Solving Homelessness in Delaware Requires Resolving the Disparities That Cause It
Sequoia Rent, B.A. Bureau Chief, Health Equity, Delaware Division of Public Health
ABSTRACT
There are several paths to homelessness for adults and families, including a lack of affordable housing, financial crises such as unemployment, underemployment and low wages, and domestic violence. For youth, homelessness can be the result of running away from family conflict, family poverty, domestic violence, being put out of their homes, or loss of resources after aging out of state programs like foster care. The aim of this essay is to discuss the common paths to homelessness for adults, youth, and survivors of domestic violence as well as the associated health outcomes related to homelessness in relation to health equity and the social determinants of health. Additionally, this piece identifies existing disparities in homelessness, highlights Delaware resources, and seeks ways that Delaware can end involuntary homelessness in Delaware. Homelessness disproportionately affects minority populations more than other groups and has direct adverse health consequences on these populations. The poor health outcomes linked to homelessness can be many, co-occurring, and lifelong. If social determinants continue to be lacking, homelessness can become chronic. Homelessness is a prevalent public health issue in Delaware. With a health equity lens, state and community resources and solutions can be applied to help reduce homelessness and its disparities.
INTRODUCTION
Each day you get up, shower, dress, grab food from your kitchen, get in your car, and head to work. In contrast, an unsheltered person experiencing homelessness gets up, packs their belongings, walks to the nearest publicly accessible bathroom, checks the stalls, and finding no one, can have privacy to clean themselves and their child. Then they need to find food and get their child to school. Even with a job working 30 hours a week, more than their income is necessary for reliable transportation and a safe, permanent home for themselves and their family.
According to evidence-based data, in multiple studies, the homeless and home insecure are vulnerable populations that face increased risks for poor health outcomes, and homelessness predominately affects minority populations.1–12 The disparities in the prevalence of adverse health outcomes and risk factors in minority populations due to inequitable access to health care, education, and environmental or socioeconomic factors experienced by socially disadvantaged groups are preventable differences.12
ADVERSE HEALTH OUTCOMES AND DISPARITIES WITHIN THE HOMELESS POPULATION
The adverse health outcomes resulting from homelessness include increased mortality rates, pre-term birth and low birth weight infants in pregnant mothers, increased risk of mental health and substance abuse disorders, increased risk of infectious diseases, and high rates of suicidal thoughts.1–5,11 Other harmful outcomes associated with homelessness include increased vulnerability to trauma such as sexual assault or victimization, chronic homelessness, delay and lapse in seeking care, and increased risky behaviors.3,11
Sixty-one percent of people experiencing homelessness in the U.S. in 2022 identified as African, African American or Black and Hispanic/Latino/a/x.7 Persons identifying as Black are four times more likely to experience homelessness than persons identifying as White in their lifetime.10 The 2022 Annual Homelessness Assessment Report (AHAR) reported that 37% of all persons experiencing homelessness and 50% of families with children identified as Black nationally.7 Black residents accounted for 61% of the total Delaware homeless population – nearly twothirds – according to the data.6–9 Comparatively, Black residents comprise only 23% of the Delaware population.9 Among homeless Delawareans in 2022, 6% identified as Hispanic or Latino/a/x.6 Asian or Asian American, American Indian, Alaska Native or Indigenous, Native Hawaiian or Other Pacific Islander, and persons identifying as more than one race accounted for just over 7% of homeless Delawareans.6 The combined outcomes, risks, and disparities elevate homelessness to a public health and health equity priority.
DELAWARE HOMELESSNESS BY THE NUMBERS
Delaware’s homeless or home insecure, which comprise people in a variety of unstable living situations, includes those outlined in the proposed Delaware 2023 House Bill 55, Bill of Rights for Individuals Experiencing Homelessness13:
• An individual who is living in a place not meant for human habitation or in a temporary shelter
• An individual who is exiting an institution and who met the…status of living or having lived on the street, in a temporary shelter, or other temporary residence immediately before entering the institution
• An individual who will lose the individual’s housing within 14 days
74 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.13
• An unaccompanied youth or a guardian with a child that does not have housing and is unlikely to obtain housing, including an unaccompanied youth or guardian with a child that satisfies either of the following:
⚬ Has not had a lease or ownership interest in a housing unit in at least the previous 60 days and is unlikely to obtain housing
⚬ Changed housing at least twice in the last 60 days, and who is unlikely to obtain housing
• An individual who is fleeing or attempting to flee domestic abuse, has no other housing, and lacks the resources or support networks to obtain housing
• An individual regarded as being an individual experiencing homelessness.
The proposed Delaware Bill of Rights for Individuals
Experiencing Homelessness acknowledges homelessness as an issue at the state level. If passed, the bill would support the current resources to tackle the adverse health outcomes and inequities faced by people experiencing homelessness and home insecurity, discussed later in this essay.
Continuums of Care (CoC) located in the regions and locales throughout the U.S. perform annual Point-in-Time Counts of sheltered and unsheltered persons experiencing homelessness on a single night in each state, usually within the last ten days of January.7 According to the 2007-2022 Point in Time Estimates by State, there were 2,369 homeless individuals in Delaware in 2022, which is more than double the 1,082 homeless individuals counted in 2018 (Figure 1).7
The 2022 AHAR reports that Delaware is one of three states with the largest percentage increase in homelessness, a rise of 103% from 2020 to 2022.7 This is a new trend; Delaware had the second largest percentage increase in the number of individuals experiencing homelessness from 2007 to 2022.7 Delaware was also one of 26 states reported to have increases in families with children who experienced homelessness

between 2020 and 2022, impacted by the Coronavirus 2019 (COVID-19) pandemic.7,8 As the numbers rose, the Delaware Department of Health and Social Services, Division of State Service Centers (DSSC) increased emergency housing, and the State served as the largest emergency shelter provider in 2021 and 2022.8 Moreover, Delaware was one of three states having the largest absolute increases of families with children experiencing homelessness, a total increase of 205%, totaling 876 more individuals, from 2020 to 2022.7 This rise coincides with the increase in family homelessness during the more extended period from 2007 to 2022, with Delaware showing the most significant documented percentage increase of 278%, totaling 959 individuals.7 These increases tell an unavoidable truth: this Delaware issue needs improvement.
Common factors contributing to homelessness are linked to the social determinants of health (SDoH) and vital conditions1 that can lead to poor health outcomes. The Centers for Disease Control and Prevention (CDC) lists these SDoH related to homelessness and housing instability: economic stability; access to quality education; access to quality health care; the neighborhood and built environment; and social and community context.1 Tracking these data and indicators help to identify communities and precise geographic locations where inequities harm vulnerable populations. The Equity Counts Data Center within Delaware’s My Healthy Community (MHC) portal is a prime place to research these health concerns among home-insecure Delawareans. One can find geographically based state data such as the Social Vulnerability Index indicators by census tract. For example, census tract 504.06 covers a portion of Seaford, Delaware, and has an overall vulnerability ranking of 0.98 out of 1.0, indicating a high level of vulnerability.14 Additional vulnerability ranking data can be tracked, such as socioeconomic status, household characteristics, racial and ethnic minority status, housing type, and transportation for that and other state census tracts.
75
Figure 1. Point in Time Estimate of Homelessness, Delaware, 20227
CIRCUMSTANCES LEADING TO HOMELESSNESS
The most common circumstances that can lead to homelessness include lack of affordable housing, financial crises such as unemployment, underemployment and low wages, and domestic violence.1,2,8,11,15 Deficits in any of the social determinants, compounded with homelessness, can result in complications from poor nutrition due to food insecurity and malnutrition, mental health issues including depression, high rates of substance use disorders, chronic diseases such as hypertension, and in the worst instances, even premature death.1,3,11 Housing instability can also adversely affect physical health and make it difficult to access health care,1 though it is needed. Many Delawareans earning minimum wage often struggle to cover rent and other basic needs. In 2021, the fair market value of a Delaware two-bedroom apartment was $1,183 per month, meaning an employee would need a job earning at least $22.76 to afford the apartment.8 Comparatively, Delaware’s 2022 minimum wage is $10.50, equating to the affordability of a $546 per month rental for an employee working full time.8 A one-bedroom unit at fair market value in Delaware averages $972, and a studio, $874, both options that could lead to housing instability and potential homelessness.8 Data found within MHC show that in 2020, 37.3% of Delaware renters were rent burdened.14 A study in New York indicated that chronic disease is more common among persons who are newly homeless than the general population.1
Lack of affordable housing can lead to overcrowding which may adversely affect mental health, stress, and sleep and increase the risk of close-contact infectious diseases.1 According to Housing Alliance Delaware, there is a shortage of more than 18,000 affordable and available rentals for extremely low-income Delawareans and only 8,282 affordable and available rentals that meet the needs of that vulnerable population.8 Without an available reliable address to receive sensitive personal documents, homeless people face barriers when applying for aid and services such as opening a bank account, registering to vote, or requesting required documentation for gainful employment. Having a post office box or general delivery are not uniformly accepted, posing additional hurdles.
YOUTH HOMELESSNESS
Youth homelessness has many factors, including runaway youths, families putting youths out of their homes, family poverty, and youths who become homeless due to a lack of resources as they are discharged from state programs such as foster care as they age out.2,3 Youths run away from home because of family conflict, home instability due to alcohol or drug addiction of a family member or someone living in the home, and physical abuse by a family member or someone living there. Once a youth is homeless, they are at risk of their essential needs not being met. They may lose access to food, clothing, quality education and have difficulty in school.3 Having a grumbling belly, sleeping on a different couch every night or in an abandoned car, and wondering how to shower before school the next day eclipses homework. Not all homeless youth stay in shelters. Some youths are abandoned in hospitals, sleep in tents, or huddled in corners on sidewalks with little
to no access to clean water or clean clothes. This can result in school absenteeism due to bullying or embarrassment. Between 2018-2021, data collected by school districts showed that 37% of students experiencing homelessness were reported as chronically absent – missing 10% or more of school attendance days and enrolled for at least ten days.16 In the 2020-2021 school year, 66.4% of the 2,576 Delaware students who were homeless were also chronically absent, a percentage that has increased annually since the 2016-2017 school year and which was similarly impacted by COVID-19 as the number of homeless families with children increased.16
Students experiencing homelessness may not finish high school.3 This may hinder their ability to find a job and affordable housing, propelling them into chronic homelessness. Such dire straits lead to adverse health outcomes, including obesity, substance use, and unintentional injury.12 With less education, youth may not be able to understand health information, have increased health risks, and be unable to make informed health decisions.12 Homeless youth without additional resources may not have access to quality health care. These can lead to poor health outcomes for youth. Adverse childhood experiences (ACEs), a Delaware School Survey (DSS) measure, include homelessness as a trauma.17 In addition to the trauma of homelessness or home insecurity, homeless youth may also face post-traumatic stress disorder, high rates of depression, thoughts of suicide, and substance use disorders.3,17 These issues may be co-occurring and compounded by the stressors of family, school, mental health, and other common risks associated with homelessness, including lack of basic safety.2,3,5,17 In the 2021 DSS, 1% of eighth-grade students and less than 30 individual eleventh-grade students confirmed that they had experienced homelessness or instability in their housing in the past 30 days.17 In the same survey, 22% of eighth-grade students and 21% of eleventh-grade students reported ever seeing or hearing violence between adults in the home.17 The DSS report includes additional collected data on individual ACEs indicators that align with the common causes that can lead youth to homelessness. A review of available data revealed a study that found that street youth experiencing homelessness have higher risks of mortality than general youth and that most deaths are caused by suicide or substance use.2
As a minority population, youth who identify as Lesbian, Gay, Bisexual, Transgender, Queer, and others (LGBTQ+) are disproportionately affected by homelessness.3,5 In Delaware, there is a gap in data on this subpopulation. To address this data concern, the Delaware Division of Public Health’s (DPH) Bureau of Health Equity is contracting with community partners to estimate the number of Delaware youth who have experienced or are at risk for homelessness, those that identify as LGBTQ+ within that group, and an informed guide to assessing the needs of this vulnerable population. Additionally, in this issue of the Delaware Journal of Public Health, there is an analytic essay on this topic titled LGBTQ+ Youth Homelessness in Delaware: Building a Case for Targeted Surveillance and Assessment of LGBTQ+ Youth Needs and Experiences. LGBTQ+ youths are more likely to experience homelessness in a single year than youth who identify as heterosexual or cisgender.3 LGBTQ+ youths face the same
76 Delaware Journal of Public Health - June 2023
common contributing factors as other homeless youth, including family conflict, domestic violence, and physical abuse.1–3 LGBTQ+ youths also face the possibility of family rejection, sexual abuse by a family member or someone living in the home, and being asked to leave their homes because of their sexual orientation, gender identity, or gender expression.2,3 LGBTQ+ youths also suffer higher rates of school bullying and violence.12 Homeless LGBTQ+ youths and youth in foster care are particularly vulnerable. According to one study, homeless LGBTQ+ youths reported higher levels of victimization, including being physically abused, raped, beaten, or other assaults.3 These additional distresses can lead to mental health disorders atop the risk for poor health outcomes due to physical traumas and deficits in the social determinants.5 National survey data indicate that about 20% of homeless youth identify as LGBT.3 The secondary DSS reported that 3% of eighth and eleventh-grade students self-identified as gay or lesbian and 12% and 13% as bisexual, respectively.17 In the same survey, 4% of eighth-grade students self-identified as “other” and 7% were unsure, while 3% of eleventh-grade students self-identified as “other” and 4% were unsure.17
In the review of reported U.S. Department of Education data, in the 2019-2020 and 2020-2021 school years, Hispanic/Latino students predominately experienced homelessness among their enrolled ungraded, 3- to 5-year-olds and kindergarten to grade 13 peers.9 For Delaware however, students identifying as Black or African American made up 54.7% (1,409) of the homeless enrolled student population in the 2020-2021 school year.9 Please note: a limitation/challenge in comparing data for homeless youth is found in the definition used for youth in different sources. Some research does not delineate youth from those unaccompanied, without a parent or guardian or family member. Those within a family and others define homeless youth to include persons as old as 25, including college students as unaccompanied homeless youth. For this article, unaccompanied youth refers to minors up to and including the age of 18 if they are still in foster care.1–3,5,7,8,17 Further, not all data is provided for all years. States began reporting race and ethnicity data of students experiencing homelessness in the 2019-2020 school year, but not all states were able to report the data.9
DOMESTIC VIOLENCE AND HOMELESSNESS
Domestic violence contributes to youth homelessness and is a primary cause among families with children, especially women.18 Reported by the National Coalition for the Homeless, 80% of women experiencing homelessness with children were previously victims of domestic violence.2 Domestic violence can include intimate partner violence, stalking, elder abuse, sexual abuse, child abuse, and physical or economic abuse. It usually occurs in a family or domestic setting when a person holds power over another person.1 In Delaware fiscal year 2022, over 3,350 calls were made to domestic violence hotlines, a slight increase from 2021.19 Adult survivors of sexual abuse, intimate partner violence, physical abuse, and elder abuse are the reference for this essay. Survivors of domestic violence may experience homelessness multiple times, with or without children. Persons with children in domestic violence
relationships often choose between continuing to live in an unsafe, abusive environment or homelessness. According to the Domestic Violence Coordinating Council, in the 2022 fiscal year, children were present for 38.9%, or 4,160, of the criminal domestic violence incidents in Delaware.19 Survivors leaving abusive situations with children must consider if there is a chance that they will be separated from their children due to shelter policies or if their children will be removed from their care and placed in foster care.2 They may stay in abusive relationships to ensure shelter for their children and themselves. Forty-five percent of domestic violence survivors report staying with abusive partners because they had nowhere else to go.2 To flee, survivors need the opportunity away from abusers to access resources for help, including relocating to shelters. Delaware survivors of domestic violence would have also faced an increased likelihood of violence due to stay-athome orders and increased barriers to prevention and help. Domestic violence survivors face additional hardships when overcoming homelessness, especially if children are involved. Healing is emotional and mental and may be physical and economical. Reported intimate partner criminal incidents in Delaware decreased for the last five fiscal years, 2018 to 2022, but there were still 935 reports where physical injury occurred to the intimate partner victim.19 Coming out of the COVID-19 pandemic, where mixed reports showed domestic and intimate partner violence rates both increased and decreased, some survivors reported that they did not seek help or report abuse during the stay-at-home period while confined with their abusers. That resulted for some in social and psychological consequences, even post-traumatic stress symptoms, in addition to the physical symptoms.19,20 These health consequences can co-occur with housing instability and homelessness when trying to leave and recover from abusive relationships. Intimate partner and sexual violence can lead to unplanned pregnancies, resulting in economic hardships, mental stress and depression, and sexual and reproductive health issues.19 Mental stress and depression were evidenced in one study that found one-third of mothers experiencing homelessness attempted suicide at least once, compared to onequarter of housed and poor mothers.2
As a result of domestic violence, some survivors may have unfavorable employment histories due to their abuse, making it difficult for them to find employment.18 Consequently, finding affordable housing or landlords willing to rent to survivors may be more challenging, especially if there are records of eviction or eviction due to domestic violence.1,18 Survivors with children who choose to leave an abusive and unsafe situation must find affordable housing but may not be financially stable. Domestic violence claims made up 23.5% of claims totaling $624,300.36 in Delaware’s Victim’s Compensation Assistance Program received in fiscal year 2022.19 Compounding health consequences with one or multiple deficits in the social determinants can make it that much more challenging for a survivor of domestic violence experiencing homelessness. During the 2022 fiscal year, 1,009 individuals were sheltered in Delaware, an increase from before males were included in the count in 2016.20 Of those 1,009 individuals, 20 identified as male, 511 identified as female, and 478 were children. Although resources exist this shows that the full need is yet unmet.19
77
HOMELESSNESS RESOURCES IN DELAWARE
The Delaware Department of Health and Social Services, DPH, and many community-based organizations and coalitions are working towards improving health risks by addressing the SDoH and disparities Delawareans experiencing homelessness face. DPH’s MHC platform is a powerful tool that is regularly updated with indicators related to community health that link community priorities to social determinants.14 Among those community-based organizations galvanized around health disparities are the1:
• Housing Alliance Delaware, which is the lead agency for the Delaware Continuum of Care and addresses the need for affordable housing8;
• Delaware Racial Justice Collaborative, which collaborates on the Equity Counts Data Center and advocates to eliminate inequitable policies14;
• United Way of Delaware, which connects people to emergency assistance and resources; and
• Better Homes of Seaford, which provides safe, affordable housing in its community. Three programs provide evidence-based intervention services comprising hotlines, counseling, case management, and foster care support as well as shelters for homeless adults, with or without children:
• Child, Inc., whose domestic violence shelters are in confidential locations19;
• People’s Place II, which has emergency shelters in Kent and Sussex counties19; and
• The Springboard Collaborative, which recently opened the 40-unit Springboard Pallet Village in Georgetown.21
An additional adult resource, Casa San Francisco in Milton, provides an emergency shelter and food pantry in the county where a high percentage of homeless persons sleep as of 2021.8 One in three homeless Delawareans lived in Sussex County in 2021 and 2022.8,21 And, West End Neighborhood House in Wilmington offers housing for homeless LGBTQ+ youth over 18. In October 2018, the Advisory Committee on Immunization Practices recommended that all persons one year or older experiencing homelessness be routinely immunized against hepatitis A.4 Since then, DPH has offered hepatitis A vaccinations to the Delaware homeless population at shelters, organizations providing transitional housing, and outpatient facilities.4 Additional resources for persons experiencing homelessness include the seven public libraries that offer reservable kiosks where patrons can use high-speed internet and an iPad for private, wheelchair-accessible video and audio telehealth appointments, interviews, job training, education, and social service and legal appointments. To help with barriers to protected data, anyone born in Delaware can obtain a Delaware birth certificate with valid government or state-issued photo identification and payment. Also, when applying for assistance through DE ASSIST, those without a permanent address are permitted to use the address of any Delaware State Service Center and enter “N/A” for housing and utility expense information, then explain why during their interview.
As a result of the pandemic, in 2022 DSSC provided housing vouchers for hotels or motels to over 1,000 people, a significant increase from the 50 persons prior to the relief program.8 The Delaware public health emergency ended on May 11, 2023. The emergency expansion and federal waivers of several programs were discontinued, such as the DSSC’s pandemic relief program, which ended October 1, 2022,8 expanded Supplemental Nutrition Assistance Program benefits, which ended April 1, 2023, and Medicaid continuous enrollment, which ended March 31, 2023; the federal student loan pause is expected to end in the summer of 2023. The impact of the loss of these programs on the Delaware homeless population and those relying upon those benefits who were home insecure is yet unknown. Even before the pandemic, persons experiencing homelessness in Delaware existed, and data tell the story that the resources provided, such as shelters, weren’t enough.
LIMITATIONS
Homelessness data is not perfect, and gaps in data exist. The CoC Point-in-Time Count estimates include data from unsheltered persons on a single night annually, except during the COVID-19 pandemic. Per the 2021 Point-in-Time Count, not all CoCs performed counts, including Delaware.6 In 2022, some counts were delayed and were taken when some shelters were not open to persons experiencing homelessness due to warmer weather.7 Data about homeless youth is primarily collected and reported by departments of education, but only if the youth are enrolled in public school.9,17 Further, because homeless youth may attend more than one school in a school year, the data reported may contain duplicates when more than one school reports the same student.17 Inconsistent definitions of youth, unaccompanied youth, and young adults across research methodologies may cause other inaccuracies or gaps.
REDUCING HOMELESSNESS IN DELAWARE
The first step towards purging involuntary homelessness in Delaware is creating a defined state plan that includes passing legislation and policies supporting this vulnerable population, such as the Homeless Bill of Rights. Connecticut, Illinois, Puerto Rico, Rhode Island, Baltimore, Maryland, Duluth, Minnesota, and Madison, Wisconsin, have passed legislation for their homeless populations.2 2023 House Bill 55 is one of several attempts at passing a Bill of Rights in Delaware to address inequities and disparities facing Delaware’s vulnerable homeless population, but it cannot be counted as a resource until legislation is passed.13
The plan should present impactful steps to make Delaware a homelessness-free state by increasing affordable housing to meet the needs of the extremely low-income workforce, setting a livable wage that allows families to pay fair market value for rent at 30% or less of their income, and designating funding for initiatives similar to Springboard Pallet Village or West End Neighborhood House’s Life Lines Housing and resources for LGBTQ+ persons. The plan should provide more resources for community-based programs that offer pathways for economic stability for both older teens and adults without creating additional barriers, such as the goals of the proposed Family Justice Centers. Another step in the plan is to include a call for additional funding to permanently increase the capacity of shelters to meet the number of those counted as unsheltered. Ongoing surveillance of home-insecure
78 Delaware Journal of Public Health - June 2023
and homeless youth of all ages and subpopulations should be included to better fill the gap in data and address the needs of youth. Finally, since the need may only be made known if the ask is made, it can become the clinical standard to complete a SDoH screening for every patient, known homeless or not, using validated tools that incorporate questions about food, safety, and housing insecurity. Homeless and home-insecure patients can then be connected to assistance and available resources in an upstream and proactive manner.
CONCLUSION
Homelessness must be a public health and community priority in Delaware. The data show that although resources exist and groups are tackling the issue, we must continually evaluate Delaware’s homelessness and home insecurity landscape compared to the community’s needs. It is necessary to determine why homelessness predominately affects certain groups more than others and where and why disparities persist despite the resources aimed to fight them. Once we understand the whys, we must swiftly address them across all the social determinants because the consequences and cost of those inequities are lives. By prioritizing resources using a racially, ethnically, and gender-unbiased health equity lens, we can reduce and hopefully eliminate health inequities linked to homelessness and the number of those disproportionately affected by it.1–4,7,8,10,15 Ms. Rent may be contacted at sequoia.d.rent@delaware.gov.
REFERENCES
1. U.S. Department of Health and Human Services. (n.d.). Housing instability. Housing Instability - Healthy People 2030. Retrieved from: https://health.gov/healthypeople/priority-areas/social-determinantshealth/literature-summaries/housing-instability
2. National Coalition for the Homeless. (2022). Issues. National Coalition for the Homeless. Retrieved March 1, 2023, from: https://nationalhomeless.org/homelessness-in-the-us/research-by-topic/
3. United States Interagency Council on Homelessness. (2018). Homelessness in America: Focus on youth. Retrieved from: https://www.usich.gov/resources/uploads/asset_library/Homelessness_ in_America_Youth.pdf
4. Talbott, J., & Hess, P. (2019, May 28). Delaware faces immunization challenges head-on. Delaware Journal of Public Health, 5(2), 6–10. Retrieved from: https://djph.org/wp-content/uploads/2021/07/djph-52-003.pdf https://doi.org/10.32481/djph.2019.05.003
5 Wang, J. Z., Mott, S., Magwood, O., Mathew, C., Mclellan, A., Kpade, V., Andermann, A. (2019, November 14). The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: A systematic review. BMC Public Health, 19(1), 1528. https://doi.org/10.1186/s12889-019-7856-0
6. U.S Department of Housing and Urban Development. (2023, February). 2007-2022 Point in time estimates by state. Washington; https://view.officeapps.live.com/op/view. aspx?src=https%3A%2F%2Fwww.huduser.gov%2Fportal%2Fsite s%2Fdefault%2Ffiles%2Fxls%2F2007-2022-PIT-Counts-by-State. xlsx&wdOrigin=BROWSELINK
7. U.S. Department of Housing and Urban Development. (2022, December). The 2022 Annual Homelessness Assessment Report (AHAR) to Congress, 18, 40, 52, 94). Washington; https://www.huduser.gov/portal/sites/default/files/pdf/2022-AHAR-Part-1.pdf
8. Housing Alliance Delaware. (2022). Housing and omelessness in Delaware. Retrieved from: https://www.housingalliancede.org/_files/ ugd/9b0471_322d16c2158c4ab09743a897dc12aa6d.pdf
9 National Center for Homeless Education. (2022). Student homelessness in America: school years 2018-19 to 2020-2021. Retrieved from: https://nche.ed.gov/wp-content/uploads/2022/11/StudentHomelessness-in-America-2022.pdf
10. Willison, C., Unwala, N., Singer, P. M., Creedon, T. B., Mullin, B., & Cook, B. L. (2023, February 16). Persistent disparities: Trends in rates of sheltered homelessness across demographic subgroups in the USA. Journal of Racial and Ethnic Health Disparities, 1–13 https://doi.org/10.1007/s40615-023-01521-9
11 Office of Readiness and Response. (2022, May 6). About homelessness. Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/orr/science/homelessness/about.html
12 Centers for Disease Control and Prevention. (2020, Nov). Health disparities. Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/healthyyouth/disparities/index.htm
13. State of Delaware. (2023). An act to amend TITLE 6 and TITLE 31 of the Delaware code relating to individuals who are homeless, legislation document. Retrieved from: https://legis.delaware.gov/json/BillDetail/
79
LGBTQ+ Youth Homelessness in Delaware: Building a Case for Targeted Surveillance and Assessment of LGBTQ+ Youth Needs and Experiences
Mary Louise Mitsdarffer, Ph.D., M.P.H.
Assistant Professor, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
Rebecca McColl, M.A.
Associate Policy Scientist, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
Erin Nescott, M.S.
Associate Policy Scientist, Center for Community Research & Service, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
Jim Bianchetta President, Wilmington/Northern Delaware PFLAG
Eric K. Layland, Ph.D.
Assistant Professor, Department of Human Development and Family Sciences, University of Delaware
Tibor Tóth, Ph.D.
Assistant Professor, Joseph R. Biden, Jr. School of Public Policy and Administration, University of Delaware
ABSTRACT
Objective: In this article, we examine the issue of LGBTQ+ youth homelessness in Delaware, summarize current services available and prior research work that has been done, examining the number, needs, and experiences of unaccompanied unhoused LGBTQ+ youth. Methods: We provide a literature review detailing risks associated with LGBTQ+ youth homelessness, resources available, and prior studies and surveys examining this population. Results: LGBTQ+ youth experiencing homelessness are particularly vulnerable to physical and mental health challenges, abuse, and violence. The unique needs of this population necessitate specialized resources, yet there are a limited number of such resources available in Delaware and a dearth of information on youth homelessness in general, including LGBTQ+ youth. For example, administrative barriers exist for unaccompanied queer youth seeking shelter services, such as need for legal identification or being grouped in shelter populations based on sex assigned at birth rather than gender identity. Exposure to unsafe environments is a general problem for queer youth. This can make public spaces feel unsafe and increase risk of physical or mental harm, mistreatment, or abuse when seeking shelter outside of agency services and resources. In order to accurately identify and appropriately serve this population, additional research is necessary. Conclusions: Evidence building is a critical first step in creating an effective study to examine the issue of LGBTQ+ youth homelessness in Delaware. With the evidence acquired in our literature review our next step to establish an informed methodology is to hold service provider and LGBTQ+ lived experience focus groups. Through a qualitative approach we aim to learn how to appropriately utilize the quantitative tools identified in our analysis and to assess what questions are missing to advance the needs of this population.
INTRODUCTION
Lesbian, gay, bisexual, transgender, and queer (LGBTQ+) youth compose an estimated 20-40% of youth experiencing homelessness (ages 13-24) in the United States, despite only representing 10-15% of the youth population.1 While some social services are available to aid unhoused youth, there is not a clear picture of what resources exist at state and local levels to address housing instability and homelessness among LGBTQ+ youth. Moreover, even less is understood about how youth learn about such services, how they access them, if they are meeting the needs of the youth population—and importantly—how systemic inequities influence disparities in LGBTQ+ youth service utilization at local levels.
A study of the nature and extent of this problem, including an assessment of the number of LGBTQ+ youth experiencing
homelessness in Delaware (DE), has not been undertaken. In response, this work aims to lay a foundation for assessing the true number of LGBTQ+ youth experiencing, or at risk of experiencing, homelessness, and the scope of need of this population. As the first step for adequately measuring these factors, here we draw upon past research, existing survey tools, and a basic inventory of DE-specific resources to establish an informed approach for future methodology aimed at enumerating the number of queer youth experiencing homelessness in DE and their needs.
The article is laid out as follows: first we provide a definition for homelessness, how we define unaccompanied LGBTQ+ youth, and current estimates of the number of youth experiencing homelessness in DE. The next section briefly explores risks associated with experiencing homeless for queer youth and
80 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.014
structural inequities that influence social service utilization. Then, we offer examples of past efforts to quantify and further understand LGBTQ+ youth homelessness in the United States. Next we explore services and resources available to LGBTQ+ youth throughout the state of Delaware. We finish by offering insights into how this review could support future work throughout the state.
COUNTING AND DEFINING HOMELESSNESS AND UNACCOMPANIED LGBTQ+ YOUTH
The U.S. Department of Education classifies homelessness as: “individuals who lack a fixed, regular, and adequate nighttime residence,”2 which includes those residing in shelters, hotels, cars, vacant buildings, and on the streets as well as couch surfers (i.e., those that may stay temporarily in a series of other people’s homes, typically by sleeping on their couches).1 Data from Delaware’s Point in Time Count (PIT) of the homeless population estimates the number of sheltered and unsheltered people experiencing homelessness on a single night in January each year.3 PIT measurements are presently some of the best and longest running estimates of those experiencing homelessness and unstable housing throughout the state. For example, over the course of the COVID-19 pandemic, from 2019 to 2022, it is estimated that the number of homeless individuals throughout the state doubled, and tripled in some cases, composed of approximately 392 families with children, 769 children under the age of 18, and 200 young adults ages 18-24.4 In addition to the PIT measures, the U.S. Department of Education (DOE), through the McKinney-Vento Homeless Education Assistance Improvement Act of 2001, which is explored more in subsequent sections, also maintains counts of unhoused youth accessing public education in a given state in a given year through the National Center for Homeless Education (NCHE).5 Delaware’s 43 Local Education Agencies report the number of unhoused students in their respective district and also subgroups of children with disabilities, those with limited English proficiency, migratory youth, and unaccompanied homeless youth.5 As a result, NCHE counts are higher than PIT numbers due to varying definitions of homelessness. The NCHE estimates that there were 2,576 enrolled students experiencing homeless in DE in the 2020-21 school year—and an estimated 265 were unaccompanied youth.5 However, it is unclear which measure is most accurate. Nevertheless, in a state like Delaware with a population of less than a million people these rates are cause for concern.
Factors associated with experiencing homelessness in youth vary. Therefore, it is important to note that not all LGBTQ+ youth encounter homelessness due to familial rejection or abuse, some encounter it due to household factors, like economic instability, that cause the whole family to lose housing. A recent scholarly review cites that the leading causes of persistent homelessness among adults were linked to substance abuse, domestic violence, and mental illness.6 However, our analysis focuses on unaccompanied LGBTQ+ youth—those not residing with family members, parents, or guardians – ages 13-24.
Finally, we strategically use the terms LGBTQ+ or queer interchangeably throughout our article as umbrella terms to refer to lesbian, gay, bisexual, transgender, and queer individuals.
LGBTQ+ YOUTH EXPERIENCING HOMELESS, RISKS FACTORS, AND SOCIAL SERVICE UTILIZATION
LGBTQ+ youth are coming out at younger ages than in previous generations, more and more in adolescence and early adulthood,7,8 potentially reflecting shifts in societal acceptance and attitudes toward LGBTQ+ people.9,10 However, societal acceptance does not merit familial approval or that queer youth feel safe in their households. Therefore, despite positive shifts in contemporary society, LGBTQ+ youth have greater odds of running away from home.11 Queer unhoused youth report incidences of familial conflict, abuse, rejection, neglect, and lack of acceptance of sexual orientation or gender identity9,12 as facilitating factors for leaving their family home.13,14
Among queer youth, 28% report experiencing homelessness or housing instability at some point in their lives15 and experience elevated incidences of victimization associated with being unhoused including incidences of prejudice, mistreatment, and exploitation.16 LGBTQ+ youth are more likely to experience unaccompanied incidences of homelessness and have longer periods of homelessness when compared to their non-LGBTQ peers.14,17 Moreover, LGBTQ youth who reported housing instability or homelessness have greater odds of reporting depression, anxiety, self-harm, considering suicide, and attempting suicide compared to those who did not report any housing instability.13–15
When LGBTQ+ youth are unable to reside in their family homes or lack safe places to live, their most commonly cited need is housing.14 Social barriers exist to utilizing housing services as many agencies have cissexist heteronormative policies that contribute to LGBTQ+ anxieties.18 Research finds that LGBTQ+ individuals are more likely to seek out services like mental health care support than their cisgender heterosexual peers,19 but access to services is uniquely challenging for LGBTQ+ youth, due in part, to cissexist heteronormative structures embedded in administrative protocols.1
Such dichotomies indicate inherent structural inequities in social service utilization, meaning that disparities in access are likely more the product of administrative barriers to accessing services and not so much due to individual motivations. For example, housing services —like shelters —are often segregated based on population age and sex. They require individuals to fill out intake forms or to show legal forms of identification in order to gain admittance. For trans and non-binary people in particular, filling out such administrative forms or sharing legal identification (ID) that reflect their sex assigned at birth rather than how they identify can be distressing.20 However, making necessary changes to government issued IDs—like driver’s licenses and state IDs–is often impeded by state policies and politics. Indeed, in Delaware, compared to its surrounding states of Pennsylvania, New Jersey, and Maryland, provider certification is required to make changes to gender markers on driver’s licenses, and policy does not allow individuals to have gender markers outside of the male/female binary.21 Without proper ID, service organizations may not accept individual’s gender identity, especially when identification reflects dead names (i.e., names given at birth no longer used by trans people) and sex assigned at birth. As a result, trans people may either be denied access or placed with a population that is
81
unsafe or traumatizing to them. According to a report produced by Canavan & Ledger,22 30% of trans people reported being turned away from a shelter due to their gender identity and 22% reported being sexually assaulted by fellow shelter residents or staff,22 trans girls and women disproportionately experience assaults and violence.23
Exposure to unsafe environments are a more general problem for queer youth living without agency services and resources, or stable housing for reasons as diverse as gentrification, street violence, and police harassment.18 This can make public spaces feel unsafe, resulting in avoidance of well lit, heavily populated places. In turn they increase their risk of physical harm, mistreatment, or abuse when seeking out places off the beaten path, like squats or unoccupied housing.1 It is estimated that 48% of LGBTQ+ youth have stress around finding a place to sleep at night.13 Moreover, research indicates that homeless LGBTQ+ young people have an increased likelihood of mental health problems and engaging in risky behaviors,1.such as substance use and survival sex,24 which are linked to increased incidences of negative health outcomes like HIV infection.1,25 As a prerequisite to adequately serving this population, we need to have accurate assessments of the number and needs of LGBTQ+ youth experiencing homelessness.
PAST SURVEY WORK ON LGBTQ+ YOUTH EXPERIENCING HOMELESSNESS
There have been several national surveys examining the experiences of both young people and service providers. Across these tools, common practices include measuring the number of youths that are unhoused; collecting demographic information, health indicators, and histories of social service utilization; and acknowledging barriers to data collection, which are often marked by hard-to-reach populations and small sample sizes. Here we offer examples of surveys designed to collect inclusive information and accounts of youth’s experiences of homelessness across multiple states and communities.
Research, Education and Advocacy Co-Lab for Youth Stability and Thriving (REALYST) is a national research collaborative examining homelessness among young people aged 18 to 26 across seven major U.S. cities.26 REALYST collaborators acknowledged that due to small sample sizes of LGBTQ+ youth experiencing homelessness, it is difficult to parse out a comprehensive, contemporary understanding of the range of experiences of young people and their day to day lives.27 To address this need, REALYST’s Homeless Youth Risk and Resiliency Survey (HYRSS) captured the experiences of over 400 LGBTQ+ young adults between 2016 and 2017, gathering data on demographics, encounters with homelessness, and experiences with stress and discrimination.27 HRYSS assessed risk and protective factors concerning sexual health behaviors, mental health, technology and social media use, education, substance use, homelessness history, reproductive health, foster care history, criminal justice history, employment, adverse childhood experiences, victimization on the streets, coping, discrimination, and stress.21 With these rich data, REALYST researchers were able to contrast differences in geographic locations to gauge variation in queer youth’s experiences of homelessness across cities and communities. For example, researchers were able to assess the role social media plays in unhoused queer populations and the
association between online interactions and youth’s decisions to engage in risk or protective behaviors.27 Which in turn holds major implications for how service organizations can design communication strategies around information dissemination and housing and health interventions. Moreover, the REALYST collaboration exemplifies how multiple research teams can create meaningful sample sizes and rich data by using matching survey tools across communities.
Voices of Youth Count (VoYC) is another initiative dedicated to capturing the experiences of queer unhoused youth. This national research initiative has four primary research activities designed to generate a more complete understanding of youth homelessness in the US—which includes counts and surveys.17 For example, VoYC has offered the VoYC Conducting a Youth Count: A Toolkit since 2018, which offers a 5-phase roadmap to conduct an inclusive youth count of the homeless population in a given community or state. Phases 1-3 focus on organizing a team of collaborators, trainings, and conducting focus groups and phase 5 focuses on data analysis and dissemination.28 Phase 4 is of particular interest as it provides steps, procedures, and tools to conduct actual counts of the youth homeless population in a given locality. Phase 4 employs a two-pronged approach: a street count guide for harder to reach populations that may be unwilling to be surveyed and the VoYC Brief Survey The VoYC Brief Survey is a handy tool as it is purposely short—with a total of 16 questions on a single page—which may circumvent barriers associated with long, tasking surveys. The survey asks participants for demographic information, their initials instead of names, where they slept the previous night, education information, access to public benefits, foster care participation, histories of incarceration, whether they are pregnant or are a parent, and their sexual and gender identities,28 allowing for an inclusive snapshot of youth experiencing homelessness.
VoYC also employed a national survey conducted in 2016 to estimate the incidence, prevalence of, and needs of unaccompanied youth experiencing homelessness -- resulting in a brief entitled Missed Opportunities: LGBTQ Youth Homelessness in America 17 In this work, researchers surveyed 26,161 adults whose households had LGBTQ+ youth (ages 13-25) with histories of homelessness as well as queer respondents (ages 18-25) with histories of homelessness.29 Collecting data by proxy, or by asking parents/guardians about their children and their lived experiences or asking individuals to recall past experiences in childhood is helpful as it allows researchers to circumvent institutional review boards’(or university ethics committees) lengthy approval periods associated with surveying protected classes, like those under the age of 18.29 However, such strategies conflict with best practices recommended for reaching LGBTQ youth. That is, parental accounts or permissions often act as a barrier to the sexual, and presumably gender, minority participation in data collection and may create secondary narratives that are biased to the realities of LGBTQ+ youth.30 However, secondary accounts and recalling past experience, while not ideal, do provide insights into facilitating factors of unaccompanied youth homelessness and past lived experiences.
Similarly, surveys that utilize the expertise of service providers help to unpack the needs and experiences of queer unhoused youth. Executing surveys at the provider level offers alternative avenues to data collection and insights to the diverse needs of
82 Delaware Journal of Public Health - June 2023
this community as practitioners work with many youths in a variety of situations. For example, The True Colors Fund, in Partnership with the Williams Institute, gathered data from 138 youth homelessness service providers for the 2014 LGBTQ Homeless Youth Provider Survey. 14 In this survey, providers reported information regarding the demographics, needs, and experiences of their clientele and reported on their own programs by detailing staff demographics and training, and barriers and successes to serving queer youth.14 Findings indicate that over half of providers surveyed reported that they do not have dedicated LGBTQ staff, and providers cited lack of funding, community support, partnerships, and training as barriers to appropriately serving this population.14
In addition to homelessness-specific surveys, numerous organizations have performed surveys examining other aspects of this population, data from which we can glean further insight into disparities faced by queer youth across social service systems beyond housing. GLSEN, a national network of educators, students, and local chapters committed to safe, supportive, and inclusive K-12 education for LGBTQ+ youth, performs the GLSEN School Climate Survey bi-annually to gather data on LGBTQ+ youth in schools.31 The Trevor Project, an American nonprofit organization focused on suicide prevention efforts for queer youth, conducts the National Survey on LGBTQ Youth Mental Health annually since 2019. The survey captures insights into novel risks LGBTQ+ youth face, barriers to mental health service use, and recently, the impacts of COVID-19 and antitransgender legislation on queer youth, with nearly 34,000 respondents in 2022.15
There are also ongoing efforts to gather information on the lives of those that specifically identify as non-binary or transgender. The National Center for Transgender Equality, beginning in 2015 and surveyed again in 2022, launched the U.S. Transgender Survey (USTS), which is the largest survey devoted to the lives and experiences of transgender people residing in the U.S.21 USTS focuses on the experiences of trans people across systems (i.e., education, employment, health, housing, and law enforcement and the carceral system).32 Results from the 2015 survey, which surveyed over 27,000 trans respondents, indicate that trans people face pervasive verbal, physical, and sexual violence in their lives in nearly every domain studied.32 In terms of housing, 30% of respondents indicated that they had experienced homelessness at some point in their life due to their gender identity and 12% indicated that they had been unhoused in the year prior to taking the USTS.32 Such results showcase how disparities in health and economic position permeate across systems due to individuals gender and sexual identities.
The United States government also makes efforts to collect data on the experiences of young people and have made small strides into becoming more inclusive of sexual minorities. For instance, the Centers for Disease Control and Prevention created the Youth Risk Behavior Surveillance System (YRBSS) in 1990 to biennially monitor behaviors that contribute to unintentional injuries and violence, unintended pregnancy and sexually transmitted diseases, alcohol and substance use, dietary behaviors, and physical activity levels among representative samples of 9-12th grade students nationwide.33,34 Notably in 2015 the YRBSS began to ask two questions on sexual identity, but as of 2022 still did not ask questions regarding youth gender identity. The YRBSS publishes reports specifically on the experiences of LGBTQ+
students, risk behaviors, and health outcomes, however, findings are limited as they do not consider non-binary and trans youth. National and local surveys are powerful tools. They highlight not only the number and needs of LGBTQ+ youth experiencing homelessness, but also the importance of spaces that offer acceptance of social identity, affirmation of individualism and emotional support. The True Color Fund’s 2014 LGBTQ Homeless Youth Provider Survey found that after housing support, acceptance and social support were the next highest needs identified by service providers for queer youth.14 Therefore, the next section defines and explores inclusive social services and programs afforded to unhoused queer youth throughout Delaware and the country as a whole.
SERVICES AVAILABLE TO LGBTQ+ YOUTH EXPERIENCING HOMELESSNESS
Homeless agencies and services refer to “public, communitybased organizations dedicated or universal, specialized or not, involved in activities related to the homeless population…. they are considered inclusive if they offer safe and stable accommodations for LGBTQ+ youth.”18 Currently, there are few organizations in Delaware specifically that meet these criteria and provide care for LGBTQ+ youth experiencing homelessness. Among these is West End Neighborhood House’s Life Lines Program which offers support to young people identifying as LGBTQ+, youth in foster care, and unaccompanied youth. Life Lines provides intensive case management including housing support, mental health services, employment placement assistance, and more.35 Supporting the mission of West End Neighborhood House is the Delaware LGBTQ+ Housing Safeguard Committee. This committee is comprised of Delaware organizations committed to examining the current issue of LGBTQ+ youth homelessness in the state and supporting those who are experiencing or at risk of homelessness.36 Youth experiencing homelessness may also utilize resources that are not LGBTQ+-specific such as the Housing Alliance Delaware, which provides a centralized intake program offering information and referrals to housing assistance and emergency shelter openings throughout the state.37
Across the state, there are several organizations connecting youth to resources and networks of their peers in order to meet social and emotional needs. Parents, Families, and Friends of Lesbians and Gays (PFLAG) chapters throughout Delaware support several youth support groups, including the Parents of Trans Kids Youth Group for young people ages 10 to 21 and the LGBTQ+ “ASK” Youth Group designed for middle and high school youth.36 Similarly, CAMP Rehoboth is a nonprofit organization with the goal of promoting community wellbeing and creating a positive and inclusive environment for people of all gender identities and sexual orientations. CAMP Rehoboth connects community members through events, education and outreach, fundraising, and providing political awareness.38 Finally, Lavender Programming Board, a studentrun organization at the University of Delaware that is open to the public, is dedicated to celebrating and connecting members of the LGBTQ+ community through meetings and social or informational events. By providing affirmative spaces and access to community resources, organizations such as these are critical to the social and emotional development of young people, especially those experiencing homelessness.
83
Together with local resources, national services and policies have the potential to provide additional support for youth experiencing homelessness, including targeted resources for LGBTQ+ and other minoritized youth. The Substance Abuse and Mental Health Services Administration has committed to providing specialized services through the 988 Suicide & Crisis LifeLine. Queer youth who use the 988 Life Line have the option of being connected with a specially trained, LGBTQ-competent mentor, providing potentially life-saving services for LGBTQ youth.15 On a policy level, the McKinney-Vento Homeless Education Assistance Improvement Act of 2001, was implemented to support families and children who may move out of districts due to experiences of homelessness or those that do not have a stable address. The act aimed to prevent disruptions in schooling and maintain a consistent school environment.1 McKinney-Vento assigns responsibility to schools to help provide transportation services, school supplies and uniforms to unhoused students.1 However, this policy has shortcomings when youth are unaccompanied and unhoused as the age of majority is 18 and enrollment in such programs may require parent or legal guardians.
DISCUSSION
In order to adequately count LGBTQ+ unhoused youth in Delaware and assess their needs, our next steps are informed by research on youth homelessness across the country – e.g., LGBTQ+ homelessness research projects and data collection strategies -- and identified limitations in LGBTQ+ homelessness resources. For example, REALYST and VoYC provide exemplary projects with possible templates for a statewide assessment of LGBTQ+ youth homelessness, where multiple strategies may be necessary for a surveillance of issues in both depth and breadth. For instance, VoYC’s Brief Survey achieved a brief understanding of queer youth’s social service utilization, identity, and needs through strategic data collection that included observations over time, confidential, deidentified data collection, discretion and privacy for participants, and resources for field-based street counting. The REALYST collective on the other hand has a more involved and lengthy survey to gauge the number, needs, and experiences of LGBTQ+ youth experiencing homelessness. Their findings offered researchers and community leaders’ evidence of youth awareness and use of services for people experiencing homelessness and possible intervention strategies. These surveys taken together garner new insights into the number and needs of the youth homeless population, specifically LGBTQ+ youth, through varying strategies in data collection- like a brief survey, field training guides, and metrics for anonymity—like the use of initials. Furthermore, our documentation of national and local Delaware support services not only provides potential entry points for connecting with LGBTQ+ youth and specific resources to investigate service utilization and awareness, but also an understanding of the current service landscape. Throughout this work, we note that not all housing services or social programs extend support to unhoused queer youth or offer sexual and/ or gender affirming support.18 We find that there are a limited number of service providers and organizations geared toward the LGBTQ+ population in DE and those that offer a safe place to land for such individuals may not have the resources or staff to support this population. Moreover, policy designed to provide
social services to enhance stability in childhood—like healthcare and education—do not consider unaccompanied youth and their needs. In the United States the age of majority is 18, thereby making unaccompanied youth ineligible for many services when a parent or guardian is not in their lives to provide support.
Finally, while the PIT and NCHE estimates offer an insight into the number of youth experiencing homelessness in DE, it is clear there is not an understanding of the true number of unaccompanied LGBTQ+ youth. Our analysis of existing work exemplifies that beyond enumeration, it is imperative to assess the scope of need of this population, especially as queer youth are exposed to greater risks to their physical, mental, and emotional health and personal well-being.13,14
Finally, when considering next steps for data collection and identifying priorities with queer youth in Delaware, research evidence provides impetus to also investigate precursors to LGBTQ+ youth homelessness (e.g., family rejection, childhood experiences of adversity), health correlates of homelessness (e.g., unhealthy substance use, mental health), and potentially elevated experiences of victimization and discrimination.
CONCLUSION
This brief literature review is the first, evidence-building process needed to gauge the number, needs, and experiences of unaccompanied unhoused LGBTQ+ youth in Delaware. We have identified past approaches in survey work and enumeration, but to truly understand if these approaches work with Delaware’s queer youth population – especially with Delaware’s large UrbanRural divide – we propose a series of informational focus groups. Focus groups should consist of LGBTQ+ individuals with lived experiences of homelessness in youth as well as service providers who may be privy to the unique needs of this population. We propose forming multiple groups throughout the state to address the varying topography of the Delaware and the resultant unique needs faced in different locations. Moreover, the focus groups would explore what we have learned in our review around facilitating factors to becoming an unaccompanied youth, lived experiences of being unhoused, how youth come to know about and access social services, and unmet needs and barriers to care. Through understandings provided by service providers as well as those with lived experiences, we will be able to determine which survey tools and questions are most appropriate to survey and count the number of LGBTQ+ youth experiencing homelessness throughout the state.
Dr. Mitsdarffer may be contacted at mmits@udel.edu
REFERENCES
1. Tierney, W. G., & Ward, J. D. (2017). Coming out and leaving home: A policy and research agenda for LGBT homeless students. Educational Researcher, 46(9), 498–507. https://doi.org/10.3102/0013189X17733964
2. Youth.Gov. (2023). Federal definitions. Retrieved from:
https://youth.gov/youth-topics/runaway-and-homeless-youth/federal-definitions
3 US Department of Housing and Urban Development. (2019). Point-in-Time Count and Housing Inventory Count. Retrieved from:
https://www.hud.gov/2019-point-in-time-estimates-of-homelessness-in-US
84 Delaware Journal of Public Health - June 2023
4 Barlow, J., Nescott, E., Galdamez, T., & Perez-Rivera, M. (2022). 2022 kids count in Delaware FOCUS on recovery from COVID-19. Retrieved from: https://udspace.udel.edu/items/b0722d28-ee53-4e75-ac89-4723ca3d9bf7
5. National Center for Homeless Education. (n.d.). Delaware. https://profiles.nche.seiservices.com/StateProfile.aspx?StateID=10
6 Zhao, E. (2023). The key factors contributing to the persistence of homelessness. International Journal of Development & World Ecology, 30(1), 1–5 https://doi.org/10.1080/13504509.2022.2120109
7 Quintana, N. S., Rosenthal, J., & Krehely, J. (2010). On the streets: The federal response to gay and transgender homeless youth. Washington, DC: Center for American Progress. Retrieved from: https://www.americanprogress.org/article/on-the-streets/
8 Bishop, M. D., Fish, J. N., Hammack, P. L., & Russell, S. T. (2020, November). Sexual identity development milestones in three generations of sexual minority people: A national probability sample. Developmental Psychology, 56(11), 2177–2193. https://doi.org/10.1037/dev0001105
9 Cunningham, M., Pergamit, M., Astone, N., & Luna, J. (2014). Homeless LGBTQ youth. Washington, DC: Urban Institute. Retrieved from: https://www.urban.org/research/publication/homeless-lgbtq-youth
10 Russell, S. T., & Fish, J. N. (2019). Sexual minority youth, social change, and health: A developmental collision. Research in Human Development, 16(1), 5–20 https://doi.org/10.1080/15427609.2018.1537772
11. Durso, L. E., & Gates, G. J. (2012). Serving our youth: Findings from a national survey of service providers working with lesbian, gay, bisexual, and transgender youth who are homeless or at risk of becoming homeless. Retrieved from: https://williamsinstitute.law.ucla.edu/wp-content/uploads/Serving-OurYouth-July-2012.pdf
12 Ryan, C., Huebner, D., Diaz, R. M., & Sanchez, J. (2009, January). Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics, 123(1), 346–352 https://doi.org/10.1542/peds.2007-3524
13 Shelton, J., DeChants, J., Bender, K., Hsu, H., Santa Maria, D., Petering, R., . . . Barman-Adhikari, A. (2018). Homelessness and housing experiences among GBTQ young adults in seven U.S. cities. Cityscape (Washington, D.C.), 20(3), 9–33
14. Choi, S. K., Wilson, B. D. M., Shelton, J., & Gates, G. (2015). Serving our youth 2015: The needs and experiences of lesbian, gay, bisexual, transgender, and questioning youth experiencing homelessness. True Colors Fund & the Williams Institute. https://truecolorsunited.org/wp-content/uploads/2015/05/Serving-OurYouth-June-2015.pdf
15 The Trevor Project. (Feb 2022). New report shows homelessness, housing instability linked to increased suicide risk among LGBTQ youth. Retrieved from: https://www.thetrevorproject.org/blog/new-report-shows-homelessnesshousing-instability-linked-to-increased-suicide-risk-among-lgbtq-youth/
16 Fraser, B., Pierse, N., Chisholm, E., & Cook, H. (2019, July 26). LGBTIQ+ homelessness: A review of the literature. International Journal of Environmental Research and Public Health, 16(15), 2677.
https://doi.org/10.3390/ijerph16152677
17. Morton, M. H., Samuels, G. M., Dworsky, A., & Patel, S. (2018). Missed opportunities: LGBTQ youth homelessness in America. Chapin Hall at the University of Chicago. Retrieved from:
https://voicesofyouthcount.org/brief/lgbtq-youth-homelessness/
18 Côté, P. B., & Blais, M. (2019). Between resignation, resistance and recognition: A qualitative analysis of LGBTQ+ youth profiles of homelessness agencies utilization. Children and Youth Services Review, 100, 437–443. https://doi.org/10.1016/j.childyouth.2019.03.024
19. Pachankis, J. E., Cochran, S. D., & Mays, V. M. (2015, October). The mental health of sexual minority adults in and out of the closet: A population-based study. Journal of Consulting and Clinical Psychology, 83(5), 890–901
https://doi.org/10.1037/ccp0000047
20 Goins, E. S., & Pye, D. (2013). Check the box that best describes you: Reflexively managing theory and praxis in LGBTQ health communication research. Health Communication, 28(4), 397–407.
https://doi.org/10.1080/10410236.2012.690505
21. Movement Advancement Project. (n.d.). Equality maps: Identity document laws and policies. Retrieved from: https://www.lgbtmap.org/equality-maps/identity_document_laws
22. Canavan, D., & Ledger, F. (2016). Equal access for transgender people: Supportive inclusive housing and shelters. U.S. Department of Housing and Urban Development. Retrieved from:
https://transequality.org/sites/default/files/docs/resources/EqualAccess-for-Transgender-People-Supporting-Inclusive-Housing-andShelters.pdf
23. Flores, A. R., Meyer, I. H., Langton, L., & Herman, J. L. (2021, April). Gender identity disparities in criminal victimization: National Crime Victimization Survey, 2017–2018. American Journal of Public Health, 111(4), 726–729
https://doi.org/10.2105/AJPH.2020.306099
24 Pearson, J., Thrane, L., & Wilkinson, L. (2017). Consequences of runaway and thrownaway experiences for sexual minority health during the transition to adulthood. Journal of LGBT Youth, 14(2), 145–171.
https://doi.org/10.1080/19361653.2016.1264909
25. Keuroghlian, A. S., Shtasel, D., & Bassuk, E. L. (2014). Out on the street: A public health and policy agenda for lesbian, gay, bisexual, and transgender youth who are homeless. The American Journal of Orthopsychiatry, 84(1), 66–72
https://doi.org/10.1037/h0098852
26. Research, Education, and Advocacy Co-Lab for Youth Stability and Thriving. (2018). Homeless youth risk and resilience survey. Retrieved from: realyst.org
85
27 Barman-Adhikari, A., Rice, E., Bender, K., Lengnick-Hall, R., Yoshioka-Maxwell, A., & Rhoades, H. (2016, July). Social networking technology use and engagement in HIV-related risk and protective behaviors among homeless youth. Journal of Health Communication, 21(7), 809–817
https://doi.org/10.1080/10810730.2016.1177139
28 Mitsdarffer, M. L., & Cook, D. T. (2020). Quantitative methods. In D.T. Cook (Ed.), The SAGE Encyclopedia of Children and Childhood Studies. SAGE Publications Ltd.
29 Nelson, K. M., Carey, M. P., & Fisher, C. B. (2019, May-Jun). Is guardian permission a barrier to online sexual health research among adolescent males interested in sex with males? Journal of Sex Research, 56(4-5), 593–603. https://doi.org/10.1080/00224499.2018.1481920
30 Kosciw, J. G., Clark, C. M., Truoing, N. L., & Zongrone, A. D. (2020). The 2019 national school climate survey: the experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. Retrieved from: https://www.glsen.org/research/2019-national-school-climate-survey
31 James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality.
32. Kolbe, L. J. (2019, April 1). School health as a strategy to improve both public health and education. Annual Review of Public Health, 40, 443–463. https://doi.org/10.1146/annurev-publhealth-040218-043727
33 Centers for Disease Control and Prevention. (2020). Youth Risk Behavior Surveillance – United States, 2019. Morbidity and Mortality Weekly Report, 69(1).
34 West End Neighborhood House. (2023). Life Lines https://westendnh.org/programs/life-lines/
35 Wilmington Delaware, P. F. L. A. G. (n.d.). Local partners https://www.pflagwilmde.org/Local-Partners
36. Housing Alliance Delaware. (2023). Centralized intake. https://www.housingalliancede.org/centralized-intake
37 Rehoboth, C. A. M. P. (2020). About us https://www.camprehoboth.com/about-us
38. University of Delaware Student Central. (n.d.). Lavender Programming Board. Lavender Programming Board. https://studentcentral.udel.edu/organization/lavendarprogrammingboard
86 Delaware Journal of Public Health - June 2023



LIVE proudly and confidently. Find out when you should get screened. DELAWARE HEALTH AND SOCIAL SERVICES Division of Public Health Bureau of Chronic Diseases Visit HealthyDelaware.org/ LGBTC ancer or call 2-1-1 for more information. Take control of your health. Get peace of mind from a cancer screening. The LGBTQIA+ community lives with a higher risk of cancer, but screenings can detect cancer early — when it’s most treatable.* Call your health care provider to schedule a cancer screening today. If you don’t have one, a nurse navigator can offer support and help schedule a cancer screening — even if you don’t have insurance. * Top Health Issues for LGBT Populations Information & Resource Kit, Substance Abuse and Mental Health Services Administration, 2012, https://store.samhsa.gov/sites/default/files/d7/priv/sma12-4684.pdf 87
Delaware’s Domestic Violence Housing Crisis
Monica Beard, D.Phil., Esq. Policy Coordinator, Delaware Coalition Against Domestic Violence
Delaware’s lack of affordable housing has become a public health crisis. There are many influential factors in the causes of local homelessness – the lack of affordable housing units, particularly for extremely low income tenants,1 and many other factors, but one of the leading causes of homelessness in Delaware is domestic violence. It is not sufficient to consider housing without contemplating the complications experienced by those fleeing unsafe homes and abuse. Any solution to the housing crisis must prioritize addressing domestic violence and providing support for the populations most vulnerable to housing insecurity due to domestic violence.
WHY IS DOMESTIC VIOLENCE A HOMELESSNESS ISSUE?
Several national organizations have highlighted that domestic violence is one of the most prevalent causes of homelessness. In the most recent Center for Disease Control report on intimate partner violence, the CDC estimated that 5.5% of women (6.9 million Americans) and 1.4% of men (1.6 million) will need support services due to housing insecurity caused by intimate partner violence.2 Intimate partner violence has been found to be not only one of the leading causes of homelessness, but also of housing insecurity. Women who experience domestic violence are four times as likely to become homeless as those who are not facing an abusive relationship; even when survivors are housed, their abusive partner ensures that their housing situation is never stable.3 In their 2022 Point in Time Survey, which examines the supports provided to domestic violence survivors on one day every year, the National Network for the Elimination of Domestic Violence noted that the majority of the services requests (53%) that domestic violence providers were unable to meet were requests for housing. NNEDV noted the lack of safe and affordable housing options available to many people fleeing domestic violence.4 Ninety-two percent of homeless women report having experienced some form of sexual or domestic abuse during their lifetime and over 50% report domestic violence was the direct cause of their homelessness.5
Homelessness due to domestic violence can take several forms. Sometimes, survivors are so unsafe in their homes with family members that they are forced to leave without a stable housing plan, but it can also include examples where domestic violence has led to broader housing insecurity. Clough, et al. note that in many abusive relationships, there is financial abuse or coercion, where survivors are unable to maintain their own autonomous funds and have their financial independence sabotaged by their abuser.5 Economic abuse can mean that survivors have to deal with low credit ratings or previous evictions, which can make it difficult to find a rental when they seek to find housing without their partner, forcing them to choose between homelessness or returning to the abusive relationship. Stalking and ongoing contact from a former partner can also mean landlords or friends feel uncomfortable providing accommodation to survivors or that safety needs can make certain units inappropriate for a survivor leaving violence. These specific concerns of domestic
violence survivors are exacerbated by the same issues faced by all low income Americans in finding safe, affordable, accessible housing to make it incredibly difficult for survivors to move into affordable housing.
Unfortunately, the lack of housing for domestic violence survivors within Delaware is even more extreme than in other states. The recent report from the National Low Income Housing Coalition (2023) highlights that Delaware has less housing stock than the national average, and this burden disproportionately falls on extremely low-income households. In the 2022 Housing and Homelessness study done by Housing Alliance Delaware, they noted that the number of people experiencing homelessness had doubled since 2019, but that this increase in homelessness was not the same among all groups. While homelessness among adults-only households doubled between 2019 and 2022, it tripled amongst families with children. The year 2022 documented the largest percentage of homelessness amongst children in Delaware ever recorded in an annual count. There is also great racial inequality within the homeless figures in Delaware, with Black Delawareans being five times as likely to experience homelessness as white Delawareans.1
Unfortunately, these inequalities mirror the groups which are most likely to experience family violence, economic inequality and poor health outcomes. Black women and children are more likely to experience abuse within the home than their white counterparts. Black women were also more likely to be criminalized for their responses to domestic violence, which can have considerable effects on their ability to access benefits or become economically independent from their abusers. Black women are also more likely to face serious pregnancy complications or maternal mortality, as well as the highest rates of breast cancer mortality, heart disease and HIV. This is amplified by the economic insecurity that Black women often face, with median earnings that lag far behind white men. This financial insecurity can mean that Black women are often unable to easily leave an abusive relationship and relocate into housing they can afford.6
This correlation demonstrates that, unfortunately, Black women and children in Delaware face these incredibly layered public health crises – both the effects of abuse and of insecure housing and homelessness, as well as the other effects of failures of the health systems towards Black women.
THE LAYERED HEALTH EFFECTS OF DOMESTIC VIOLENCE AND HOMELESSNESS
Experiencing domestic violence leads to long term significant health consequences, both mentally and physically. One in three American women and one in seven American men who have experienced intimate partner violence have symptoms of post-traumatic stress disorder (Center for Disease Control, 2022). Domestic violence has the highest risk of repeat victimization of any type of violence crime, which means that
88 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.015
many domestic violence survivors have to deal with repeat trauma or the extreme vulnerability of the risk of re-trauma. Domestic violence survivors also require more emergency care than the average population and are six times more likely to become dependent on drug and alcohol and are far more likely to exhibit symptoms of other mental health disorders, including depression and anxiety.7
Domestic violence survivors can have additional struggles in accessing emergency housing. Many traditional homeless shelters are intended to be in locations which can be easily reached through public transport. Traditional shelters may not meet a survivors’ need for additional security or safety; for example, they are not necessarily in undisclosed or secretive locations where abusers would be unable to find them. There can be other restrictions on domestic violence survivors when finding permanent housing, such as a history of criminal convictions, erratic behaviors due to trauma, such as substance abuse or severe mental health crises. The effects of economic abuse or coercion can often mean that survivors do not have the relevant credit score to qualify for long term leases or affordable mortgages after leaving an abusive relationship. Survivors often have very specific needs for trauma-informed housing provisions, which cannot always be met without specific in-depth training on trauma and the effects of domestic violence.8
The effects domestic violence has on long term physical and mental health is very similar to the long term physical and mental effects of homelessness, meaning that domestic violence survivors are often dealing with the complex trauma caused by both family violence and an unsafe and insecure housing situation. Empirical studies have demonstrated that those without housing have significantly worse health outcomes than those who are housed. This includes not only respiratory issues and infectious disease, but reproductive health issues such as sexually transmitted infections. Homeless women disproportionately experience these reproductive health epidemics. The life expectancy for homeless people is 20 years less than people who are housed.9
Even once rehoused, domestic violence survivors and their families will often need continual support, with specific safety and support needs and ongoing mental and other health needs. The after-effects of domestic violence and homelessness does not simply end when removed from the traumatic situations; over 25% of women continue to report ongoing mental health needs after homelessness. While it is essential for domestic violence survivors to receive access to housing, housing in itself is not sufficient to deal with these complicated traumas.10
HOUSING SOLUTIONS FOR DOMESTIC VIOLENCE SURVIVORS
Due to these complicated factors of both the internal health issues and practical and financial concerns of domestic violence survivors, it is essential for Delaware to develop specific policies to house families leaving abusive situations. The model which is often cited is Oregon’s Temporary Assistance for Domestic Violence Survivors program (TA-DVS). The eligibility process is far less strenuous than many assistance programs – it applies to either pregnant or parenting Oregon citizens fleeing
domestic violence. It provides direct cash assistance that survivors can use to pay bills – most notably rent payments for housing or security deposits.
TA-DVS waives other requirements which would often be applicable for Temporary Assistance for Needy Families benefits. Undocumented migrant survivors and those who may have earned over the TANF income limits can be eligible for the TA-DVS program, as the program notes that it is essential to ensure that restrictions do not put survivors at risk for domestic violence. A survivor of domestic violence may earn too much income to ordinarily qualify for benefits, yet economic control by their partner means that they are unable to access the income. Strong restrictions on support systems can often mean that some survivors will be unable to access these means of financial independence.
In addition, the TA-DVS program does not put a harsh burden on survivors to demonstrate their abuse – they do not need to file a police report or obtain a protection from abuse order against their abuser in order to access TA-DVS. There are also no employment requirements to access these benefits, nor are survivors asked to seek child support from their abusers or pursue assets from their abusive partner. The TA-DVS gives survivors space to safety plan and make the decisions based on what will keep themselves and their children safe.
In order to support both survivors and employees of the Oregon Department of Human Services, the department has co-located domestic violence advocates in order to provide advice on safety planning, program effectiveness and continual training. Advocates can also provide connections for supporting services, including accessing health services and medical support.
By providing survivors with safe housing and a chance to parent and have health needs addressed without a requirement of employment, Oregon is dealing with the public health effects of homelessness. The presence of domestic violence advocates also allows the TA-DVS to adapt to meet the specific health and safety needs of individual families. The current BidenHarris administration has been urged to federalize this Oregon program in order to support domestic violence survivors across the United States.11
Delaware’s Department of Public Health (DPH) has made some steps toward providing similar supports for specific populations. In 2022, it was announced the DPH would be providing housing assistance and wraparound services for pregnant homeless women.12 Since pregnant homeless women are disproportionately likely to experience homeless violence, it is commendable that DPH is trialing this version of the TADVS. As Delaware continues to commit to creative solutions for ending the public health crisis of homelessness, DPH should continue to fund and expand housing assistance and connected support services.
Dr. Beard may be contacted at nbeard@dcadv.org
REFERENCES
1. Housing Alliance Delaware. (2022). Housing and homelessness in Delaware: 2022. Housing Alliance Delaware. https://www.housingalliancede.org/_files/ ugd/9b0471_322d16c2158c4ab09743a897dc12aa6d.pdf
89
2. Leemis, R. W., Friar, N., Khatiwada, S., Chen, M. S., Kresnow, M., Smith, S. G., . . . Basile, K. C. (2022). The national intimate partner and sexual violence survey: 2016/2017 Report on intimate partner violence. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/nisvs/ nisvsreportonipv_2022.pdf
3. Adams, E. N., Clark, H. M., Galano, M. M., Stein, S. F., Grogan-Kaylor, A., & Graham-Bermann, S. (2021, April). Predictors of housing instability in women who have experienced intimate partner violence. Journal of Interpersonal Violence, 36(7-8), 3459–3481. https://doi.org/10.1177/0886260518777001
4 National Network to End Domestic Violence. (2023). 17th annual domestic violence counts report. National Network to End Domestic Violence. https://nnedv.org/resources-library/17th-annual-domestic-violencecounts-report/
5 Clough, A., Draughon, J. E., Njie-Carr, V., Rollins, C., & Glass, N. (2014, September). Having housing made everything else possible: Affordable, safe and stable housing for women survivors of violence. Qual Soc Work, 13(5), 671–688. https://doi.org/10.1177/1473325013503003
6. DuMonthier, A., Childers, C., & Milli, J. (2017, Jun). The status of black women in the United States. Institute for Women’s Policy Research, https://iwpr.org/wp-content/uploads/2020/08/The-Status-of-BlackWomen-6.26.17.pdf
7 Howard, L. M., Trevillion, K., & Agnew-Davies, R. (2010). Domestic violence and mental health. International Review of Psychiatry (Abingdon, England), 22(5), 525–534.
https://doi.org/10.3109/09540261.2010.512283
8 Baker, C. K., Billhardt, K. A., Rollins, C. W. J., & Glass, N. E. (2010). Domestic violence, housing instability and homelessness. Aggression and Violent Behavior, 15(6), 430–439.
https://doi.org/10.1016/j.avb.2010.07.005
9. Muñoz, M., Crespo, M., & Pérez-Santos, E. (2005). Homelessness effect on men’s and women’s health: A comparison between a representative homeless sample. International Journal of Mental Health, 34(2), 47–61
https://doi.org/10.1080/00207411.2005.11043400
10 Vostanis, P., Tischler, V., Cumella, S., & Bellerby, T. (2001, Winter). Mental health problems and social supports among homeless mothers and children victims of domestic and community violence. The International Journal of Social Psychiatry, 47(4), 30–40.
https://doi.org/10.1177/002076400104700403
11. Futures Without Violence. (2021, Jan). Economic security for survivors of domestic and sexual violence: Policy recommendations for cash assistance programs. Futures Without Violence.
https://www.futureswithoutviolence.org/wp-content/uploads/CashAssistance-Recommendations.pdf
12 Delaware Department of Health and Human Services. (2022, Mar). COVID-19 funding for vulnerable Delawareans and DHSS health care professionals at 24/7 facilities [Press release].
https://news.delaware.gov/2022/03/15/covid-19-funding-forvulnerable-delawareans-and-dhss-health-care-professionals-at-24-7facilities
90 Delaware Journal of Public Health - June 2023
From the Delaware Division of
Diabetes and obesity webinar for employers set for June 6
Delaware employers are invited to a free webinar about diabetes and obesity. The June 6, 2023 webinar runs 9:00 a.m. to 10:30 a.m. Participants will learn how addressing diabetes and obesity can improve workforce health, productivity, and retention and reduce costs. Presenters will share how to access resources to implement evidence-based programs and medical interventions.
According to 2021 data from the Division of Public Health (DPH), of Delaware adults, 12% of Delaware adults have diabetes, 12.6% have prediabetes, and 33.0% report that they are obese





The webinar is sponsored by the Delaware Diabetes Coalition, DPH, Novo Nordisk Inc., and the Greater Philadelphia Business Coalition on Health. Attendees can receive 1.25 Professional Development Credits from the Delaware Society of Human Resource Managers.
To register for the webinar, click here
21st Annual Diabetes Wellness Expo

The 21st Annual Diabetes Wellness Expo will be held on June 20, 2023 from 9:00 a.m. to 3:00 p.m. at Delaware Technical Community College’s Terry Campus, located at 100 Campus Drive in Dover. Admission is free. Attendees will find information about diabetes and prediabetes management, nutrition, and exercise, plus exhibitors, screenings, and giveaways.
The Expo is hosted by the Delaware Diabetes Coalition and the Division of Public Health’s Diabetes and Heart Disease Prevention and Control Program. To register, visit https://www.dediabetescoalition.org/ Registration is free.
DHMIC presents 2023 Kitty Esterly, MD Health Equity Champion Awards
The Delaware Healthy Mother and Infant Consortium (DHMIC) presented the 2023 Kitty Esterly, MD Health Equity Champion Awards during its 17th summit, held on April 18. Dr. Esterly, a pediatrician who specialized in neonatal care, was a visionary who worked to improve health equity.
Black Mothers in Power received the organization award for being a grassroots powerhouse for eradicating racial health disparities for Black birthing people and Black babies throughout Delaware.
Black Mothers in Power burst onto the Delaware scene in 2019 with a community listening series at the Wilmington Library and they have kept up a high level of energy and engagement ever since. With their advocate, Shane' Darby, Black Mothers in Power has consistently connected women and children in need with direct support. Members held diaper drives and other community events, did advocacy work, and worked to improve practices like doula training and reimbursement
Mona Liza Hamlin, MSN, RN, of ChristianaCare received the individual award for her personalized approach in caring for each woman and baby. She has led many initiatives that were the catalysts for statewide change and improvements.
Mona forged a partnership with the University of Delaware to develop the Birth Companion Doula program, which ensures that every mother has doula support throughout her birthing journey. She promoted a diverse lactation staff and manages Christian’s Cribs for Kid's distribution. Mona also organized a breast pump closet at ChristianaCare and designed the Twistle Program, which now has more than 3,000 enrollments and helps increase breastfeeding longevity in one of the largest birthing hospitals in our region.
Help us say thanks!
To nominate an individual or an organization for the annual Kitty Esterly, MD Health Equity Champion awards, visit dethrives.com. Nominations open once a year. Awardees ensure that access to better health is inclusive and within reach of all Delawareans.
Public Health May 202
91
Be smart; prepare for hurricanes
Before tropical storms and hurricanes head our way, prepare to protect lives and property from high winds and flooding. Flooding can occur from heavy rainfall and storm surge in both coastal and inland areas. Take these precautions from the Delaware Emergency Management Agency:
• Know your flooding risk. Type in your address at the Federal Emergency Management Agency’s Flood Map Service Center

• Make an emergency plan Shelters should be your last resort. Determine which friends, family, and hotels may be available to you. Individuals with functional, access, or medical needs and their pets and service animals can stay safe.
• Create an emergency kit beginning with one gallon of water per day for each person and a non-perishable three-day supply of food for all household members and pets.
• Know the latest path of hurricanes and tropical storms at the National Oceanic Atmospheric Agency’s National Hurricane Center
• Sign up for Delaware Emergency Alert Services
• Follow instructions from public safety officials to shelter-in-place or evacuate. Plan your evacuation routes using the Delaware Department of Transportation’s (DelDOT) evacuation route maps DART or Paratransit reduce their routes and may stop completely right before, during, and immediately after a disaster.
• Keep gutters clean. Prune shrubs and trees and remove dead trees and limbs.
• Take photographs of your home and contents (inside and outside). Check the coverage on your homeowner’s, rental, and business insurance policies. Consider flood insurance.
• Keep your cell phone charged and have a charged power bank.
For helpful materials, visit PrepareDE.org, www.dema.delaware.gov, or www.ready.gov
Prepare pets for emergencies
Delawareans should know how to properly prepare for a wide range of emergencies that could affect their lives. As pets are family members, make sure they are included in emergency plans.
Delaware Animal Response (DAR) is a program within the Office of Animal Welfare, located within the Delaware Department of Health and Social Services, Division of Public Health. DAR suggests that pet owners have a pet emergency kit containing:

• three days’ worth of food and water
• medical information which includes vaccination records, medicines, and a first aid kit
• collar with ID tags and extra leash
• crate or pet carrier
• a photo of the pet and pet owner together
• the pet’s favorite toys, treats, and bedding
• plastic bags, litter, and cleaning products. Before emergencies happen, plan where pets can stay Find out now if pets can stay with family, friends, or at a hotel during an evacuation. If the State of Delaware opens a community shelter, pet owners can stay there with their pets. Bring the pet emergency kit to the shelter with the pet because the vaccination records in it will be required to register the pet there. If the pet is normally housed outside, bring it inside immediately and out of danger during bad weather or a disaster
For more information about pet preparedness or how to become a DAR Volunteer Team member, send an email to the DAR Coordinator at dar@delaware.gov. To prepare families and pets for emergencies, visit www.dema.delaware.gov, www.fema.gov, or www.ready.gov
The DPH Bulletin – May 2023 Page 2 of 3
92 Delaware Journal of Public Health - June 2023
DAR Coordinator Edward Bamberger, with his dog “Spud” OAW photo.
Aging is a dynamic time to live fully Aging is a dynamic time to enjoy independence and fulfillment. The Delaware Department of Health and Social Services Division of Services for Aging and Adults with Physical Disabilities (DSAAPD) recommends that aging Delawareans:
• Embrace the opportunity to change. Find a new passion, go on an adventure, and push boundaries by not letting age define your limits. Invite creativity and purpose into your life by trying new activities in your community to bring in more growth, joy, and energy.
• Explore the rewards of growing older. With age comes knowledge, which provides insight and confidence to understand and experience the world more deeply. Grow that knowledge through reading, listening, classes, and creative activities.
• Stay engaged in your community. Everyone benefits when everyone is connected and involved. Stay active by volunteering, working, mentoring, and participating in social clubs and community activities such as at your local senior center.

• Form relationships. As an essential ingredient of well-being, relationships can enhance your quality of life by introducing new ideas and unique perspectives. Invest time with people to discover deeper connections with family, friends, and community members.
For more information, visit the official Older Americans Month website, and follow DSAAPD on Facebook and Instagram.
Public Health Emergency ends
The State of Delaware’s Public Health Emergency Order ended at the end of the day on May 11, 2023 Governor John Carney made the announcement on April 6 May 11 was also the end date of the federal Public Health Emergency.
On May 10, 2023, My Healthy Community reported that 646,924 Delawareans (66.9% of the state population) were fully vaccinated with a primary series of COVID-19 vaccine. Since March 11, 2020 in Delaware, there have been 333,767 total positive cases and 3,394 deaths.
Kids should not ride on lawn mowers
When you were a child, your family member may have given you a ride on a riding lawn mower However, it is a dangerous practice that should be avoided. Children can suffer cuts and traumatic amputations from lawn mower-related incidents. According to pediatric orthopedic surgeon Jennifer Ty of Nemours Children’s Health, lawn mowerrelated pediatric injuries include cuts to the hands and fingers, eye injuries or cuts from rocks and sticks thrown by mowing equipment, and burns. Lifechanging traumatic amputations in children are most commonly caused by lawn mowers
Prevent lawn mower injuries with these safety tips:

• Never have young children in the yard when using lawn mower equipment.
• Never let young children ride on a lawn mower.
• Children should be age 12 and older to operate a walk-behind power mower or hand mower safely.
• Children should be age 16 and older to operate a riding lawn mower safely.
• Children with cognitive or behavior issues, who are immature, or are physically unable to operate lawn mowing equipment safely should not be allowed to mow lawns.
For more safety tips, read Dr. Ty’s blog at https://blog.nemours.org/2017/06/lawn-mower-safety/
The DPH Bulletin – May 2023 Page 3 of 3
93
Providing a Home for Good
Eugene R. Young, Jr. Director, Delaware State Housing Authority
ABSTRACT
In a small state, collaboration is imperative to address complex public policy programs. In Delaware, homelessness is one of the state’s most complex problems. The Delaware State Housing Authority (DSHA) and the Federal Home Loan Bank of Pittsburgh’s (FHLBank) Home4Good program is a case study in how, through collaboration, innovative homelessness solutions can be implemented to help unhoused members of our community find stable housing. This commentary will outline the Home4Good program and explain its success. Finally, the commentary will speak to the need to continue working together to further assist Delaware’s homeless population.
HOMELESSNESS IN DELAWARE
When discussing any public policy problem, it is crucial to understand the data that illustrate the pervasiveness of the issue. One of the most common metrics used to measure the extent of homelessness statewide is the Point-in-Time (PIT) count. The PIT count is an annual two-day count conducted by Continuum of Care volunteers across the country in an effort to gather statistics about the effectiveness of the government’s response to addressing homelessness. The results from this annual count are clear; enough is not being done to address this issue (Figure 1). While 2023’s count results are not available yet, most anticipate the trends will be no different from that of previous years. In 2022, 2,369 people were experiencing homelessness in Delaware alone.1 The data denotes a two-fold increase in the volume of Delawarean homelessness since the beginning of the COVID-19 pandemic in 2020. As of the 2022 report, the PIT count includes people sleeping in emergency shelters, transitional housing for people experiencing homelessness, and hotels/motels paid for by the state or charitable organizations (temporary shelters), as well as people who are unsheltered, meaning that they are sleeping outdoors or in other places not meant for human habitation, such as cars.1 This chart shows the linear trend in Delaware’s homelessness over the past five years: The increasing linear trend conveys that homelessness may worsen without deliberate actions. With the waning availability of many pandemic assistance and protection programs, the number of unhoused Delawareans will only continue to increase unless state leaders, like the DSHA, act.

ADDRESSING HOMELESSNESS
As the primary housing finance and community development agency for Delaware, DSHA continues to look for ways to invest in effective homelessness solutions. One source of funding is FHLBank’s Home4Good grant program. Through a partnership with FHLBank this joint effort has been able to provide almost $5.3 million in grants to nonprofit organizations to support rapid re-housing, homelessness diversion and innovation in homelessness services since 2018.2 Rapid re-housing serves the purpose of assisting individuals and families that meet the definition of “literally homeless” to mitigate the challenges to rapidly obtaining permanent housing.3 Conversely, homelessness diversion programs aid people seeking shelter by helping them to identify immediate alternative housing arrangements and, if necessary, connecting them with services and financial assistance to help them return to permanent housing. Finally, the broadest of the categories – innovation. This service type provides grants to organizations for solutions that look to make the delivery of homelessness assistance more efficient and effective. In Fiscal Year 2022, Home4Good funded programs like rapid re-housing services through Catholic Charities, Ministry of Caring, Inc., and the YMCA of Delaware; homelessness diversion programs through organizations like Family Promise of Northern New Castle County; and innovative services through nonprofits like Brandywine Counseling and Community Services, Inc., and the New Castle County Department of Community Services.4 Through this funding, DSHA and FHLBank have been able to collaboratively support homelessness mitigation efforts.
94 Delaware Journal of Public Health - June 2023 Doi:10.32481/djph.2023.06.016
Figure 1. Delaware Point in Time Counts, 2018-20221
WHY HOME4GOOD WORKS
The impact of this program is centered on the various types of agendas it supports. Each homelessness service model is a proven method to facilitate individuals in unhoused situations moving to more stable housing. With regard to the rapid re-housing model, according to the National Alliance to End Homelessness, rapid re-housing provides short-term rental assistance and services with the goal of obtaining housing quickly, increasing self-sufficiency, and remaining housed.5 Through the funding of repaid re-housing services, unhoused individuals can become more stable in life, and wait times at local shelters can be diminished. Assistance is provided in breaking the cycle of homelessness by offering support that keeps people housed. It is worth noting the cost effectiveness of rapid re-housing as a homelessness intervention method. Of the housing solutions studied in the Family Options Study, rapid re-housing had the lowest monthly cost per family of any intervention studied, as well as the lowest cost for an average stay.6 The cost of an average stay for one family, by program type, was: $6,578 for rapid re-housing, $16,829 for emergency shelter, $18,821 for a permanent subsidy and $32,557 for transitional housing.6 The rapid rehousing model has been effective through Home4Good as well. For example, 870 individuals have been assisted through the above types of services described through the funding rounds for fiscal years 2020 through 2022.5 Furthermore, of the individuals that identified as chronically homeless, 204 individuals were assisted throughout the aforementioned funding cycles.5
Another proven method to get individuals into stable housing is through homelessness diversion. Also known as shelter diversion, homelessness diversion programs look to divert individuals and families from entering emergency shelters or sleeping in uninhabitable places.7 This tactic targets those who have already lost their housing, and are doubled up or may not have a place to stay. Many times, the programs provide financial assistance and robust case management. It is important to note that homelessness diversion is not a denial or barrier to shelter or homeless system entry. Diversion happens at the front door of the homelessness system, but housing-focused problemsolving, which is a crucial part of diversion, can happen upstream and throughout the system.3 Just like rapid rehousing, the homeless diversion services funded through Home4Good have been another effective method to deliver services. To that end, 432 individuals have been assisted through homelessness diversion programs in the funding rounds for fiscal years 2020 through 2022.5 Additionally, of the individuals assisted that identified as extremely low income (i.e. 0-30% AMI), 97 individuals were assisted.5
CONCLUSION
It is clear that our work to address homelessness is not done. Through the Home4Good program, DSHA has proved that through collaboration, complex societal problems can find innovative solutions. To be clear, the Home4Good program is not a panacea for homelessness. Delaware needs to leverage a collaborative, system-based approach to address homelessness and its root causes to ensure that unhoused Delawareans can find a stable home. The mission statement of DSHA is to, “efficiently provide, and assist others to provide, quality,
affordable housing opportunities and appropriate supportive services to low - and moderate-income Delawareans.”
Combating homelessness is just one of the many ways that this agency helps fulfill that calling and expands finite affordable housing opportunities. Using the collaboration with FHLBank as a model, DSHA is ready to engage with federal, state, local and nongovernmental entities to work together toward the common goal of ensuring all Delawareans have access to quality affordable housing.
Mr. Young may be contacted at melissa@destatehousing.com
ABOUT DSHA
DSHA, formed in 1968, is dedicated to providing quality, affordable housing opportunities and appropriate supportive services to low- and moderate-income Delawareans. In addition to its role as the State’s Housing Finance Agency, DSHA is unique in that it also serves as a Public Housing Authority and acts as a Community Development and Planning Agency. As a Public Housing Authority, DSHA receives funding from HUD to build, own and operate public housing in Kent and Sussex counties, two of Delaware’s three counties. For more information about DSHA, please call (302) 739-4263 or visit destatehousing.com.
ABOUT FHLBANK PITTSBURGH
FHLBank Pittsburgh provides reliable funding and liquidity to its member financial institutions, which include commercial and savings banks, community development financial institutions, credit unions and insurance companies in Delaware, Pennsylvania and West Virginia. FHLBank products and resources help support community lending, housing and economic development. As one of 11 Federal Home Loan Banks established by Congress, FHLBank has been an integral and reliable part of the financial system since 1932. Learn more by visiting www.fhlb-pgh.com.
REFERENCES
1. Delaware Continuum of Care. (2022). 2022 Point in time count Summary. Wilmington: Housing Alliance Delaware. https://www.housingalliancede.org/_files/ ugd/9b0471_67a3ffc2765f495580bc310970a39934.pdf
2. Delaware State Housing Authority. (2021). Support for homelessness initiatives. Retrieved from: http://destatehousing.com/OtherPrograms/ot_h4g.php
3. Johnson, J. (2022, October 13). Improving homeless response systems through diversion and problem-solving. Retrieved from: https://endhomelessness.org/blog/improving-homeless-responsesystems-through-diversion-and-problem-solving/
4. Delaware State Housing Authority. (2022). Home4Good awards FY 2022. Retrieved from: http://www.destatehousing.com/ OtherPrograms/othermedia/h4g_2021_awards.pdf
5. Delaware State Housing Authority. (2020-2022). H4G Quarterly Report Totals.
6. Gubits, D., Shinn, M., Wood, M., Bell, S., & Dastrup, S. (2016). Family options study: 3-year impacts of housing. Washington: U.S. Department of Housing and Urban Development.
7. Strategies to End Homelessness. (2023, March 14). Shelter diversion: A best practice to prevent homelessness. Retrieved from: https://www.strategiestoendhomelessness.org/shelter-diversiona-best-practice-to-prevent-homelessness/
95
Homelessness, Housing and Health: The Secrets ALICE Will Not Tell You
Michelle A. Taylor, Ed.D. President and CEO, United Way of Delaware
ABSTRACT
The number of individuals and families facing homelessness in Delaware far outstrips the available stock of subsidized or low-income units. This article reviews facts and figures that paint a grim picture of the plight of persons experiencing homelessness or unstable housing conditions. It discusses low-income, rent-stressed families who do not earn enough to meet basic needs such as food, transportation, childcare and health care. It further explains why the housing crisis has an impact on all of us, whether or not we, ourselves, ever have been without a home. Finally, it provides several possible steps to take to address this seemingly unsolvable puzzle.
THE ILLNESS AMONG US
The housing crisis in Delaware is evident in our cities and on our streets. Persons experiencing homelessness show us their presence, but often we look away. Those people are the visible symptom of a huge – almost inconceivably huge –illness among us.
Housing Alliance Delaware reports that in July 2022, they received 1100 calls from people in a housing crisis or experiencing homelessness and who needed assistance. More than 360 of those callers recently had slept in a car, outdoors, in a homeless encampment or in an abandoned building. Another four hundred households were temporarily staying with family or friends. Sadly, only 231 referrals were available for assistance, and zero permanent supportive housing units were available anywhere in the state.1
This was not a unique finding. The United States Interagency Council on Homelessness reports that as of January 2020, 1,165 Delaware households experienced homelessness on any given day. That number comprised 136 family households, 78 Veterans, 43 unaccompanied young adults (aged 18-24), and 267 persons experiencing chronic homelessness.2
The U.S. Department of Housing and Urban Development reports approximately 16,000 units of public housing and 9,300 housing vouchers are available in Delaware to serve approximately 127,000 households with incomes below the federal poverty level.3
SO, WHAT IS BEING DONE?
In Januar y 2023, Delaware Governor John Carney announced record-breaking funding for housing initiatives in his proposed state budget -- some $101.5 million to go towards affordable housing, including $31.5 million from the state’s revenues and the remainder from the American Rescue Plan Act (ARPA) funds.4
Recently, Wilmington Mayor Mike Purzycki announced what he called the most ambitious housing plan in the city’s history: a $50 million residential redevelopment project. Some $55.6 million of the funding is from the American Rescue Plan Act (ARPA).5 The revitalization is fueled by key partners such as Wilmington Neighborhood Conservancy
Land Bank, Wilmington Housing Authority, DE Affordable Housing Group, Central Baptist CDC / Eastside Housing Partners, LLC, Habitat for Humanity of New Castle County, Woodlawn Trustees / Todmorden Foundation and New Castle County Vo-Tech School District.6
A non-governmental effort, REACH Riverside is building high-quality, mixed-income housing in the Riverside section of Wilmington replacing nearly 300 units of public housing with some 700 mixed-income rental homes including130 affordable income units in a purpose-built community.7
Woodlawn Trustees and partners Todmorden Foundation and HDC MidAtlantic are well into redevelopment of the hundred-year-old homes in The Flats community. More than 220 units of the projected 453 total units in Wilmington’s West Side have been completed.8
Numerous dedicated nonprofits such as First State Community Action Agency, Salvation Army, Sojourners Place, Neighborhood House, Peoples Place and many more provide housing services and emergency shelter.
WHAT ABOUT ALICE?
People experiencing housing emergencies and crises are the proverbial tip of the iceberg. Not far below lies a group who are but one crisis away from homelessness.
UWDE participated with local partners to conduct a study that showed that 32% of Delaware families fall into the category of Asset Limited, Income Constrained, Employed (ALICE).4 These families live above the Federal Poverty Level (FPL) but do not earn enough to meet the family’s basic needs such as housing, food, transportation, childcare, health care, and basic household technology.
They are disqualified from many governmental support programs and the help they do receive does not increase them to a household survival budget level.
The report indicated that in 2019, before the pandemic, 47% of households in Delaware were rent-burdened with rent that accounted for more than 30% of household income, and 24% were severely rent-burdened with rent that consumed more than 50% of household income.
96 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.017
ALICE families are often financially consigned to rental housing (sometimes substandard), in conditions with more people sharing a space, or living in less desirable locations such as neighborhoods with older infrastructure, scarce health care options, food deserts, lacking in greenspace and play areas, and exposure to environmental hazards.
As shown in Figure 1, the survey calculates that a family of four needs to earn $41.20 per hour to meet basic needs. The actual cost of household basics in every county in Delaware is well above the Federal Poverty Level (FPL) for all household sizes and types.
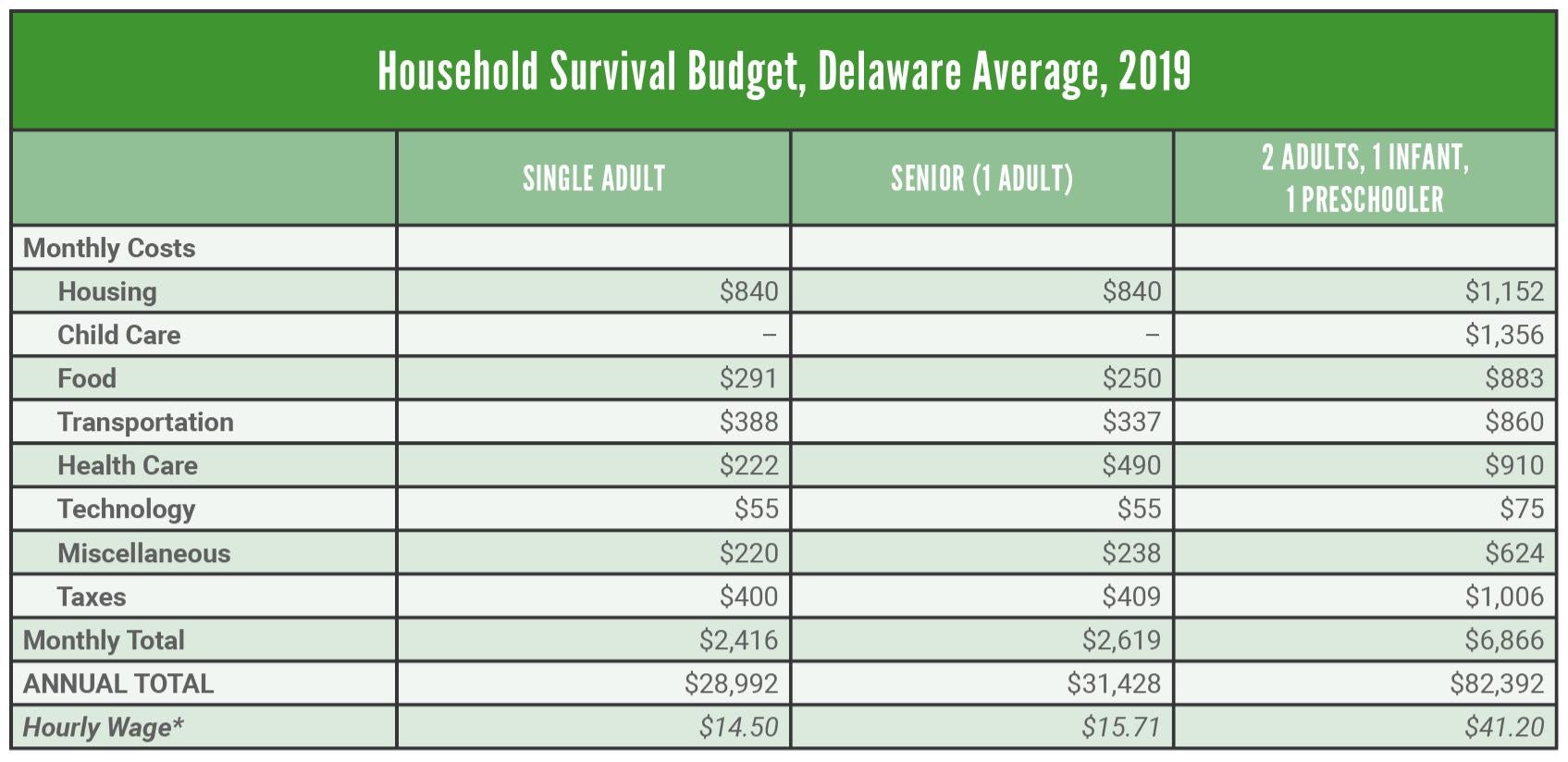
The ALICE survival budget is calculated on costs from 2019. Some four years later, inflation has driven prices higher for necessities such as food, gasoline, and utilities.
When funds run short, cash-strapped ALICE households are forced to make unthinkable choices: Do we pay the rent this month or the childcare? Do we fix the furnace or the car, do we pay the electric bill or order fuel oil? Can we afford to visit a doctor or refill prescriptions?
What do you see in the rent-burdened ALICE family’s future? We see a potential loss of their home or apartment, and possibly eviction.
Discussion of eviction and its consequences are found in a synopsis of a bill9 now in the Delaware General Assembly that if passed, would provide the right to counsel for covered individuals with household income below 200% of the federal poverty guideline for evictions.10
The bill contends that “Approximately 18,000 eviction cases are filed each year in the State of Delaware, and while 86% of landlords are represented by an attorney, agent, or business manager, only 2% of tenants have representation.”
“The disruptive displacement that accompanies eviction proceedings create significant costs for state and local government related to shelter funding, education funding, health care provided in hospitals instead of community-based providers, transportation costs for homeless youth, and foster care. Evictions and disruptive displacement also have significant, well-documented, and long-lasting effects on the lives of individuals and families, including poorer physical and mental health, increased risk of homelessness, increased risk of employment loss, loss of personal property, damage to credit standing, and relocation into substandard housing. Further, evictions fall disproportionately on Black and Latinx families, who have also been the hardest hit by the COVID-19 crisis.”10
The statistics cited paint a dire outlook for the working poor. Going through life burdened by financial stress and fear undoubtedly takes a toll on family dynamics.
• Low-income parents often need to take on more than one job or work jobs with nonstandard schedules and recent studies indicated that more than one-quarter of low-income working parents with children under 12 years of age work evening or night shifts or a schedule that changes week to week. Their children display poorer brain and language development and more behavioral issues, more frequent absenteeism, repeating a grade and placement in special education programs.11
97
Figure 1. Household Survival Budget, Delaware Average, 2019
• Housing disruption both causes and exacerbates family strife. Having no home or being removed from a home can cause negative adults’ job performance issues and possibly loss of work. A lack of public or personal transportation may increase time away from home if a new housing location results in long commutes.
• Businesses may be affected by employee turnover.
• Students may have to change schools or may be unable to attend regularly while the family is relocating. Disrupted students can experience declining grades, inability to connect with peers, depression and dysregulated behaviors causing upheaval in the classroom (and affecting the other students around them.)
HERE IS THE SECRET THAT ALICE WILL NOT TELL YOU
Lacking or inadequate housing affects you —whether you have personally experienced it or not. It is a complex social problem that affects Delaware in many ways: Chronic homelessness causes strain on social services from increased emergency room visits, increased hospitalizations, crime and police intervention, justice system overloads, incarceration, the use of mental health interventions, poverty supports, homeless programs and puts a strain on the foster care system.
Treating persons experiencing homelessness contributes to overall health care costs. Homelessness causes or is associated with serious health issues, including HIV/ AIDS, addiction, psychological disorders, malnutrition, dental diseases, joint diseases and complications of diabetes. For a homeless person, even routine medical care is difficult to adhere to and even maintaining bed rest is complicated when the patient does not have a bed.12
Why is the housing crisis so pervasive?
• There are not enough affordable housing units to meet the need.
• There are not enough housing support services to help families learn the skills to maintain a home, such as budgeting, planning, saving, and understanding the use of credit.
• There are inadequate financial curricula in middle school through high school.
• People living in chronic poverty lose hope for a better future.
• Solutions need long-term commitment and collaboration among government, nonprofits, businesses, financial services, and community leaders.
• Affordable housing must be recognized by the voting public as a long-term investment with a high rate of return.
HOW CAN A STATE APPROACH THE HOUSING CRISIS?
• Continue and strengthen First-Time Home Buyers’ Programs to offer affordable loans, assist with down payments and closing costs, and work with lenders to offer favorable interest rates.
• Increase the use of non-traditional credit data to allow more people to qualify for rentals or homeownership, including wire transfer data, auto insurance payments, rent payments, payments for child care, and others.13
• Incentivize the creation of low-income housing units in all parts of the state.
• Maintain a minimum wage that reflects the local cost of living so working families can thrive.
• Continue to find creative housing strategies for remaining American Rescue Plan funds.
• Drive legislative changes to remove barriers and provide a level playing field for all regardless of race or ethnicity.
We must have the will to win. Do we want to continue to pay for costs associated with the housing crisis, or would we rather use that money to provide affordable housing and help families create a stable, productive lifestyle?
Consider this:
• If homelessness is closely associated with crime and incarceration… Delaware would save the $39,080 per person per year the state spends on incarceration14
• If a family is not rent-stressed, they will have more expendable income to purchase goods and services in the community.
• If a community provides stable housing for children, it is likely to see higher school attendance rates, greater academic achievement, improved student behavior and higher graduation rates.
• If a family has stable affordable housing, residents are more likely to have increased access to health care, healthier lifestyles and improved overall health.
• If an employee can put down stable roots in a location, they will likely remain at the job longer, perform better at work, and contribute to the tax base.
• If a family is not rent-stressed, they may be able to save money to buy a home and begin generational wealth accumulation.
Just as ALICE families face challenges and seemingly impossible difficult decisions, we as a community must face the challenge and make policies and decisions that engender housing equity in our communities.
In the words of Martin Luther King, “No one is free until we all are free.” I will add, “No one is stable until everyone is stable. Dr. Taylor may be contacted at mtaylor@uwde.org
98 Delaware Journal of Public Health - June 2023
REFERENCES
1. Housing Alliance Delaware. (2022) Housing and homelessness in Delaware 2022. Retrieved from: https://www.housingalliancede. org/_files/ugd/9b0471_322d16c2158c4ab09743a897dc12aa6d.pdf
2. U.S. Interagency Council on Homelessness. Continuum of Care report to Dept. of Housing and Urban Development. https://www.usich.gov/
3. U.S. Department of Housing and Urban Development.
4. Kiefer, P. (2023, Jan). Gov. Carney’s 2024 budget offers some tax relief, spending boosts for education, housing. Delaware Public Media.
https://www.delawarepublic.org/politics-government/2023-01-26/ gov-carneys-2024-budget-offers-some-tax-relief-spending-boosts-foreducation-housing
5. Owens, J. (2022, Jan). Wilmington unveils $50M revitalization plan. Delaware Business Times. https://delawarebusinesstimes.com/news/wilmington-revitalization-plan
6. City of Wilmington. (2021). American rescue plan act: Neighborhood revitalization. Retrieved from: https://stories.opengov.com/wilmingtonde/published/8TReFwLj5
7. Riverside, R. E. A. C. H. (n.d.). Redevelopment of Riverside. Retrieved from: https://reachriverside.org/redevelopment/
8. Woodlawn Trustees. (n.d.). The flats. Retrieved from: https://woodlawntrustees.com/the-flats
9. United Way of Delaware. (n.d.). ALICE: Asset limited, income constrained, employed. Retrieved from: https://uwde.org/how-we-work/strategic-initiatives/alice
10. Delaware General Assembly. (2022). Senate Bill 1. https://legis.delaware.gov/BillDetail/79186

11. Sandstrom, H. (2015, Sep). Why parents’ nonstandard work schedules matter for children: Is it the hours or the instability? Urban Institute. Retrieved from: https://www.urban.org/urban-wire/why-parents-nonstandard-workschedules-matter-children-it-hours-or-instability
12. Institute of Medicine. (1988). Homelessness, Health and Human Needs. Committee on Health Care for Homeless People, National Library of Medicine. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK218232/
13. Fannie Mae. (2023, Apr). Selling guide. Retrieved from: https://selling-guide.fanniemae.com/
14. Anderson, J. (2019, May). America spends much more on prisoners than students — here’s why. Go Banking. Retrieved from: https://www.gobankingrates.com/money/economy/states-that-spendmore-on-prisons-than-education
UNWRAP THE TRUTH ABOUT YOUR FAVORITE CIGAR. One large cigar can contain as much tar and cancer-causing chemicals as 10 or more cigarettes. And just like cigarettes, its secondhand smoke is toxic too. Rethink what you’re unwrapping. Just because it’s “premium” doesn’t mean it isn’t deadly.

UnwrapYourSmoke.org
99
THERE’S HALF A PACK IN EVERY ONE.
Fire on My Tongue
Michael Kalmbach, M.F.A. Founding Director, Creative Vision Factory, Wilmington Delaware
“Let Your Life Speak” reads the sign that’s been winking at me on my commute home along Fourth Street in Wilmington (Figure 1). Knowing I ought to be more familiar with the Friends Meeting House on Quaker Hill, the ghost of Thomas Garrett lured me into turning the car around. When I found his barely legible tombstone, I knew exactly how I would let my life speak. It came to me at a Billy Strings concert in Atlantic City. Channeled by another ghost, this time my departed friend and colleague Michael Solomon. Solomon was the heart and soul of the Creative Vision Factory (CVF), a drop-in center that is both a large art room and a refuge for people who are poor, with psychiatric disability, homeless, or who otherwise find themselves marginalized and stigmatized on the streets of Wilmington. Solomon’s death was the hardest among the many we have endured in this era of housing, opioid, and COVID crisis. He loved Atlantic City. When Billy Strings played The Fire on My Tongue, I wept with a force.
Peer support specialists are weary. Ours is a weariness that fuses with the families who have lost loved ones to overdose. It’s a weariness that holds space for our unhoused friends who prefer their freedom in tents and vacant buildings over having their homelessness treated with under-resourced behavioral health tools. May our weariness unite us, and may the fire on our tongues forge the stories needed to trigger cascading change.
Entering our fourth year of COVID, while grieving the loss of disability advocate Judy Heumann, the Creative Vision Factory is bearing witness to the daily humiliation and suffering of individuals experiencing homelessness while navigating multiple disabilities. The CVF regular who got a hard-fought extra day to stay in his hotel room, only to be struck by a car while attempting to cross Route 13 in his wheelchair. CVF’s most prolific artist, recently relegated to spending nights huddled under a dirty hospital blanket with his girlfriend who has cerebral palsy. An elderly woman we know who was turned away from the only shelter in the city on the premise that her disability is too great of a liability, and the fear on her heavily scarred face as she wondered how she was going to get through another cold wet night.
To write these words, to let my life speak through writing, I retreated from my frenetic work environment, always threatening to activate my PTSD, to the Wilmington Library, where I could steal an hour or two of quiet focus. Upon entering, I was taken aback by the numbers of Creative Vision Factory members among the available tables, greeting me with surprised smiles, daps, and looks of recognition. Being able to see our members supported by an infrastructure that I was not responsible for felt good on a molecular level. Writing in this room, and seeing people I have been in intense periods of crisis with quietly smile and nod as they walk by, has been a deep medicine.
Even here, however, there are reminders of the world from which we seek respite. In the library’s Rodney Square Room, like another wink from the ghost of Thomas Garrett, is a painting by N.C. Wyeth, from a series of commissioned illustrations for the 1920 release of Robinson Crusoe. The image is of Crusoe stepping on the head of the Indigenous Friday, after apparently slaying the figure in the background. This is why we need artists, poets, and storytellers reimagining the scope of our public institutions. To instead bear witness to such scenes as the tragic 2015 death of Thomas Cottingham in Rodney Square. Cottingham was an avid skateboarder known as Cannibal by his friends. The policing of Rodney Square after Cannibal’s death created a surge in CVF’s membership. By the time COVID stopped everything in March 2020, CVF stood out as one of the few remaining third spaces in downtown. The composition of this Wyeth painting is strikingly similar to a painting currently hanging at the CVF. What kind of stories and supportive futures can we imagine when that painting, Knicoma Frederick’s One Billion Dollars, joins Wyeth’s in the Rodney Square Room (Figure 2)? Frederick has spent countless days and nights drawing and painting in Rodney Square. In his thousands of drawings lies the influence of the library’s architectural details, permeating his images of life in the city. The many characters and situational dramas that come to life in Frederick’s paintings bring to mind what the late Representative Phil Burton called the “raggedy-ass-lobby.” Writing in the Wilmington Library among the Creative Vision Factory members I can’t help but see Wilmington’s raggedy-ass lobby taking shape.
The pandemic exposed CVF and the Wilmington Library as critical pieces of infrastructure, the very fabric of a woefully

100 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.018
Figure 1. “Let Your Life Speak” banner. Friends Meetinghouse at 4th and West Streets in Wilmington, Delaware. Photo Credit – M. Kalmbach.
underfunded social safety net. The victims of austerity and decades of disinvestment, these constituents are enduring the predictable outcomes of narratives woven around phrases like just say no, trickle-down economics, public-private partnership, and tough on crime. When I look at Knicoma Frederick’s One Billion Dollar painting, I can’t help but see it as a Phil Burton-like fever dream. Completed in March of 2020, just a week before the shutdown, the painting is of a skateboarder, looking like a Radio-Raheem-Uncle-Sam shooting across the city skyline. He drinks from a can celebrating the end of terrorism, and calls for an investment of one billion dollars directly into the hands of the people. Knicoma Frederick is the illustrator of our city’s streets. Through his works I’ve gained a deeper understanding of what it is to receive behavioral health services while experiencing homelessness in Wilmington. In Frederick’s words: “They’re always on time with the meds, and always late with the check.”
I Danced with the Delaware Stars on the floor of the Wilmington library with my colleague Sarah Lester, ultimately losing the trophy to my dearly departed friend and Wilmington Sitting Together Is Radical co-founder, Councilwoman Rysheema Dixon. I sat on that floor, in the same row as activist Bebe Coker and arts advocate Raye Avery, and listened to Marc Lamont Hill talk about his book WE STILL HERE: Pandemic, Policing, Protest, & Possibility1:
“As I reflect on the current moment, I see a widening sky of possibility. The public sphere is filled with radical voices, radical ideas, and radical action. We are dreaming together, envisioning a free and safe world where we finally turn to each other rather than on each other.”


We nurses, teachers, librarians, EMTs and peer support workers are weary, but we are not burned out. We’re heartbroken and under-resourced. The hollowing out of our social safety net has added layers of complex traumatic stress between the lines of our job descriptions. Some of us have protections. Others, after serving through their third winter of housing, opioid, and COVID crisis are rewarded with contract uncertainty, no collective bargaining, and historic inflation. If we are to realize the widening sky of possibility, the hard-earned wisdom of our weariness must be centered. We must turn towards one another and imagine the cascading change triggered by the decriminalization of all drugs. Imagine the lives saved when the drug supply is no longer contaminated. Imagine the trauma that would be eradicated by everyone having their own bed and private bathroom in a Delaware where our hospital systems are robust partners in the development of affordable housing. In the words of Billy Strings:
“The fire on my tongue is for those who die young, and the weariness of we who stay behind.”
Let our lives speak!
Mr. Kalmbach may be contacted at michael.kalmbach@gmail.com
REFERENCES
1. Hill, M. L. (2020). We Still Here: Pandemic, Policing, Protest, & Possibility. Chicago: Haymarket Books.
101
Figure 2: N.C. Wyeth’s Robinson Crusoe illustration (Wilmington Public Library) and Knicoma Frederick’s One Billion Dollars (Creative Vision Factory)
Sunday Breakfast Mission: A Christian Non-Medical Model Toward Addiction Homelessness Rehabilitation
Reverend Tom Laymon President/CEO/Senior Pastor, Sunday Breakfast Mission
On any given night over the past 129 years, the Sunday Breakfast Mission (SBM) has opened its doors to the homeless men—and now women and families—of Wilmington, Delaware. At first, there were a few dozen men who gathered on Sunday mornings for breakfast and church (thus the name), but soon after that first opening, like most early rescue missions, cots were borrowed from another mission in nearby Germantown, PA (Whosoever Gospel Mission) to accommodate the men for nightly shelter.
These efforts were a continuation of the movement that began in Glasgow, Scotland by David Naismith. As a young man, David had seen other young Scottish men come into the cities from the Highlands for work in the new Industrial Revolution, but get caught up in addiction and dissolution. Having been recently converted to Christianity himself, he began to reach out to rescue and disciple these men, starting the City Mission of Glasgow (1826) and then establishing works in Dublin, London and beyond in Europe, America and Africa.
From the start and continuing, we have witnessed a prominent connection between homelessness and addiction to alcohol or drugs among those served at SBM.1 SBM started off as food, shelter and ministry to the soul. The role of volunteers from local churches in particular was preeminent. But also, early on, SBM worked to help participants in its long-term residential Christian program (called discipling) stop using substances, find work, and renew normal life. This was a defining characteristic of SBM, as it was with other gospel rescue missions around the nation and even the world.
Over the years, the emphasis on homeless men expanded to efforts to reach out to impoverished children and mothers in most missions by providing community meals both on holidays and regularly, Christmas gifts, and “mother’s clubs.” SBM had such outreaches throughout its history and even now. These were often facilitated by women’s auxiliaries.
The current work of SBM remains true to what was established in 1893. Nightly, SBM draws guests, anywhere from 130 to over 200 men, women, boys, and girls, for overnight lodging. All of these individuals have the opportunity to eat a full course hot meal together with others from the surrounding community, and a hearty breakfast the next morning. Showers, clothing, shoes, hygiene products, and the reception of mail are provided. Of course, the spiritual component begins with exercising God’s love toward all and providing nightly chapels through the cooperation of local churches.
While the nature and character of the work of SBM has remained the same, the population has changed some throughout the years. In a previous generation, the typical homeless adult was in his fifties, and there were not many women and children. But currently here and across the U.S.,
homeless women and children combined have become the majority, and the majority of adults are significantly younger. So, in 2010, while continuing to provide significant shelter and program space for homeless men, SBM opened a large facility to provide for women and women with children.
Along with providing overnight shelter, the other main portion of SBM’s work is found in its rehabilitation program called the New Life Discipleship Program. This is a free, long-term residential program that is open to men, women, and women with children of any age, and who are homeless for any reason. The core of the program lasts eighteen to twenty-four months, and is divided into three stages. The first stage is a probationary stage of 30 days, during which Program residents participate in initial classes, work therapy, and AM/PM chapels. The second stage is composed of three levels, each with its own goals and objectives dealing with the processes of deconstructing the old life, reconstructing a new life, and rebuilding key relationships. Counseling (individual and group), program classes, education, work therapy, and recreation, as well as morning and evening chapels round out the Christian based rehabilitation program. The final stage of the Program is called Aftercare and is divided into two forms (Aftercare I and Aftercare II). Aftercare I allows the individual to find and begin work to save income for transportation and housing. If deferred, necessary legal fines and other obligations are paid during this time. After an agreed period of six to nine months, and after enough savings have been accumulated, the graduate may then move out and exit into independent living. Sometimes a further period to achieve more ambitious goals such as finishing a degree or a technical certificate, getting married, buying a house, etc. is desired. With approval of the plan and coaching, the resident may pay a modest monthly program fee and then live in Mission housing for up to two years to accomplish these goals. This is the core of Aftercare II. Graduates of these programs have been highly successful in breaking the cycles of addiction and homelessness. The two primary activities of SBM represent the typical rescue and rehabilitation approaches offered by Christian-based, Rescue Missions world-wide. Particular to SBM is its studied understanding of the problem of homelessness.
The first part of this understanding is what homelessness is not. We understand homelessness to be something more than just a function of poverty. Furthermore, only supplementing poverty with additional material resources does not provide a path out of homelessness; someone may become or remain homeless despite available resources. Thus, SBM does not focus on the alleviation of the apparent lack of resources.
Similarly, we understand and approach homelessness as more than a function or outgrowth of “houselessness.” We find that people come to us, not out of the lack of affordable housing,
102 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.019
but rather because of a failure on the individual to maintain their housing and instead using available resources on other, less appropriate activities (e.g. substance use). We also find that many mentally ill or mentally disabled adults lack the capability to self-administer their affairs. In response, we work to prepare people to be ready to handle their own housing, not allowing for problematic habits and addictions to take priority over maintaining housing. Additionally, it is recognized that housing that is reasonable must be in neighborhoods that are not filled with sellers and users of drugs and is well-policed.
Thirdly, we work from an understanding that homelessness is neither solved solely through employment (e.g. “Why don’t they just get a job?”) nor occurs as a necessary result of a lack of employment opportunities. In other words, joblessness is not the prominent cause of homelessness nor is high unemployment a necessary correlation of such. In fact, we often need to encourage the homeless adult to end their particular employment in order to come into the full-time program. Often homeless men and women continue in both homelessness and employment for years, using their income on inappropriate activities, activities that do not contribute to a functioning lifestyle.
The primary way we understand the situation of homeless individuals and families is one in which the relationships to family, friends, employers, church, government, school, landlords, and others have been severed. These key relationships are what typically prevent homelessness. Break all these relationships and, unless one is independently wealthy, an individual will inevitably become homeless.
Two things are prominent in the cases for these broken relationships: substance abuse and mental illness. The former we have found to be prominent in over 90% of those who utilize SBM. The latter is prominent but not nearly as prominent as substance abuse, nor with as clear of a delineation. Certainly, some of the substance use is self-medication for this other issue. Finally, to reiterate, we approach rehabilitation from a Christian/Biblical counseling perspective open to all, not exclusive to those who identify as Christians. There is no requirement that participants affirm the Christian faith to join or remain in the official rehabilitation Program. However, all counseling and curriculum for classes are based in a Godcentered understanding of human nature and a Christ-centered understanding of redemption from sin and the effects of sin like abuse and habitual destructive life patterns. This is carried out in a progressive series of counseling and classes in five levels from a probationary position, to peeling away layers of destructive attitudes and habits, to establishing a new foundation of attitudes, habits and internal personal renewal, to reconnecting broken relationships, and finally a time of practice in real world re-acclimation (Aftercare) where individuals can begin building resources. All of these rely on Biblically-based materials and Christian Counseling.
Rev. Laymon may be contacted at: tlaymon@sundaybreakfastmission.org
REFERENCES
1. Califano, J.A. (2007). High society: How substance abuse ravages America and what to do about it. Public Affairs.
103
Housing, Poverty, and Health Outcomes
Kim Blanch, R.N., B.S.N. Board Member, Sussex County Health Coalition; Board Member, Delaware Coalition of Domestic Violence
ABSTRACT
Poverty and homelessness have significant impacts on the health outcomes of individuals and communities. Lack of safe, healthy, affordable housing in Sussex County requires attention and action to move the needle on the health of our impoverished and housing insecure populations. Health concerns descend on the scale of importance when an individual’s housing and financial circumstances are unstable. Employment opportunities exist, however, housing costs in the area are prohibitive resulting in negative impacts on an individual’s potential for social mobility as well as on local businesses and organizations seeking employees. Social determinants of health are indicated as prominent factors affecting health outcomes, even more so than access to and the delivery of healthcare. Findings from several reports highlight the correlation between financial insecurity, housing insecurity, and health. Innovative and collaborative solutions are necessary to create and hardwire health equity, housing stability, and social mobility within our county and state.
Poverty, as defined by Merriam-Webster Dictionary, is “the state of one who lacks a usual or socially acceptable amount of money or material possessions.” Poverty is also one of the leading factors contributing to homelessness, with additional factors including, but not limited to, the lack of affordable housing, mental illness, and substance use disorder. All of which are very present concerns in Sussex County and the state of Delaware as a whole. Due to Beebe Healthcare’s newly launched Community Mobile Health Clinic (MHC), funded through Delaware’s Division of Substance Abuse and Mental Health (DSAMH), we have the ability and commitment to take care to the communities most in need, several of which are in impoverished and unincorporated areas, where our neighbors who are experiencing homelessness are among the individuals presenting to the mobile health clinic in need of care. Most are presenting without a primary care provider or are unable to recall the last time they had an appointment with a provider. Typically, these discussions around healthcare access include visits to a local emergency department or walk-in clinic, which may have occurred due to a need for immediate care and/or the lack of connection to a primary care provider. And the same medical and social complexity healthcare systems are seeing in patients within their brick-and-mortar facilities exists outside those walls in many communities throughout our county. However, this is not unique to Sussex County or Beebe Healthcare. This reality is statewide.
In the current state and national healthcare landscape, increased awareness and effort are being directed toward identifying social determinants of health (SDOH) with a secondary focus on mitigating their potentially negative impact on patient health outcomes and preventable healthcare utilization. Poverty, housing instability, access to primary care, and access to health services are just four of the nineteen SDOH that the U.S. Department of Health and Human Services lists in its Healthy People 2030 campaign.1 Secondly the Joint Commission on Accreditation of Healthcare Organizations’ new requirements for providers include having designated leadership to reduce health disparities, assess patients’ health-related social needs, provide information on available resources and services, and demonstrate identification of healthcare disparities through quality and safety data stratification
using socio-demographic characteristics.2 And lastly, the Centers for Medicare and Medicaid Services (CMS) released the CMS Framework for Health Equity 2022-2023,3 which details five health equity priorities for reducing health disparities and informs efforts with CMS stakeholders from underserved and disadvantaged areas for the next ten-year period. These recently declared foci of three significant entities in the public health and healthcare system arenas underscore the Robert Wood Johnson Foundation’s County Health Rankings model,4 which depicts the measured influence of clinical care as it correlates to health outcomes is 20%, leaving 80% to other health factors, policies, and programs. This category includes access to care, as it pertains to insurance - or lack thereof - in addition to the accessibility of primary, mental, and dental care as well as the quality of care, which encompasses preventable hospital stays, mammography screenings, and influenza vaccinations. Although the physical environment in this model holds a weight of 10% with severe housing problems as a subcategory, it does not include severe housing cost burden, homeownership, or air & water quality in its calculations. Additionally, the category of social and economic factors weighted at 40% includes community safety, which encompasses injury deaths, homicides, suicides, firearm fatalities, motor vehicle crash deaths, and juvenile arrests And yes, it still does not include the effects of residential segregation, median household income, living wage, and several other highly influential aspects existing in many of our communities that are now well-recognized contributors to health outcomes. Figure 1 shows the County Health Rankings model demonstrating these percentages as they pertain to health outcomes with an equally divided categorization of the length of life and quality of life.
As a community-based healthcare system, Beebe Healthcare has been expanding its awareness and committing resources to identify the social determinants of health of its patient population and support connection to appropriate resources through specific initiatives. In addition to existing programs, Beebe is actively developing and implementing innovative programs to not only meet the needs of one of the fastest growing counties east of the Mississippi River but also to focus efforts on the health inequities and disparities that were
104 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.020
spotlighted by the pandemic. Our triennial Community Health Needs Assessment5 (CHNA) conducted in 2022 resulted in three areas of prioritized need: Behavioral Health, Chronic Disease, and Healthy Lifestyles (figure 2). Each of these prioritized areas is being addressed through both a health equity and SDOH lens.

Throughout the CHNA primary data collection process that included a community member survey, key stakeholder interviews, and two focus groups, homelessness and lack of affordable housing were on the list of top concerns. Data from
Dignity Health and Truven Health Analytics were obtained to quantify the severity of health disparities in our county and the subsequent Community Need Index (CNI) data source was used in the health assessment. CNI considers multiple factors that are known to limit healthcare access, and the tool is useful in identifying and addressing the disproportionate and unmet health-related needs of neighborhoods (figure 3). The five prominent socioeconomic barriers to community health quantified in the CNI are income barriers, cultural/language

105
Figure 1. County Health Rankings Model
Figure 2. Beebe Healthcare’s FY2022 CHNA Needs
barriers, educational barriers, insurance barriers, and housing barriers. A score of 5.0 represents a ZIP code area with the most socioeconomic barriers (high need), while a score of 1.0 indicates a ZIP code area with the lowest socioeconomic barriers (low need). A low score is the ultimate goal; however, ZIP codes with a low score should not be overlooked. Rather, communities should identify what specific entities are succeeding, such as accessibility to care that results in effective mitigation of preventable hospitalizations as well as effective health policy and local health planning, which ensures a low score.5
As the previous map indicates, most zip codes in Sussex fall within the moderate and high need levels. Combining a 20172021 poverty rate of 11.5% per the U.S. Census6 with the rates of homelessness and lack of affordable housing in Sussex County, it is worth exploring the potential correlation between poverty and housing insecurity. Additionally, ALICE in Delaware – A

Financial Hardship Study7 published in 2021 reveals critical information about our statewide neighbors. In 2019, 38% of the 376, 239 households in Delaware struggled to make ends meet; 11% were living below the Federal Poverty Level, and the other 27% fell into the ALICE category: Asset Limited, Income Constrained, Employed (figure 4).
According to the report, ALICE households were at 21% in 2007, which further proves that more Delaware households have moved toward the ALICE threshold over the last decade, and families already in the ALICE percentile were unable to rebuild or replenish their savings.
As figure 5 from the ALICE report demonstrates, these are undeniable challenges that demand consideration and clearly outline the potential negative impact these circumstances could have on the health outcomes of an individual or a population.
106 Delaware Journal of Public Health - June 2023
Figure 3. ZIP Code Map of CNI Scores
How does any one individual who is struggling to make ends meet, or who is not even close to doing so, focus on their physical health needs - until it reaches a level of severity that inhibits their ability to work, care for their loved ones, or put food on the table.
To further emphasize the SDOH and associated challenges present in Delaware’s southernmost county, the Impacted Communities Study, completed by Sussex County Community Development and Housing Department in 2016, found that 14 areas of concentrated poverty around Sussex County are known as impacted communities.8 All 14 communities report issues of water quality, vacant and abandoned housing, animal control issues, trash issues, and traffic and safety concerns. This study reports that 32% of homes in impacted communities need minor repairs, and 37% need major repairs.
Additionally, the Housing Opportunities and Market Evaluation report was completed by LSA Planning for Sussex County Council in 2019, with the following findings8:
• More than 24,000 households living in Sussex County spend more than 30% of their income on housing costs.
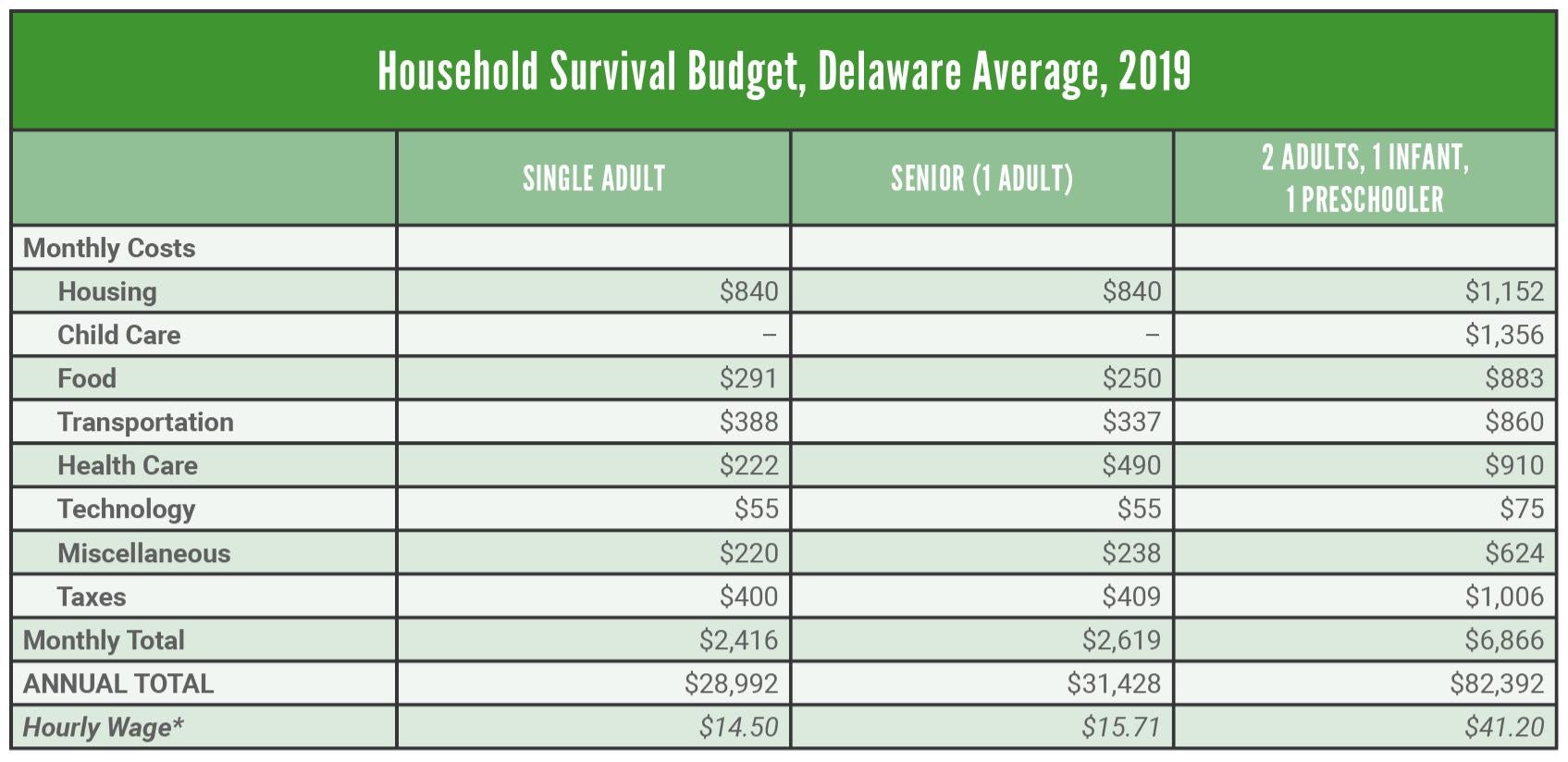

• A full-time, year-round minimum wage worker has an income of about 30% of area’s median income, which allows them to afford housing that costs no more than about $380 per month. No housing in the county is available at this rent level.
• Between 2020 and 2050, the county needs to produce 17,597 new housing units to meet the needs of the growing county. Approximately 22% of these homes need to be for households earning less than 50% of the Area Median Income (this equates to households of 4 making $42,000 or below per year).
• Health Care and Social Assistance is another large and growing industry in Sussex County, with higher wages ($50,000s) on average than jobs in the tourism industry. While wages are slightly higher, a range of lower-wage occupations (e.g., home health aides, administrative) suggest a growing need for lower-priced homes to accommodate growth in this sector.
• On average, households spend 53% of their income on housing and transportation costs. This is before taxes are taken out.
The need for stable, safe, affordable housing is paramount. Taking into account the numerous circumstances that can be present for families and individuals such as lack of a livable wage, lack
107
Figure 4. Households in Delaware Requiring Assistance7
Figure 5. Delaware Average Annual Household Survival Budget, 20197
of ability to properly care for children and/or aging parents, the heightened levels of stress, and worst of all, substandard housing or lack thereof, healthcare is highly likely to descend even further on the list of daily priorities. This is where our state agencies, public health division, and healthcare systems have an opportunity to collaborate and create accessible and convenient avenues to high-quality, safe, and affordable healthcare with a comprehensive array of social service resources. However, it does not stop there. Social mobility is necessary to effect lasting change. Social mobility and equality of opportunity can be measured in terms of earnings, income, or social class. Still, they can also be understood to encompass other well-being dimensions, such as health and education. Beebe’s Community Mobile Health Clinic was invited to an apartment complex in Seaford in recent months and had the opportunity to offer preventative health screenings and mental health services to the residents and adjacent neighborhoods. Understanding that the mobile clinic moves at the speed of trust, and it was our first time on site, we did not anticipate a high level of interest but were available to be of service to anyone interested. What ended up happening was an impromptu career day. Over twenty children of elementary and middle school ages eagerly boarded the mobile clinic and began asking questions about what we do, listening to each other’s heartbeats and lung sounds with assistance from our staff, and telling us which healthcare professional they wanted to be when they grew up. All these conversations were provoked by what they experienced in those few hours.
As importantly, the pandemic highlighted the need to meet people where they are. As an example, Beebe Healthcare stood up numerous sites in Lewes, Georgetown, and Millsboro that offered community-based testing and vaccination opportunities. An offshoot of those efforts was a partnership between Beebe, Sussex County Libraries, and Sussex County Emergency Management Systems that involved deploying the Bookmobile as a low-barrier, low-tech, easy-access point with a walkability factor for COVID-19 vaccinations. Leaning into a longstanding relationship with First State Community Action Agency, we were introduced to community champions and respected leaders in underserved and marginalized neighborhoods in Sussex County. This endeavor allowed us to meet people where they were and foster connections through conversations that included, but were not limited to the vaccines. The Bookmobile staff were asked questions about conditions other than COVID, such as how safe hospitals and doctors’ offices were for their loved ones needing care, could they schedule a same day procedure, should they schedule that imaging they were supposed to have done months ago; could we help them get food for their family; and numerous other topics. This place-based presence afforded us many opportunities to discuss the delay of care and its potential repercussions. By bringing care to people where they live, work, worship, and play, it was not only an integral component in the provision and accessibility of care, but it played a valuable role in reinforcing the importance of health and wellness - particularly at a time when distrust of public health and healthcare, in general, was exacerbated by fear and misinformation.
As Beebe Healthcare moves forward in our efforts to recognize and mitigate the social barriers our patients face, we acknowledge the work of many of our Beebe teams and programs. To highlight
a few, our environmental services team recently onboarded several individuals into full-time positions who are currently residing at the pallet village, a transitional housing community consisting of 40 cabins in a supportive village setting with shared common areas. This opportunity has the potential to change the trajectory of those new Beebe team members, and it can open cabins in the pallet village to other individuals experiencing homelessness as the newly employed community members have the potential to transition to more permanent housing. Our home health agency has served the community for many years with a multidisciplinary approach that includes social work visits and collaboration with other teams and agencies to best connect patients to needed support services. Our transitional care programs support patients who are high utilizers of the healthcare system and/or are diagnosed with significant chronic conditions as they return to their places of residence, some of which are in marked states of disrepair and may have contributed to their frequent visits to the acute care setting. One such example involved a patient who was admitted just two months after her first admission. The patient fell twice within a short timeframe due to sheets of plywood haphazardly placed over their disintegrating floor. The initial fall resulted in a fractured femur and a subsequent fall upon the return home resulted in a fractured clavicle which required a second admission. A circumstance such as that one has the potential to be avoided, at least prior to the second admission, through a soon-to-launch collaboration with Milford Housing Development Corp. (MHDC) with funding from Energize Delaware. The Ecosystem Empowerment Grant allows Beebe Healthcare staff to identify patients who are income-eligible homeowners and in need of minor and major repairs, safety-related modifications, and/or energy efficiency interventions. Upon determination of eligibility through designated staff at Beebe and MHDC, subject matter experts will assess these patients’ homes, and a remediation plan will be developed. Funding could support improvements in up to twenty-five homes depending upon the needs addressed. And it’s quite possible, given the lack of affordable housing in Sussex County and the prevalence of both homeowner-occupied and renter-occupied substandard housing, healthcare systems participating in this grant opportunity may have employees who could potentially qualify for the program. Beebe Healthcare is very aware of the housing needs in our area as recruitment efforts offer ongoing insights into the lack of affordable and conveniently located housing at all position levels. Basic economics underscore the supply and demand realities of housing in Sussex County. Recent research sheds light on the precariousness of people’s housing situations as we find ourselves in the midst of historically high rent prices and inflation. The estimated increase in homelessness is projected to be 9% for every $100 increase in median rent. Market adjustments in payrates certainly help organizations remain competitive on a local and regional level. Unfortunately, the gap not only exists but continues to widen between median household incomes and local housing costs. Ancillary staff for new practices and locations encounter difficulties when seeking housing options closer to their workplace, and they are not alone. Other industries speak to these same challenges as do businesses that rely heavily on international students seeking seasonal employment in our coastal region as a means of increasing staff to meet the demands of high tourismrelated volumes.
108 Delaware Journal of Public Health - June 2023
In summary, poverty is just one piece of the proverbial puzzle. Employment opportunities in Sussex County are abundant year-round, not just in seasonal stretches, as many businesses demonstrate through a reduction in operational hours with explicit statements pertaining to lack of staff posted on their doors. However, understanding that the move from homelessness to housed for any individual may require more than a job, consensus from a county-wide, cross-sector collective is necessary to affect change and commit to making safe, affordable, and healthy housing opportunities available to all in order for individuals, communities, local economies, and systems to thrive. Innovation and collaboration are necessities when considering ways to collectively mitigate poverty, homelessness, substandard housing, and poor health outcomes in our communities. Social determinants of health strongly contribute to the disparities and inequities we see daily in our state and throughout our country. There is a great focus from diverse organizations on health equity, affordable housing, and social mobility. And there may be copious ideas on tackling any or all of them. However, none of us can do this alone. It will take a collective impact approach to affect profound and lasting change. Collaborative, data-driven decisionmaking coupled with the amount of determination and commitment I, for one, witness in our community partners is present up and down our state. A unified commitment to do what is best for our fellow residents is worth exploring.
Ms. Blanch may be contacted at kblanch@beebehealthcare.org
REFERENCES
1. Office of Disease Prevention and Health Promotion. (n.d.). Healthy People 2030 building a healthier future for all. Retrieved from:
https://health.gov/healthypeople/priority-areas/social-determinants-health
2. The Joint Commission. (2022). R3 Report - requirement, rationale, reference. Retrieved from: https://www.jointcommission.org/-/media/tjc/documents/standards/r3reports/r3_disparities_july2022-6-20-2022.pdf
3. Centers for Medicare and Medicaid Services. (2022, April). CMS framework for health equity. Retrieved from: https://www.cms.gov/files/document/cms-framework-healthequity-2022.pdf
4. County Health Rankings. (2023). Building a culture of health, county by county. Retrieved from: https://www.countyhealthrankings.org/explore-health-rankings/countyhealth-rankings-model
5. Beebe Healthcare & Umbach. T. (2022). Community health needs assessment. Retrieved from: https://www.beebehealthcare.org/sites/default/files/2022-11/2022%20 Beebe%20CHNA%20Report.pdf
6. US Census Bureau. (2022, July 1). Quick Facts Sussex County, Delaware. Retrieved from: www.census.gov: https://www.census.gov/quickfacts/sussexcountydelaware
7. United Way of Delaware. (2021). ALICE in Delaware - a financial hardship study. United for ALICE. Retrieved from: https://www.unitedforalice.org/state-overview/delaware
8. Sussex County. (2016). Impacted communities study. Retrieved from: https://sussexcountyde.gov/impacted-communities-study
109
A Vision for Community, Connection and Reinvestment
Amanda August, M.A.
ABSTRACT
Jefferson Street Center (JSC) implements community-driven priorities that support quality of life, improved community health and neighborhood vitality in Northwest Wilmington. JSC serves as a Connector and Capacity Builder in the Washington Heights Blueprint Community® and its surrounding neighborhoods and responds to the needs of residents and stakeholders. The organization focuses on two implementation strategies: opening of a shared-use community hub, in partnership with Hanover Presbyterian Church, and channeling resources to implement place-based revitalization projects and initiatives. These strategies focus on long-term efforts to cultivate place-based asset growth, aiming to alleviate poverty, promote housing stabilization and grow civic muscle. These strategies are also specific tactical responses to the public health concerns of the residents and stakeholders in Northwest Wilmington.
As a small yet growing nonprofit, the organization is building toward these efforts through the growth of collaborative partnerships, focusing on leveraging established resources into Northwest Wilmington. JSC is also working within the structure of its Community Hub to elevate programming directly supporting positive outcomes associated with social determinants of health, such as workforce development, food access, physical activity and connections to educational opportunities. All efforts continue to be guided by the values, needs and priorities of the surrounding neighborhoods and local community members and leaders.
JEFFERSON STREET CENTER
Implementing Community development initiatives through an asset-based framework promotes long lasting impact, strengthening civic muscle and sense of belonging.
As one of the last active Blueprint Communities® in Delaware, Jefferson Street Center (JSC) works to preserve resources in Northwest Wilmington while empowering the resourcefulness of
local community leaders and networks. Resourcefulness-based approaches1 support the development of self-determination regarding choices about health, access, distribution of goods and building agency. This approach to organizing and elevating is embedded in the strategic mission of JSC.
JSC is a growing grassroots 501(c)(3) that serves four Census Tracts (2,3,4 & 5) and two Qualified Census Tracts (3 & 4), in which at least 50% of the households have an income less than 60% of the Area Median Gross Income. The organization’s service area is bounded by North Market Street, Lea Blvd, Broom Street/Miller Road, and the boundary of Brandywine Park (Figure 1).
There are several communities that reside within Northwest Wilmington: Brandywine Village, Baynard Village, Harlan Neighborhood, 9th Ward and Triangle Neighborhood. The area is composed of a majority BIPOC residents, mostly African American. Each community has differing assets, needs and boundaries, which is reflected in the 2020 Census Data.

110 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.021
Figure 1. Map of Jefferson Street Center Service Area
Throughout the service area, residents who live below the poverty level peak at 35%, with 23% representing individuals over the age of 65. In certain areas, upwards of 65% of adults over the age of 25 have not graduated high school, translating to a 68% unemployment rate for residents ages 16 and over. Over 40% of households are married, and 38% of total households also have children. While there is a strong homeownership and renter population within the Northwest, some areas reveal up to 18% of the housing stock as vacant.
This data only tells part of a story. These communities are growing their civic associations and finding creative ways to engage and recruit new neighbors or those who are not on social media. They meet on evenings and weekends to clean up the yards of vacant properties or fundraise to plant new trees on their hot, city streets. Local organizers volunteer to create momentum around healthy food and cultural events, working to alleviate the lack of substantial grocery stores in the area. Neighborhoods that are more affected by crime utilize their deep networks to prevent public health scares, which range from shooting sprees to low-access health care and go door-to-door to build awareness and support. Residents and local stakeholders work together to build up the commercial corridor on Market St. and Concord Avenue to increase local job opportunities for the residents. These organizing approaches, which leverage deep resourcefulness, feed the strategic planning of Jefferson Street Center and its community-centric collaboration.
The organization, which originally served as a nonprofit childcare center from 1987-2010, located in Hanover Presbyterian Church, closed because of the Great Recession in 2010. As a result, several members of JSC’s board, Hanover congregation, and additional community members began to engage with the local schools as part of the Delaware Readiness Team ecosystem. Funded by the Early Learning Challenge Grant in partnership with private foundations and corporations, Delaware Readiness Teams are a state-wide initiative offering a unique opportunity for communities to build strong and reciprocal linkages between early learning and K-12 schools and support young children’s, ages 0-8, readiness for school and for life. As a result, this dynamic group, called the Hanover Dream Team (HDT), started working in the community surrounding Warner Elementary and Shortlidge Academy schools in 2013. Part of the work of the HDT Readiness Team included a community assessment to better understand the needs of parents and guardians raising children in the community. The community boundaries of the HDT Readiness Team are nearly the same as the boundaries of the current Washington Heights Blueprint Community®. Three central themes emerged from the HDT Community Assessment2:
1. How individuals felt about their community varied greatly depending upon the street and sometimes the block where they lived.
2. Breaking the cycle of inadequate parenting is critical.
3. Personal and organizational connections and relationships make a real difference in how a person feels about their community.
As these themes laid the groundwork for the HDT Readiness Team, who looked to expand their outreach, they were informed of the Blueprint Communities® proposal request from the University of Delaware Center for Community Research & Service.
Additional members were recruited to the team and a proposal was submitted; Washington Heights Blueprint® revitalization initiative was eventually approved and began the process in 2016. The Washington Heights Blueprint® team was composed of demographically diverse members of the service area, and the city of Wilmington, as well as representatives from a variety of job sectors. Throughout this year-long engagement endeavor, the team received training through the University of Delaware, which provided the skill sets to utilize relational data collected from JSC’s service area. This trust building activity laid the foundation for the work ahead and was a catalytic exercise for getting the organization on the community development map. The trained team engaged directly with local stakeholders, identifying assets to protect, issues to address, and projects to prioritize. As a result, the Washington Heights Blueprint Community® Revitalization plan was constructed, and it drives the strategic work of JSC today. The strategic issues that arose out of the Blueprint® plan focused on six buckets: Public Safety and Crime, Education, Youth Opportunities, Cleanliness, Housing and Rentals and Family & Household Relations (figure 2).
Growing its grassroots efforts from this plan, JSC advances community-driven development work toward neighborhood vitality throughout Northwest Wilmington. Five years after the Blueprint® process began, the organization hired its first staff to carry out its operational strategy, connecting with community leaders and partners in JSC’s service area, and to learn what had changed since 2016. The staff work to connect with stakeholders in the service area, building strong rapport and identifying the importance of trust relationships, particularly in disinvested communities. It has been through a steady and consistent presence (e.g., attending monthly civic meetings, listening more than talking, organizing and volunteering at neighborhood cleanups, being invited into places of worship, business or people’s homes) that residents have grown to recognize that JSC is truly invested in working with them to build stronger, more connected neighborhoods.
Focusing on community-driven development, and as a result of the Washington Heights Blueprint Community®, JSC focuses on two implementation strategies: operating a shared-use community hub in partnership with Hanover Presbyterian Church and leveraging resources to implement place-based revitalization projects and initiatives throughout Northwest Wilmington. These strategies are aimed at investing in all residents and stakeholders throughout our service area. These efforts focus on providing programmatic opportunities for youth and intergenerational connection; increase civic muscle and engagement through education and revitalization efforts; build on positive assets and activities to grow a strong, connected sense of place; connect resources to small businesses, nonprofits and organizations; and address areas of concern that affect the health and wellbeing of stakeholders. To achieve these goals, JSC serves as a Connector, providing responsive hub programming to the surrounding communities, supporting the recovery efforts from COVID-19 and building partnerships to support the growth of strong housing stock. The organization also works as a Capacity Builder, focusing on supporting youth and neighboring schools and leveraging resources to organizations, groups and programs that serve the community.
111
THE COMMUNITY HUB
Jefferson Street Center, in partnership with Hanover Church, has established the first community hub in the Washington Heights Blueprint Community® neighborhoods and Northwest Wilmington. From any direction, there is no other Community Hub within one mile of JSC. The building provides access to a commercial kitchen, basketball gym, classroom space and a social hall with a stage. Throughout the Blueprint Community® Revitalization process, as well as a recent impact survey conducted with community stakeholders in summer 2022, residents and participants emphasized the need for a safe neighborhood space for recreation, physical activity, intergenerational programming, resources and a place to share a meal, promoting a sense of belonging.
Our Community Hub3 is a central point where residents can access a range of services, programs, and/or activities offered by diverse organizations, community groups or individuals depending on the needs of the community. It is a conveniently located space that is recognized and valued by local residents (figure 3).

The hub’s current direct services are highly utilized, which include a food pantry and clothing closet. Within JSC’s service area, 35% of the community lives at or below the poverty line, earns less than $25,000 annually4 and has a highly concentrated area of seniors 62 and older, who live in subsidized housing. Based on this data, JSC conducted a six month pilot program in 2022, which hosted over 180 community events focused on physical health and well-being, addressing food insecurity, workforce development, youth programming and access to personal care needs. A quantitative survey was also conducted, collecting responses from 75+ participants, volunteers, program leaders and staff.
The survey results revealed that the most vulnerable recipients of services, like from our food pantry and clothing closet, experienced an increase in well-being, social connectedness and physical health. JSC then looked to grow the program’s impact and incorporate partnerships into an already-existing framework,
with the goal of connecting services to alleviate the symptoms of poverty. The organization partnered with Bright Spot Farms, who provided free produce for 16-weeks along with recipe examples and lesser-known foods, as well as the Wilmington Community Advisory Council to directly connect incomequalified individuals to free or reduced internet. These services are provided during the Food Pantry, which doesn’t demand additional travel for recipients to receive these services. JSC also partnered with Network Connect, who worked with the Food Pantry and Clothing Closet programs to host free stores, which provide free personal items to the community.
The unique approach of co-facilitating a shared use space within a faith-based building provides a breadth of opportunities to a multitude of initiatives to thrive while keeping the integrity of the space. First and foremost a place of worship, developing meaningful relationships with the congregational community creates capacity for equitable input. The resourcefulness embedded in the networking emphasizes trust-building and transparency, encouraging both organizations to work with each other through an inclusive and generative practice. Throughout the six month pilot program, which brought new programming into the church, this demonstrated a sustainable opportunity to reactivate building amenities, grow connections and cultivate positive outcomes.
COMMUNITY-DRIVEN PROJECTS AND PRIORITIES
Revealed in the Washington Heights Blueprint Communities® Revitalization Plan, participants expressed the need to protect assets, such as green spaces, small businesses and schools, and address areas of need, like public safety and crime, cleanliness and housing stock. Through the leveraged impact of strong partnerships, JSC directly supports efforts of beautification, facilitating neighborhood clean-ups, subsidizing beautification efforts and working with local organizations to grow green spaces. Continuing to serve as a connector, the organization is channeling resources directly into these efforts, which are facilitated by the
112 Delaware Journal of Public Health - June 2023
Figure 2. Washington Heights Blueprint® Strategic Issues
Benefits of Shared Use
People everywhere want access to safe and affordable recreational spaces. With shared use, public and private property owners can open underutilized facilities for community use. Though often used as a strategy to increase opportunities for physical activity, shared use has many wide-ranging benefits.
communities themselves. Some of these efforts include garden installations on highly trafficked areas, the purchasing, planting and maintenance of trees in residential pockets, and providing items needed for neighborhood cleanups.
As a Capacity Builder, the organization is building its infrastructure to advance asset growth in Northwest Wilmington. JSC is currently in the process of starting a seed funding pilot program, providing microgrants to small businesses and organizations for a capital project, program or engagement activity. As the organization continues to be introduced to budding entrepreneurs or grassroots programs, the opportunity to connect them to additional resources and partners will bolster their chances of success, impact and sustainability.
JSC is also focusing on building long-term relationships to support the alleviation of housing insecurities and grow home ownership. The organization participated in the Cinnaire Jumpstart program in 2022, which provided foundational tools about the housing development process, partners in the field and funding sources for small start-up developers. As a result, JSC has connected several residents in its service area to the program, including members of its board, to build the toolbox of home ownership. As the organization strategically grows, connecting resources to support the renter-to-home ownership pipeline is a priority, as well as partnering with financial institutions to assist individuals with credit recovery, education, and financial planning.
Health
INCREASED PHYSICAL ACTIVITY among people who live near recreational spaces
REDUCED RISK OF CHRONIC DISEASE associated with more physical activity
BETTER ACCESS TO HEALTHY FOODS through community gardens and kitchens
IMPROVED MENTAL WELL-BEING for those who live near parks or recreational facilities
REDUCED STRESS for people who spend more time outside
Equity
MORE OPPORTUNITIES FOR PHYSICAL ACTIVITY in low-income communities and communities of color, which are less likely to have access to recreational spaces
REDUCED HEALTH INEQUITIES by creating more spaces for play and exercise in the communities that need them most
Community
DECREASED CRIME, VANDALISM, AND VIOLENCE in recreational spaces that residents use regularly
STRONGER COMMUNITY TIES through informal interaction, organized activities, and volunteering
Education
IMPROVED ACADEMIC PERFORMANCE among kids who are more physically active
BETTER CLASSROOM BEHAVIOR when students can play and be active
Economy
MORE COST-EFFECTIVE than building new resources or facilities
INCREASED ECONOMIC OPPORTUNITY when shared use supports small business incubation
HIGHER PROPERTY VALUES for properties closer to parks, open spaces, and recreational facilities
Another revitalization focus is Baynard Blvd between 18th and Concord Ave, particularly concerning better sidewalks and street safety.5 After serving as the official partner for the first Baynard Blvd Open Streets event, in which 0.7 miles of the artery was closed, the community was buzzing with energy to affect long lasting change on the four-lane road.
JSC followed-up with University of Delaware Living Labs, who was present during the Open Streets event, to collect resident input on the safety of Baynard Blvd. The results revealed the high level of concern around safety and traffic hazards, and the lack of accessibility for pedestrians, bicyclists and individuals with differing physical abilities. Serving as a connector and facilitator, JSC connected with DelDOT, City of Wilmington, WILMAPCO, and Urban Bike Project to establish a plan that could create a space and platform for community members to directly share feedback, concerns and ideas on the boulevard, and take an active role in establishing a temporary transportation installation. Through canvassing efforts, sharing on social media and connecting with the civic groups, JSC facilitated 3 successful public workshops in early fall, and is actively working with the surrounding community and civic associations to ensure the successful impact of the installation in Fall 2023.
The communities in Northwest Wilmington run long and deep. The neighborhoods, with most of the housing developed between 1900-1930, served as a bedroom community for workers employed by the expanding industries and businesses located in
113
STOP + HOSPITAL COMMUNITY Garden Community Welcome DURING NON-SCHOOL HOURS
ChangeLab Solutions is a nonprofit organization that provides legal information on matters relating to public health. The legal information in this document does not constitute legal advice or legal representation. For legal advice, readers should consult a lawyer in their state. This publication was supported by the Grant or Cooperative Agreement Number 5U38OT000141-02 awarded to ChangeLab Solutions and funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services. © 2015 ChangeLab Solutions Learn more at www.changelabsolutions.org/shared-use
Figure 3. Benefits of Shared Use, Change Lab Solutions.
Downtown Wilmington and along the Christina and Brandywine Riverfronts.2 Many of the current homeowners have lived in this area for years, some moving only a few blocks away, whether they needed to expand or had to downsize later in life. Some residents who have experienced times of unrest or development might take longer to trust a ‘new’ organization, especially in disinvested communities. This has driven the organization to grow low and slow - learning, listening and showing up, over and over - and approaching the work through a trauma-informed lens. It is essential for community-building and engagement efforts to be realistic and transparent about new opportunities and to be truthful about what we are offering.6 Since becoming staffed in 2021, the past two years have been, and continue to be, critically important to build trust between JSC and the community it serves.
Our work continues to be laid out in front of us and we have much to do. Whether we’re building systems of sustainability through the infrastructure of our community hub, or working to decrease vacant housing in our neighborhoods, we must continue to evaluate our work, how it’s delivered, who is driving it, and what the impact is on the community. It is imperative that JSC continues to show up and support transformative partnerships, whether organizational or informal, that directly impact positive physical and socioeconomic place-based changes. Empowering the resourcefulness of Northwest Wilmington will continue to be at the forefront of our work, and so will the community we serve. Ms. August may be contacted at aaugust@jeffersonstreetcenter.org
REFERENCES
1. Kelman, I., Merilainen, E., Peters, L., & Shannon, G. (2021). Toward resourcefulness: pathways for community positive health. Sage Journal, 29(3).
https://journals.sagepub.com/doi/full/10.1177/17579759211051370
2. University of Delaware. (2017). Washington Heights blueprint revitalization plan. Retrieved from https://www.bidenschool.udel.edu/ccrs/content-sub-site/ Documents/Washington%20Hts%20Blueprint%20Community%20 Revitalization%20Plan%20(1).pdf
3. Space Coalition. (2019, Feb). How to hub: Community hub development toolkit.
https://d3n8a8pro7vhmx.cloudfront.net/socialplanningtoronto/ pages/2484/attachments/original/1612818074/How_to_Hub_Toolkit_ Feb_2019_Electronic_Version.pdf?1612818074
4. Internal Revenue Service. (2020). Zip code data by individual state or area.
https://www.irs.gov/pub/irs-soi/20zp08de.xlsx
5. City of Wilmington. (2020). Wilmington 2028: A comprehensive plan for our city and communities. https://www.wilmingtonde.gov/home/ showpublisheddocument/8490/637188241765600000
6. Arena, O., Falkenburger, E., & Wolin, J. (2018). Traumainformed community building and engagement.
https://www.urban.org/sites/default/files/publication/98296/traumainformed_community_building_and_engagement.pdf
114 Delaware Journal of Public Health - June 2023


Use crosswalks, carry a flashlight and be aware when crossing Delaware’s busy roads. ArriveAliveDE.com/Walk-Smart WALK BRIGHT 115
Leveraging Delaware’s Public Health Resources to Mitigate Spread of Communicable Diseases in Congregate Settings
Laura A. Strmel, M.P.A.
Vulnerable Populations Planner IV, Emergency Medical Services and Preparedness Section, Office of Preparedness, Delaware Division of Public Health
Diane Hainsworth, B.S.N./B.A. Section Chief, Emergency Medical Services and Preparedness Section, Delaware Division of Public Health
Muriel Gillespie
Disaster Coordinator, Delaware Department of Health and Social Services
Sydney Kappers, B.S.
Congregate Testing Coordinator, Emergency Medical Services and Preparedness Section, Delaware Division of Public Health
Mollee Dworkin, M.S.
Epidemiologist II, Emergency Medical Services and Preparedness Section, Office of Preparedness, Delaware Division of Public Health
ABSTRACT
While resources available to public health entities increased during the COVID-19 pandemic, the need to focus mitigation efforts on Delaware’s most vulnerable citizens was evident. The higher risk of community-spread and complications resulting from COVID-19 associated with individuals residing in congregate settings such as homeless shelters and encampments prompted the Delaware Division of Public Health to leverage existing and new resources to provide technical assistance, education and to build valuable partnerships with community-based homeless service providers to reduce the public health threat to those experiencing homelessness.
INTRODUCTION
From 2020 to 2022, the number of people experiencing homelessness in Delaware more than doubled, according to the Housing Alliance of Delaware’s annual point-in-time count. On the evening of February 23, 2022, the annual count yielded 2,369 people experiencing homelessness in Delaware, compared to count of 1,165 individuals conducted in 2020.1
Homeless people are vulnerable to disease due to their increased exposure to environmental risk factors. This presents specific challenges to mitigating infectious disease spread within emergency shelters and encampments.
The Delaware Department of Health and Social Services (DHSS), Division of Public Health (DPH), Emergency Medical Services and Preparedness Section (EMSPS) focused its resources and efforts to protect homeless vulnerable populations from COVID-19. Following the state’s vaccination response, in 2021 EMSPS applied for the Centers for Disease Control and Prevention (CDC) grant, Detection & Mitigation of Covid-19 in Homeless Service Sites and Other Congregate Living Facilities Project E: Emerging Issues, supported through the American Rescue Plan Act of 2021. In July 2022, CDC awarded DPH a two-year $450,000 grant aimed at mitigating the spread of COVID-19 and communicable diseases that are prevalent in congregate settings. The grant award allowed DPH’s Office of Infectious Disease Epidemiology (OIDE) and EMSPS to develop a comprehensive workplan supporting the homeless and included homeless service sites, encampments, and group homes (Figure 1).
According to the CDC, the risk of COVID-19 transmission is higher in these settings compared with the general population. In addition, there is a high prevalence of certain medical conditions associated with severe COVID-19 among people experiencing homelessness and among people who are incarcerated, increasing the risk for severe outcomes from COVID-19 in these populations.2
This project aligned with DPH’s mission to protect and promote the health of all people in Delaware and the overall DHSS mission to improve the quality of life for Delaware’s citizens by promoting health and well-being, fostering self-sufficiency, and protecting vulnerable populations. Delawareans living in congregate shelters represent a targeted vulnerable population due to increased environmental risk factors for spreading infectious disease.
HOMELESSNESS INTERVENTIONS TO MITIGATE SPREAD OF COVID-19 IN DELAWARE
The term ‘homeless service sites’, as defined by the CDC, includes emergency night shelters, day shelters, meal service sites, transitional housing, permanent supportive housing sites, and other sites that provide services to people experiencing homelessness. The term ‘encampment’ is defined as an outdoor location not intended for human habitation where at least one person is residing and may also include locations where people experiencing unsheltered homelessness gather during the day.3 Encampments in Delaware, specifically in rural Sussex County, increased from 2020 to 2021. Causes potentially attributed to the increase include rising rental rates and a shortage of affordable housing prior to and during the pandemic. An additional challenge is the limited resources and capacity of organizations supporting those experiencing homeless.4
116 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.022
EMSPS acknowledged early in the planning process the long-standing challenge for DPH to effectively engage non-state regulated agencies and other charitable organizations supporting individuals and families experiencing homelessness. Proposed activities were based foundationally on increased engagement and interaction with existing and new community-based partners to meet the overall goal of mitigating the spread of COVID-19, and by default, reducing the spread of other communicable infectious diseases common in congregate settings.
Three main high-engagement objectives guided the workplan’s development. First, EMSPS would consistently complete the resource request process for over-the-counter COVID-19 testing kits on behalf of community-based homeless sheltering partners during the Public Health
Emergency. Second, EMSPS would purchase, assemble, and deliver DPH personal hygiene care packages to homeless sheltering partners for distribution to individuals experiencing homelessness. Third, DPH would develop and disseminate information and sanitation supply toolkits to homeless sheltering partners. These toolkits would include Best Management Practices (BMPs) on how to effectively engage with DPH for infectious disease testing and reporting. Additional training toolkits focused on the implementation of a train-the-trainer model education for staff and volunteers on preventative sanitation measures to mitigate spread of respiratory diseases and diseases spread by fomites (surfaces or objects that are likely to carry diseases or transmit it), foodborne or waterborne, blood or bodily fluids.

117
Figure
1. Delaware Communicable Disease Mitigaton Workflow for Congregate Settings, 2022
STATEWIDE EFFORT OF PARTNER ENGAGEMENT
In October of 2021, DPH began the workplan development required for submission of the grant. Provider networks that support encampments, food pantries, and soup kitchens were included on the list of engagement partners in addition to the list of traditional emergency shelters within Delaware.
Leading the list of activities from the workplan was creating a full-time COVID-19 mitigation coordinator position to coordinate resources, develop strategies, and support relationships with homeless shelters, encampments, and service providers. This new position of Congregate Testing Coordinator was created and hired to oversee the coordination of testing within all congregate settings, order supplies, and maintain relationships with facilities. Additional existing clinical support staff facilitated testing within all congregate settings.
Implementation of regular COVID-19 screening and diagnostic testing for homeless service site clients, homeless service site staff, people experiencing unsheltered homelessness, and outreach staff started with assessment of current provider networks. The Coordinator assessed the various sites and identified gaps within existing programs. At the time of the initial assessment, there were at least four State Service Center voucher program hotels identified; the New Castle County Hope Center, a referral program based in a former Wilmington hotel; approximately 20 statewide homeless shelters operated by organizations such as the Salvation Army and Catholic Charities; at least six known homeless encampments; and multiple Code Purple shelters in each county. Clinical Support staff was responsible for facilitating testing and providing education to facility staff. Both the Coordinator and the Clinical Support maintained working relationships with the facilities and State stakeholders as needed. Currently, the State has Incident Response Teams or a Strike Team to re-deploy to assist with onsite testing and client education. Strike Team deployment is an on-going resource provided to congregate settings and homeless service providers.
To respond to COVID-19 and other infectious diseases that may co-exist with COVID-19 within this population, the Congregate Testing Coordinator and DHSS Disaster Coordinator established and supported formal partnerships between DPH and other health departments, homeless service providers, health care providers, and relevant community organizations. These partnerships will continue throughout the duration of the grant, and beyond to address community needs.
Through the grant, DPH epidemiologists have access to various systems that allow for surveillance of people experiencing homelessness, including syndromic surveillance data to track Emergency Room visits associated to COVID-19 and other priority infectious diseases of interest among people experiencing homelessness. DPH established and supported processes to collect and report indicators on housing status and homelessness on COVID-19 and other infectious disease case report forms and in appropriate data collection systems. Additionally, epidemiologists created and developed a list of priority infectious diseases that may affect the population of interest.
To enable the swiftest response to cases and outbreaks, processes to share data with health departments, homeless service providers, and relevant public health agencies (including CDC) were established and supported. DPH epidemiologists developed a checklist to empower and guide shelter staff as they identify, mitigate, and report on sporadic or cluster-related cases; shelter clients received COVID-19 educational materials in multiple languages. Processes were established to allow for the timely reporting of cases, referrals to temporary housing and other related services, and communication related to clearance of cases. DPH epidemiological points of contact for COVID-19 and other infectious diseases was communicated. One mitigation activity was to support facility efforts to implement distancing and reduce overcrowding by decompression. The coordinator worked with the shelters to ensure that facilities were following CDC guidelines for congregate sheltering for social distancing. In addition, on-site technical assistance for implementing these guidelines was provided. DPH developed infection prevention and personal sanitation kits and provided them to partners for distribution to encampments, homeless shelters, and other homeless service sites. The kits included educational materials to underscore the importance of personal hygiene and sanitation measures that mitigate transmission. Clients may not otherwise have had access to such materials. Since homeless shelters rely on cleaning and sanitation supply donations, gaps in disinfection and sanitation processes may limit their ability to effectively mitigate COVID-19 transmission. Based on this assessment, the Congregate Testing Coordinator procured cleaning and sanitizing supplies for homeless service sites or encampments. Furthermore, best practices for cleaning and sanitation were developed, and educational materials on disinfection was provided to the shelters as references. Binders were created from current best practices and distributed to sheltering partners during grant implementation period.
DPH epidemiologists developed procedures to assist shelter staff identify, mitigate, and report on sporadic or cluster-related cases and promptly conduct contact tracing activities. OIDE quickly and efficiently responded to outbreaks in homeless shelters, encampments, and other congregate living facilities, including supporting individual-level or location-based contact tracing. As needed, during an outbreak, testing stations will be were set up at encampments. OIDE developed three BMP guides for homeless sheltering partners to utilize: (1) Identifying, mitigating, and reporting of sporadic or cluster-related cases; (2) Contact Tracing and Clearance of Cases; and (3) Best Management Practices for Cleaning and Disinfecting Your Facility.
EFFECTIVENESS OF HOMELESSNESS INTERVENTIONS STILL TO BE DETERMINED
DPH achieved its planned milestones and timelines from the initial workplan to include hiring of full-time Congregate Testing Coordinator. While there have been fewer reported cases of COVID-19 and other communicable diseases specific to homeless individuals, as of mid-March
2023 DPH had not yet conducted an interpretation of data as a result of these interventions. No adverse effects or unintended negative consequences to these intervention activities have been reported.
118 Delaware Journal of Public Health - June 2023
Leveraging existing and new resources from the grant award led to increased engagement between DPH and homelessness support providers and networks, which helps to lay the groundwork for continuing the relationship with homeless shelters.
Sustainability will rest upon utilization of the best practice resources provided to these partners. EMSPS plans to continue to aid in infectious disease mitigation, provide support during outbreaks, and further develop these new partnerships to promote the health of those experiencing homelessness.
Public health engagement with homelessness service providers and networks is critical to successful infectious disease mitigation efforts. Delaware partners were provided resources and best practices to reduce spread of COVID-19 and other communicable infectious diseases common to congregate settings at the base level, within their own facilities and operations. Continued engagement and promotion of best practices with community-based partners remains the responsibility of state and local health departments to address infectious disease control within vulnerable populations.
Ms. Strmel may be contacted at laura.strmel@delaware.gov
REFERENCES
1. Housing Alliance of Delaware. (2022). 2022 Point in Time Summary. Retrieved from: https://www.housingalliancede.org/_files/ ugd/9b0471_8845d32c539342758944d04329e8c07c.pdf
2. Center for Disease Control and Prevention. (n.d.). Interim guidance on unsheltered and coronavirus disease 2019 (COVID19) for homeless providers and local officials. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/community/homelessshelters/unsheltered-homelessness.html
3. Center for Disease Control and Prevention. (2021). Guidance for the use of supplemental funding (August 2021) for CK191904 ‘Detection & mitigation of COVID-19 in homeless service sites and other congregate living facilities’ through the American Rescue Plan Act of 2021. Retrieved from: https://www.cdc.gov/ncezid/dpei/pdf/detect-mitigate-covidhomeless-508.pdf
4. MacArthur, R. (2021, Dec 10). Number of homeless families is growing. Cape Gazette. Retrieved from: https://www.capegazette.com/article/number-homeless-familiesgrowing/231529
DATE
NAME
our office highly recommends that you visit healthydelaware.org/diabetes
There, you will find available educational programs and classes you can enroll in. They will help you to:

• understand the disease and how to manage it
• develop an action plan best for you
• make choices about treatment and medications
• develop healthier behaviors and eating habits
• live well and possibly beat the disease
Courses are taught at local hospitals, healthcare facilities and community settings with convenient times and locations. View them at healthydelaware.org/diabetes
Sponsored by:
DELAWARE
Division of Public Health
Diabetes and Heart Disease Prevention and Control Program

HEALTH AND SOCIAL SERVICES
119
To help you better manage your diabetes or prediabetes,
From the Delaware Division of Public Health April 202
Clothesline Project raises awareness
Survivors of sexual assault expressed their emotions on shirts to be displayed throughout Delaware during April, Sexual Assault Awareness and Prevention Month.
The Clothesline Project began on Cape Cod, Massachusetts in 1990 with a display of 31 shirts decorated by victims of sexual violence.
The Division of Public Health (DPH) Office of Women’s Health (OWH) is collaborating with the Delaware Alliance Against Sexual Violence (DAASV) and other community partners to bring the Clothesline Project to Delaware. The University of Delaware (UD), Delaware State University (DSU), and CAMP Rehoboth are working with survivors of violence to create artistic testimony to violence.
According to DAASV, the Clothesline Project will be on display at the following locations:
• Through April 28 at DSU, Martin Luther King, Jr. Student Center, 1200 N. Dupont Highway, Dover, DE 19901.
• April 26 from 12:00 p.m. to 2:00 p.m., at the Blue Hens CARE Peer Educators Inaugural Spring Support Fair, Central Green, UD campus, Newark, DE 19711.
More information about the Clothesline Project can be found at https://www.theclotheslineproject.org/

For more information about OWH’s partnership, contact Karen.McGloughlin@delaware.gov. Learn about DPH’s work to prevent gender-based violence prevention at https://dhss.delaware.gov/dhss/dph/mh/owhgbvp.html.
Support and resources for victims of violence are listed on the Victim Rights Task Force website at delawarevictimservices.org



Cultural Competency Training offered May 11 and 12 in Dover
In May, the Mid-Atlantic Association of Community Health Centers is hosting an in-person Cultural Competency Training at the Modern Maturity Center, located at 1121 Forrest Avenue in Dover. The same content will be offered on two dates:
• Thursday, May 11, 2023, 12:00 p.m. to 4:00 p.m.
• Friday, May 12, 2023, 8:00 a.m. to 12:00 p.m. Jennifer R. Daniels, PhD will lead an interactive workshop focused on the impacts of microaggressions in health care. Participants will learn how explicit and implicit biases contribute to microaggressions as well as interventions and strategies to manage and mitigate microaggressions in support of a healthy, inclusive workplace.
This is a free event and includes lunch. Participants need to be present for the entire course and complete a course evaluation to receive three Continuing Nursing Education credits. Register at https://www.machc.com/upcomingevents
Primary Care Recruitment Conference is May 24 at Modern Maturity Center
The Annual Primary Care Provider Recruitment Conference is being held on May 24, 2023 at the Modern Maturity Center, located at 1121 Forrest Ave. in Dover. The event runs from 9:00 a.m. to 3:00 p.m. and is designed for health professionals who are responsible for health provider and staff workforce recruitment and retention.

The conference is sponsored by the Division of Public Health’s Bureau of Health Planning & Resources Management. Featured topics include State and federal incentive programs that support recruitment and Delaware policy initiatives to support primary care
The no-cost event includes coffee and buffet lunch. Register at https://wams.wufoo.com/forms/2023annual-primary-care-recruitment-conference/.

120 Delaware Journal of Public Health - June 2023
The Clothesline Project
Recruitment tools support medical community’s search for providers

To improve access to care, the Division of Public Health (DPH) Bureau of Health Planning and Resources Management (BHPRM) recruits medical professionals to live and work in Delaware.
Recently BHPRM, in conjunction with the Middletown-based Epic Marketing Consultants Corporation, developed a recruitment video. The video features health care professionals from across the state, including Lieutenant Governor Bethany Hall-Long, MSN, PhD; Megan Werner, MD, MPH, FAAFP, Westside Family Healthcare; and Karyl Rattay, MD, MS, former DPH director Any organization – including hospitals, private practices, Federally Qualified Health Centers, and state agencies – can use the video and a digital packet to attract physicians, nurses, and other specialized health care professionals.
As Delaware’s population grows and becomes more diverse, health care providers are seeing an increase in demand for a range of services and assistance in various communities. Delaware seeks highly qualified providers in the areas of family practice, pediatrics, internal medicine, gynecology/obstetrics, dentistry, and psychiatry to work in its federally designated Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs).
Providers work in shortage areas for two or more years to reduce loan debt and for other financial incentives They work through programs such as the National Health Service Corps, the Nurse Corps Scholarship Program, the Delaware State Loan Repayment Program, The National Rural Recruitment and Retention Network for Healthcare Professionals (3RNet), and the Conrad State 30/J-1 Visa Waiver program High school graduates can apply for scholarships. Regional medical colleges reserve spaces for Delaware applicants. Access the recruitment video at https://www.youtube.com/watch?v=Y8Kr3uRQto4. DHSS links medical professionals with the programs best suited to their needs and interests. Contact the DPH Office of Primary Care at 302-741-8599 or https://dhss.delaware.gov/dph/hsm/bhprmhome.html.
Medical professional resources
Medical professionals living in Delaware may be eligible to receive financial benefits and state loan repayment opportunities that position them to get the best return on their investment and can help remunerate medical education expenses.
• The Delaware State Loan Repayment Program provides educational debt relief to cover a portion of government and commercial loans incurred during one’s health professional education, up to $50,000 annually.
• The Delaware Health Care Provider Loan Repayment Program is a state-sponsored educational debt relief program for medical providers, awarding up to $50,000 annually to eligible health care professionals.
• The National Health Service Corps (NHSC) provides practical experience to physicians around the country and offers financial incentive. The NHSC Loan Repayment Program and the NHSC Scholar Program offer tax-free funding for educational expenses.

• The Conrad State 30/J-1 Visa Waiver program allows foreign medical graduates who have been admitted to the U.S. for medical training to remain in Delaware. Up to 30 J-1 physicians per year are accepted into the waiver program in Delaware, where they serve in Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs)
• The Delaware Institute for Dental Education and Research provides Delaware residents with an opportunity to receive quality education and training at Temple University Kornberg School of Dentistry. Each year five admission slots are reserved for Delaware applicants.
• The National Rural Recruitment and Retention Network for Healthcare Professionals (3RNet) posts medical job vacancies for free.
121 The DPH Bulletin – April 2023 Page 2 of 2
Social Capital from Online Social Media is Associated with Visiting a Healthcare Practitioner at Least Once a Year Among College Students
Joshua Fogel, Ph.D. and Ashaney Ewen, B.S., B.B.A. Brooklyn College, Brooklyn, NY USA
ABSTRACT
Objective: Social capital is positively associated with healthcare access such as healthcare practitioner visits. There does not appear to be any literature on social capital through online social media and its association with healthcare access such as healthcare practitioner visits. This paper studies the relationship between social capital through online social media use and healthcare practitioner visits. Methods: Data were analyzed from 663 participants in New York City in 2017 with exposure to social media prescription medication advertisements from social media (e.g., Facebook, Twitter, LinkedIn, Instagram, YouTube). The main predictor variable was visiting a healthcare practitioner at least once a year. Outcome variables were bonding social capital and bridging social capital from online social media. Results: Those who visited a healthcare practitioner at least once a year had greater mean bonding social capital and bridging social capital from online social media than those who did not visit a healthcare practitioner at least once a year. Multivariate linear regression analyses showed a similar pattern for not visiting a healthcare practitioner at least once a year (bonding social capital: b=-5.31, SE=1.68, p=0.002; bridging social capital: b=-3.27, SE=1.55, p=0.04). Conclusions: Government organizations, healthcare practitioners, and healthcare organizations should continue marketing and disseminating health education for young adults through online social media. This public health online social media health education is likely to be considered bonding social capital and/or bridging social capital by young adults and this may be associated with more young adults visiting healthcare practitioners at least once a year.
INTRODUCTION
A commonly used definition for social capital is features of social organizations where individuals work together to improve society’s efficiency through trust, social networks, and norms.1 Greater levels of trust from these social organizations are associated with greater efficiency.2 Social capital is not only in face-to-face settings but also in online settings where social capital is positively associated with attitudes about that online environment.3
Bonding and bridging are two categories of social capital. Bonding social capital is defined as the relationships between people who share close bonds with each other such as close relatives and friends.1 Bridging social capital is defined as the relationships between people who share loose ties with each other such as casual friends and coworkers.1 Bonding and bridging social capital can occur online as well as in person. Social media networking websites are associated with increased bonding social capital in an online social media environment and are associated with increased bridging social capital in an offline inperson environment.4 Bonding and bridging do not always have different associations for a particular area of focus. Both bonding and bridging can be present and have similar associations for a particular area of focus.5 In the literature review below we review the relationship of social capital with the three topics of selfperceived health, health care access, and social media.
Social Capital & Self-perceived Health
Bonding and bridging social capital are studied regarding selfperceived health. Bonding social capital is consistently positively associated with better self-perceived health.6–9 Bridging social capital has differing findings regarding its association with better self-perceived health. Some report that bridging social capital is positively associated with better self-perceived health,9 some report that bridging social capital is negatively associated with better self-perceived health,6,7 and some report that bridging social capital does not have any association with self-perceived health.7 This literature suggests that social capital is relevant for understanding health issues experienced by people.
Social Capital & Healthcare Access
In addition to the relevance of social capital for self-perceived health, it would be useful to understand if social capital impacts healthcare access. One can have a health concern but not necessarily have access to healthcare to treat the health concern. For general healthcare access, social capital of participating in social organizations was positively associated with Chinese migrants having public health services of established health records and receipt of health education information.10 For physician visits and days hospitalized, there are mixed findings. Social capital of trust and people willing to help each other were each not associated with elderly Japanese refraining from visiting a doctor when medical care was needed.11 A broad measure of social capital was negatively associated with doctor visits and days hospitalized during the last two years of a person’s life
122 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.023
among elderly Medicare patients in the United States.12 Social capital of belonging to the community was positively associated with Canadians having general practitioner physician visits and negatively associated with nights hospitalized.13 Social capital of frequency of religious service attendance, tangible social support, and affection each had mixed findings where one analysis showed a negative association with general practitioner physician visits and another analysis showed no association.14 Among Canadian immigrants, social capital of frequency of religious service attendance, community belonging, tangible social support, and affection were each not associated with general practitioner physician visits.15 Among Canadian non-immigrants, social capital of tangible social support was positively associated with general practitioner physician visits, social capital of affection was negatively associated with general practitioner physician visits, and social capital of frequency of religious service attendance and community belonging were each not associated with general practitioner physician visits.15
Social Capital and Online Social Media
In addition to the relationship of social capital with health and healthcare access, social capital can impact communication through online social media. A systematic review reports that the most frequent reason for online social media use is to seek and share health-related information.16 Another systematic review on social media use in healthcare reports that all relevant retrieved articles reported that patients used social media for information support of useful or needed health information.17 Communication on online social media is positively associated with both bonding and bridging social capital.18 General use of online social media is not associated with social capital in the community while online social media use for news is positively associated with social capital in the community.19 In longitudinal analyses, online social media social capital more strongly predicts offline social capital than offline social capital predicts online social media social capital.20
Online Social Media
There are a number of points to keep in mind when studying online social media. First, content on online social media is not always accurate and this inaccurate content can be called “fake news.” The fake news content often appears as credible. Confirmation bias of the attitude that the news is consistent with one’s worldview is the main factor for acceptance of fake news.21 Second, advertisements on online social media can have enhanced acceptance if the advertisements are targeted to be congruent with the consumer’s psychological personality.22 Third, the influence of online social media may differ depending upon the culture of the area studied. For example, those that identify most with mainland American culture have a greater network size on online social media and more often share photos on online social media than those who identify most with Asia-Pacific culture.23
The literature reviewed above shows that 1) bonding social capital is positively associated with better self-perceived health while the pattern for bridging social capital is mixed for its association with self-perceived health, 2) there are mixed findings for the association of social capital with healthcare access such as physician visits, and 3) online social media is positively associated
with social capital. This literature suggests that social capital is potentially relevant for understanding self-perceived health issues experienced by people that can involve the need for healthcare access. However, there does not appear to be any literature on social capital through online social media and its association with healthcare access such as healthcare practitioner visits. From a theoretical perspective, it would be useful to understand the relationship of social capital through online social media and healthcare access. Online social media use is a common activity. Social capital through online social media may have a different pattern for healthcare access than from what has been previously studied for the relationship of social capital with healthcare access. The findings from this study can benefit future studies as future research regarding online social media and healthcare access can use this study as the foundation for what is known about the topic. In addition to theory, there is applied relevance. It is a common practice to see a healthcare practitioner for an annual physical examination24 or annual wellness visit.25 As social capital can impact healthcare access, it would be useful to understand whether social capital through online social media is associated with healthcare access of this common practice of an annual visit to a healthcare practitioner.
Our overall research question is whether bonding or bridging social capital through online social media is positively associated with an annual visit to a healthcare practitioner (whether primary care or specialty care) among college students. It is important to study both types of social capital. These are two distinct types of social capital that potentially can have different associations with an outcome. Also, previous research on social capital often studies both types of social capital.6,7,9 First, we hypothesize that bonding social capital through online social media is positively associated with an annual visit to a healthcare practitioner. Second, we hypothesize that bridging social capital through online social media is positively associated with an annual visit to a healthcare practitioner.
METHODS Participants
The study design was a cross-sectional survey using convenience sampling. This study design was chosen as this allowed the researchers to access a large sample size of potential respondents open minded to completing a survey. There were 950 undergraduate college students from a New York City public college who were asked to complete the survey. All undergraduate students were eligible to complete the survey and there were no formal exclusion criteria. Of these students, 41 declined to participate and 88 surveys were considered not valid due to substantial non-completion of content. The response rate of 86.4% for the 821 completed surveys was calculated as 821/950*100%. We then excluded 23 students above age 35 to allow for a more consistent traditional college-age sample. We also excluded 131 individuals who had no exposure to prescription medication advertisements on social media and four people who did not answer the social capital questions. Data were analyzed from 663 participants who indicated exposure to prescription medication advertisements on social media from one or more of the following social media platforms of Facebook,
123
Twitter, Snapchat, Instagram, Google+, Tumblr, Pinterest, LinkedIn, and YouTube. We included those with exposure to prescription medication advertisements on social media as these advertisements encourage consumers to discuss the prescription medication advertised with their healthcare professional. This is also a sample that is aware of and has exposure to healthcare topics on social media. Such a sample would potentially be useful for generalizing to understand the impact of social media with other types of healthcare focused advertisements and for consumers visiting a healthcare professional.
The sample obtained is representative of the college population as the race/ethnicity percentages of the 663 participants in our sample are similar to the race/ethnicity percentages reported by the college for the college population. The anonymous surveys were completed in classrooms and lecture halls where students were asked to complete the paper survey and then surveys were distributed to all students present. The principal investigator trained the one student research assistant on survey data collection. Some data collection sessions had both the principal investigator and student research assistant present for data collection. Most of the data collection sessions were conducted independently by the student research assistant. Students typically had no prior relationship with the principal investigator or student research assistant and could easy decline to participate. Informed consent was obtained. Ethical approval to conduct this study was obtained from the college Institutional Review Board and was conducted consistent with the Declaration of Helsinki. Surveying occurred in September and October 2017.
Measures
Demographic variables consisted of age (years), sex (man/ woman), and self-reported race/ethnicity (white, African American, Hispanic, Asian/Asian American, South Asian [India, Pakistan, surrounding areas], other). These variables were included as these are important variables for understanding sample characteristics and are typically included in studies conducted in the United States. Self-perceived health had categories of excellent, very good, good, and fair/poor. Fair and poor were grouped together because there was a small number of participants in those categories. Healthcare visit information was obtained by asking about the last time participants saw a doctor, a nurse practitioner, or a physician’s assistant where participants talked about a health condition or concern of their own. Participants were informed to exclude emergency room visits from this question. Healthcare visit had two categories of either less than or equal to once a year or greater than once a year. The one year dividing point was chosen as it is a common practice to see a healthcare practitioner for an annual physical examination24 or annual wellness visit.25
Outcome Variables
Social Capital
Social capital was measured with a scale measuring online social capital of bonding and bridging.26 The measure has several strengths. It was developed from a sample of people from all the states in the United States which includes our current sample of those from similar cultural background in the United States. The scale is reliable and valid with the original development study reporting Cronbach alpha reliability for the bonding scale of 0.90 and for the bridging scale of 0.84. The scale is also used by others to measure online social capital (e.g.25).
Bonding
The bonding scale had 10 items. A sample item is, “There are several people on my online social network that I trust to help solve my problems.” The response scale ranged from 1=strongly disagree to 7=strongly agree. The total score was calculated by adding all 10 items. We changed two reversed items to be in the same direction as the other items. We also modified “online” to “on my online social network.” There were six people that omitted one item and one person that omitted two items. The mean for each person was used to impute the missing values to allow for the scale to be included for that person.
Bridging
The bridging scale had 10 items. A sample item is, “Interacting with people on my online social media network makes me feel like part of a larger community.” The response scale ranged from 1=strongly agree to 7=strongly disagree. The total score was calculated by adding all 10 items. We modified “online” to “on my online social network.” There were 14 people that omitted one item. The mean for each person was used to impute the missing values to allow for the scale to be included for that person.
Statistical Analysis
Descriptive statistics of mean and standard deviation were used for the continuous variables. Percentage and frequency were used for the categorical variables. Analysis of variance compared healthcare visits with the social capital measures of bonding and bridging. Multivariate linear regression analyses were conducted for bonding social capital and bridging social capital. All analyses used IBM SPSS Version 25.27 All p-values were twotailed with alpha level for significance at p<0.05.
RESULTS
Table 1 shows the sample characteristics. The mean age was slightly above 22 years and the percentage of women was slightly more than half. In terms of race/ethnicity, slightly less than one-third of the sample was white. The second-largest racial group was Asian Americans who were slightly more than onefifth of the sample. Almost half of the sample perceived their health as very good whereas less than one-tenth of the sample believed they were in fair/poor health. Lastly, 15.7% visited their healthcare practitioner less frequently than once a year.
Cronbach alpha reliability for the bonding scale was 0.94 and for the bridging scale was 0.93.
Table 2 shows the mean comparison between healthcare visits and social capital from online social media. In both bonding and bridging social capital, those who visited a healthcare practitioner at least once a year had higher mean scores than those who did not visit their healthcare practitioner at least once a year.
Table 3 shows the linear regression analysis for bonding social capital from online social media. Those who visited their healthcare practitioner less often than once a year were significantly associated with lower levels of bonding social capital. In addition, higher age was associated with significantly lower levels of bonding social capital.
124 Delaware Journal of Public Health - June 2023
Table 4 shows the linear regression analysis for bridging social capital from online social media. Those who visited their healthcare practitioner less often than once a year were significantly associated with lower levels of bridging social capital. Higher age was significantly associated with lower levels of bridging social capital. Asian Americans were significantly associated with greater levels of bridging social capital. Lastly, those who perceived their health as very good were significantly associated with greater levels of bridging social capital.
DISCUSSION
Consistent with our hypotheses, those who visited a healthcare practitioner at least once a year had greater bonding and bridging social capital from online social media than those who did not visit a healthcare practitioner at least once a year. In addition, the multivariate analyses showed that higher age was significantly associated with lower levels of both bonding and bridging social capital from online social media. Asian Americans were significantly associated with greater levels of bridging social capital from online social media. Lastly, those who perceived their health as very good were significantly associated with greater levels of bridging social capital from online social media. We found that those who visited a healthcare practitioner at least once a year had greater bonding and bridging social capital from online social media than those who did not. We are not aware of any studies on bonding or bridging social capital as it relates to yearly healthcare practitioner visits. There are mixed findings regarding other types of social capital as it relates to health care practitioner visits. Some studies report general social capital12 and religious social capital15 are not associated with healthcare practitioner visits. However, another study shows that social capital of belonging is positively associated with general practitioner visits.13 Our findings for bonding and bridging social
125
Variable Mean (SD) or # (%) Demographics Age (years) 22.3 (3.70) Sex (women) 348 (52.5) Race/ethnicity White African American Hispanic Asian/Asian American South Asian Other Missing 204 (30.8) 89 (13.4) 100 (15.1) 142 (21.4) 59 (8.9) 67 (10.1) 2 (0.3) Health Self-perceived Health Excellent Very good Good Fair/Poor 122 (18.4) 283 (42.7) 210 (31.7) 48 (7.2) Healthcare Visit ≤ 1 year >1 year 559 (84.3) 104 (15.7) Note: SD=standard deviation
Table 1. Characteristics of the Sample
Variable ≤ 1 year Mean (SD) (n=559) >1 year Mean (SD) (n=104) p-value Bonding39.8 (15.89)33.8 (15.16)<0.001 Bridging 44.3 (14.34)40.2 (14.90) 0.01 Note: SD=standard deviation
Table 2. Mean Comparison Between Healthcare Visits and Social Capital From Online Social Media
Table 3. Linear Regression Analysis for Bonding Social Capital from Online Social Media
Variable b (SE)p-value Demographics Age (years) -21.15 (8.51) 0.01 Sex (women) 0.85 (1.14)0.46 Race/Ethnicity White African American Hispanic Asian/Asian American South Asian Other Reference 0.40 (1.84) 0.84 (1.77) 3.16 (1.61) 2.52 (2.19) 2.68 (2.05) 0.83 0.64 0.050 0.25 0.19 Health Self-perceived Health Excellent Very Good Good Fair/Poor Reference 3.11 (1.56) 0.35 (1.68) -2.72 (2.51) 0.046 0.84 0.28 Healthcare Visit (> 1 year)-3.27 (1.55) 0.04 Constant 69.47 (11.56)< 0.001 Note: b=unstandardized beta, SE=standard error
Table 4. Linear Regression Analysis for Bridging Social Capital from Online Social Media
Variable b (SE)p-value Demographics Age (years) -34.63 (9.18)< 0.001 Sex (women) -1.24 (1.23)0.31 Race/Ethnicity White African American Hispanic Asian/Asian American South Asian Other Reference -3.71 (1.98) -2.36 (1.91) 2.90 (1.74) 0.48 (2.36) -1.68 (2.22) 0.06 0.22 0.10 0.84 0.45 Health Self-perceived Health Excellent Very Good Good Fair/Poor Reference 1.52 (1.68) -2.39 (1.81) -3.72 (2.71) 0.37 0.19 0.17 Healthcare Visit (> 1 year) -5.31 (1.68) 0.002 Constant 87.58 (12.47)< 0.001 Note: b=unstandardized beta, SE=standard error
capital from online social media are similar to studies about social capital of belonging. We know from a related concept of social support, that co-worker social support is positively associated with doctor visits.28 We suggest that having a close connection with others through social capital from online social media is related to caring about one’s health and visiting one’s healthcare practitioner. This approach applies not only to close relationships through bonding social capital but also to relationships between other communities through bridging social capital.
We found that higher age was significantly associated with lower levels of bonding and bridging social capital from social media. A study of college students ages 18-25 shows that higher age is associated with increased levels of bonding and bridging social capital through social media.29 Communication with family and friends on online social networks and self-concept of friendship building on online social networks are each positively associated with social media use among college students in their early 20s.30 We suggest that the use of social media to foster social capital is more important among those in their early to mid 20s than to those in their late 20s and early to mid 30s.
We found that Asian Americans were significantly associated with greater levels of bridging social capital from online social media. Religious Asian American college students were positively associated with cross-racial interaction, a form of bridging social capital.31 Our findings among all Asian Americans for online social media are similar to this pattern. Asian Americans typically prefer coping approaches that use a collectivistic orientation where the focus is on the group rather than on the individual.32 Bridging social capital is for those who share loose ties with each other. We suggest that Asian Americans due to their collectivistic approach have a greater desire to have higher levels of bridging social capital from online social media than other racial/ethnic groups. This collectivistic approach may be the mechanism for Asian American use of online social media as a platform to establish new bridging social capital relationships with others.
We found that those who perceived their health as very good were significantly associated with greater levels of bridging social capital from online social media. There are mixed findings for the association of bridging social capital with self-perceived health where some report a positive association,9 some report a negative association,6,7 and some report no association.7 Our findings for bridging social capital from online social media are similar to those who report a positive association. Buddies in online support groups are positively associated with goal attainment for health behaviors.33 We suggest that the mechanism of the positive association of perceiving their health as very good with bridging social capital from online social media is that this bridging social capital from online social media provides additional buddies that leads to a healthier lifestyle and greater perceptions of better health.
Limitations
This study has several limitations. First, this study was only from those college students ages 18-35 years and these patterns may differ among those from different age groups. Future research should study this topic among other age groups. Second, this study was collected with hard copy surveys. It is possible that an online method of data collection may have connected with different participants and there may have been different findings.
CONCLUSIONS AND PUBLIC HEALTH IMPLICATIONS
In conclusion, we found that those who visited a healthcare practitioner at least once a year had greater bonding and bridging social capital from online social media than those who did not visit a healthcare practitioner at least once a year. This study adds to theory that social capital through online social media is positively associated with healthcare access. This study has potential implications for public health policy. First, online social media marketing of healthcare visits may be of interest to young adults. Second, government organizations, healthcare practitioners, and healthcare organizations should continue marketing and disseminating health education for young adults through online social media. This public health online social media health education is likely to be considered bonding social capital and/or bridging social capital by young adults and this may be associated with more young adults visiting healthcare practitioners at least once a year. Regular visits to a healthcare practitioner are likely to result in a healthier population. This study has public health relevance to Delaware. Prior research in Delaware found that online social media was the most frequently used source for seeing advertisements, flyers, and/or infomercials for a public health campaign about protection from ticks and tick-borne diseases.34 Also, obesity, alcohol use, and cigarette use are topics that can be discussed at an annual healthcare visit. In Delaware, hospitalized adult patients differ by location regarding obesity, cigarette use, and alcohol use. Wilmington and Bear has almost half of patients hospitalized with obesity as compared to approximately one-third in Northwest New Castle County, and North Wilmington.35 Wilmington has more than one-quarter hospitalized with alcohol use disorder as compared to percentages of 16% or less in Bear, Northwest New Castle County, and North Wilmington.35 In New Castle County, the greatest portion of current cigarette smokers live in Wilmington.36 Public health online social media messages regarding obesity, alcohol use, and cigarette use can target different communities with messages tailored to the health concerns of the community. Lastly, Delaware has the My Healthy Community data portal that reports statistics and provides information on many health topics.37 Public health practitioners can track the location of searches for particular health topics and target different communities with online social media messages tailored to the particular health concerns of the community. A public health approach in Delaware with online social media messages targeted to different health needs of different communities can likely to be considered bonding social capital and/or bridging social capital by young adults in these communities. This may be associated with more young adults in Delaware visiting healthcare practitioners at least once a year and resulting in improved health for these young adults due to counseling and interventions by these healthcare practitioners.
Dr. Fogel may be contacted at joshua.fogel@gmail.com
126 Delaware Journal of Public Health - June 2023
REFERENCES
1. Bhandari, H., & Yasunobu, K. (2009). What is social capital? A comprehensive review of the concept. Asian Journal of Social Science, 37, 480–510.
https://doi.org/10.1163/156853109X436847
2. Gelderblom, D. (2018). The limits to bridging social capital: Power, social context and the theory of Robert Putnam. The Sociological Review, 66(6), 1309–1324.
https://doi.org/10.1177/0038026118765360
3 Yao, C.-Y., Tsai, C.-C., & Fang, Y.-C. (2015). Understanding social capital, team learning, members’ e-loyalty and knowledge sharing in virtual communities. Total Quality Management, 26(5-6), 619–631
https://doi.org/10.1080/14783363.2013.865918
4 Williams, J. R. (2019). The use of online social networking sites to nurture and cultivate bonding social capital: A systematic review of the literature from 1997 to 2018. New Media & Society, 21(11-12), 2710–2729
https://doi.org/10.1177/1461444819858749
5 Leung, M. R., Chin, J. J., & Petrescu-Prahova, M. (2016, August). Involving immigrant religious organizations in HIV/ AIDS prevention: The role of bonding and bridging social capital. Soc Sci Med, 162, 201–209
https://doi.org/10.1016/j.socscimed.2016.06.042
6. Chen, H., & Meng, T. (2015, November 16). Bonding, bridging, and linking social capital and self-rated health among Chinese adults: Use of the anchoring vignettes technique. PLoS One, 10(11), e0142300.
https://doi.org/10.1371/journal.pone.0142300
7. Gele, A. A., & Harsløf, I. (2010, March 17). Types of social capital resources and self-rated health among the Norwegian adult population. International Journal for Equity in Health, 9, 8. https://doi.org/10.1186/1475-9276-9-8
8 Novak, D., Emeljanovas, A., Mieziene, B., Štefan, L., & Kawachi, I. (2018). How different contexts of social capital are associated with self-rated health among Lithuanian high-school students. Global Health Action, 11(1), 1477470
https://doi.org/10.1080/16549716.2018.1477470
9 Poortinga, W. (2012, March). Community resilience and health: The role of bonding, bridging, and linking aspects of social capital. Health & Place, 18(2), 286–295 https://doi.org/10.1016/j.healthplace.2011.09.017
10. Hou, Z., Lin, S., & Zhang, D. (2017, August 18). Social capital, neighbourhood characteristics and utilisation of local public health services among domestic migrants in China: A crosssectional study. BMJ Open, 7(8), e014224
https://doi.org/10.1136/bmjopen-2016-014224
11. Mizuochi, M. (2016, August 2). Social capital and refraining from medical care among elderly people in Japan. BMC Health Services Research, 16, 331.
https://doi.org/10.1186/s12913-016-1599-8
12. Williams, J. (2012). Geographic variations in health care utilization: Effects of social capital and self-interest, and implications for US Medicare policy. Socio-economic Review, 10, 317–342.
https://doi.org/10.1093/ser/mwr018
13 Laporte, A., Nauenberg, E., & Shen, L. (2008, October). Aging, social capital, and health care utilization in Canada. Health Economics, Policy, and Law, 3(4), 393–411
https://doi.org/10.1017/S1744133108004568
14 Nauenberg, E., Laporte, A., & Shen, L. (2011, November). Social capital, community size and utilization of health services: A lagged analysis. Health policy (Amsterdam, Netherlands), 103(1), 38–46.
https://doi.org/10.1016/j.healthpol.2010.12.006
15 Samek, D. A., Laporte, A., Nauenberg, E., Shen, L., & Coyte, P. C. (2012, August). The effect of social capital on the use of general practitioners: A comparison of immigrants and nonimmigrants in Ontario. Healthc Policy, 8(1), 49–66.
https://doi.org/10.12927/hcpol.2012.23022
16 Chen, J., & Wang, Y. (2021). Social media use for health purposes: Systematic review. Journal of Medical Internet Research, 12;23(5), e17917.
17 Smailhodzic, E., Hooijsma, W., Boonstra, A., & Langley, D. J. (2016, August 26). Social media use in healthcare: A systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Services Research, 16(1), 442.
https://doi.org/10.1186/s12913-016-1691-0
18. Chen, H.-T., & Li, X. (2017). The contribution of mobile social media to social capital and psychological well-being: Examining the role of communicative use, friending and selfdisclosure. Computers in Human Behavior, 75, 958–965
https://doi.org/10.1016/j.chb.2017.06.011
19. de Zuniga, H. G., Jung, N., & Valenzuela, S. (2012). Social media use for news and individuals’ social capital, civic engagement and political participation. Journal of ComputerMediated Communication, 17, 319–336
https://doi.org/10.1111/j.1083-6101.2012.01574.x
20. de Zuniga, H. G., Barnidge, M., & Scherman, A. (2017). Social media social capital, offline social capital, and citizenship: Exploring asymmetrical social capital effects. Political Communication, 34, 44–68
https://doi.org/10.1080/10584609.2016.1227000
21 Di Domenico, G., Sit, J., Ishizaka, A., & Nunam, D. (2021). Fake news, social media and marketing: A systematic review. Journal of Business Research, 124, 329–341
https://doi.org/10.1016/j.jbusres.2020.11.037
22. Matz, S. C., Kosinski, M., Nave, G., & Stillwell, D. J. (2017, November 28). Psychological targeting as an effective approach to digital mass persuasion. Proceedings of the National Academy of Sciences of the United States of America, 114(48), 12714–12719.
https://doi.org/10.1073/pnas.1710966114
23 Rosen, D., Stefanone, M. A., & Lackaff, D. (2010). Online and offline social networks: Investigating culturally-specific behavior and satisfaction. Proceedings of the 43rd Hawaii International Conference on System Sciences, Honolulu, January 5-8, 2010, 1-10.
24 Goroll, A. H. (2015, October 15). Toward trusting therapeutic relationships— In favor of the annual physical. The New England Journal of Medicine, 373(16), 1487–1489.
https://doi.org/10.1056/NEJMp1508270
127
25 Gorbenko, K., Metcalf, S. A., Mazumdar, M., & Crump, C. (2017, June). Annual physical examinations and wellness visits: Translating guidelines into practice. American Journal of Preventive Medicine, 52(6), 813–816.
https://doi.org/10.1016/j.amepre.2016.12.005
26. Williams, D. (2006). On and off the ’net: Scales for social capital in an online era. Journal of Computer-Mediated Communication, 11, 593–628
https://doi.org/10.1111/j.1083-6101.2006.00029.x
27 Corporation, I. B. M. (2017). IBM SPSS Statistics for Windows, Version 25. Armonk, NY: IBM Corporation.
28 Tamers, S. L., Beresford, S. A. A., Thompson, B., Zheng, Y., & Cheadle, A. D. (2011, July). Exploring the role of co-worker social support on health care utilization and sickness absence. Journal of Occupational and Environmental Medicine, 53(7), 751–757.
https://doi.org/10.1097/JOM.0b013e318223d42f
29. Kim, B., & Kim, Y. (2017). College students’ social media use and communication network heterogeneity: Implications for social capital and subjective well-being. Computers in Human Behavior, 73, 620–628
https://doi.org/10.1016/j.chb.2017.03.033
30 Sponcil, M., & Gitimu, P. (2013). Use of social media by college students: Relationship to communication and selfconcept. Journal of Technology Research, 4, 1–13
31 Park, J. J., & Bowman, N. A. (2015). Religion as bridging or bonding social capital: Race, religion, and cross-racial interaction for college students. Sociology of Education, 88(1), 20–37.
https://doi.org/10.1177/0038040714560172
32 Kuo, B. C. H. (2013). Collectivism and coping: Current theories, evidence, and measurements of collective coping. Int J Psychol, 48(3), 374–388
https://doi.org/10.1080/00207594.2011.640681
33 Esmaeeli, A., Pechmann, C. C., & Prochaska, J. J. (2022, May). Buddies as in-group influencers in online support groups: A social network analysis of processes and outcomes. J Interact Market, 57(2), 198–211.
https://doi.org/10.1177/10949968221076144
34 Gupta, S., Eggers, P., Arana, A., Kresse, B., Rios, K., Brown, L., Kploanyi, M. (2018, March). Knowledge and preventive behaviors towards tick-borne diseases in Delaware. Ticks and Tick-Borne Diseases, 9(3), 615–622.
https://doi.org/10.1016/j.ttbdis.2018.01.006
35 Siegel, S. D., Brooks, M. M., Sims-Mourtada, J., Schug, Z. T., Leonard, D. J., Petrelli, N., & Curriero, F. C. (2022, January). A population health assessment in a community cancer center catchment area: Triple-negative breast cancer, alcohol use, and obesity in New Castle County, Delaware. Cancer Epidemiol Biomarkers Prev, 31(1), 108–116
https://doi.org/10.1158/1055-9965.EPI-21-1031
36. Brooks, M. M., Siegel, S. D., & Curriero, F. C. (2021, March). Characterizing the spatial relationship between smoking status and tobacco retail exposure: Implications for policy development and evaluation. Health & Place, 68, 102530
https://doi.org/10.1016/j.healthplace.2021.102530
37 Offutt-Powell, T. N., Parykaza, M., Knapp, M., CodesJohnson, C., Kozak, I., & Muspratt, M. (2021). Delaware’s My Healthy Community data platform: At the intersection of public health informatics and epidemiology. Delaware Journal of Public Health, 15;7(3), 58-65.
128 Delaware Journal of Public Health - June 2023

FREE YOURSELF FROM TOBACCO You try to quit, but there are triggers everywhere you turn. You feel lost. Trapped. But you’re not alone. The Delaware Quitline has helped thousands escape their addiction and get on the path to living tobacco-free. Call 1-866-409-1858 or visit QuitSupport.com for free counseling, cessation aids, and medications to help you quit for good. 129
Ensuring Access to Opioid Treatment Program Services Among Delawareans Vulnerable to Flooding
Jennifer A. Horney, Ph.D., M.P.H. Professor, Epidemiology Program, University of Delaware
Sarah Elizabeth Scales, M.P.H. Graduate Research Assistant, Epidemiology Program, University of Delaware
Urkarsh Gangwal Graduate Research Assistant, Department of Civil and Environmental Engineering, University of Delaware
Shangjia Dong, Ph.D. Assistant Professor, Department of Civil and Environmental Engineering, University of Delaware
ABSTRACT
Objective: To quantify potential flood-related access disruptions to medication-assisted treatment for opioid use disorder (OUD) among Delawareans. Methods: Spatial flood risk maps and infrastructure, services, and hazard risk, transportation networks, opioid treatment programs (OTPs) for the State of Delaware were integrated to visually display the relationship between these layers. A complex network theory-based simulation model was used to assess both direct (e.g., inundation with flood water) and indirect (e.g., isolation) impacts of floods.
Results: Delaware is at increasing risk from flooding associated with storms and sea-level rise, which can lead to sunny day flooding during high tides. Of the 18 OTPs in Delaware, 4 are expected to be flooded in a 100year flood and 7 are expected to be severely disrupted, increasing to 9 by 2035 and to 10 by 2050, with service reachability less than 15 square miles due to flood-induced isolation. Conclusions: Individuals utilizing OTPs for OUDs must be able to access treatment programs regardless of external disruptors like floods. Because these programs require consistent treatment adherence and in-person oversight by clinicians, timely restoration of services and continuity of operations for treatment facilities in post-disaster settings is critical for treatment compliance. Policy Implications: The State of Delaware has the third highest rate of drug overdose mortality in the U.S., with three-quarters of all drug-related deaths involving opioids. Impeded access to opioid treatment during a flood disaster can lead to relapse, overdose, and death. Hazard planning must develop policies and practices to address these risks.
INTRODUCTION
In disaster and post-disaster contexts, most deaths are attributable to indirect causes, such as lapses in access to care and the deterioration of vital infrastructure.1,2 As disasters related to climate-mediated hazards become more common,3 it is important to better characterize and understand the wider societal-level impacts of disasters. One area of impact that needs more substantive exploration is the impact of disasters on the provision of opioid treatment program (OTP) services.
At 47.3 overdose deaths per 100,000 people, Delaware has the third highest drug overdose mortality rate of all U.S. States, with 75% of those overdose deaths involving opioids.4 In 2020, there were nearly 450 drug overdose deaths in Delaware.5 Ensuring that individuals with opioid use disorder (OUD) in disaster contexts have access to treatment is an important dimension of both facility- and community-level disaster preparedness and response. Prior disasters and emergencies have led to documented disruptions to access to OTPs. Following Hurricane Sandy, individuals with substance use disorders ran out of “take home” doses of medications for treating opioid use disorders.6 Following Hurricane Katrina, individuals in OTPs were at higher risk of withdrawal and relapse due to disruptions in treatment attributable to not only storm damage and displacement but also
cumbersome state and federal regulations without functional emergency provisions.7 Another study after Hurricane Katrina noted the downstream effects of treatment disruptions for individuals with comorbid psychiatric conditions8; these included but were not limited to homelessness, criminality, and overdose. In a study assessing disruptions to OTPs, Elliott et al., set forth recommendations from state opioid treatment authorities to mitigate the negative impacts of disasters on treatment continuity.9 However, most provisions centered on providing at-home doses, improving patient-provider communication, and implementing other stop-gap measures rather than addressing larger policy and planning frameworks to reduce overall risk.
METHODS
The location of OTPs in Delaware was downloaded from the U.S. Department of Health & Human Services and the Centers for Medicare & Medicaid Services. The road network was extracted from the open-source platform OpenStreetMap, and flood risk data was obtained from the First Street Foundation. These flood data are produced through a probabilistic flood model that considers flooding risk due to rainfall (pluvial), riverine flooding (fluvial), and coastal surge flooding. A complex network approach was employed to integrate flood risk with the transportation network, which was then
130 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.024
abstracted as a graph with nodes representing intersections and links representing roads.10 During network disruption simulation, once a road is detected in a flood zone, it was removed from the network. A search algorithm was then deployed to identify the flooded and isolated intersections from OTPs. The properties and population associated with those intersections were then estimated.
RESULTS
Delaware has a total of 18 OTPs (Figure 1). Mapping the State’s transportation network onto the OTP facility locations produces a total of 137,586 nodes and 170,114 edges, where nodes are intersections and links are roads (1a). When the 100-year floodplain map is overlaid with the transportation network, flooded roads can be identified. During flooding, 18,160 nodes in Delaware will be directly inundated. An additional 72,196 nodes, while not inundated, will lose access to OTPs (1b).

(a) 100-year flood map overlaid with road network of Delaware and spatial distribution of the OTPs. (b) Flooded and isolated (disconnected) nodes for access to OTPs. (c) the population impacted due to flooding and isolation. (d) OTPs that are either flooded or severely disrupted with reachability less than 15 sq. miles. (e) Estimated number of population and OTPs impacted by flooding.
The loss of access to OTPs is expected to grow over time (1c). Accounting for climate change impacts, the population impacted by flooding will increase when using projected flood risk for 2035 and 2050. In particular, isolated access to OTPs increases by more than three times the increase in the number of flooded OTPs (1c). Accordingly, the proportion of the population that may be isolated from needed OTP services during a flood disaster will only increase over time.
The operation of OTPs can be severely impacted as well (1d). Four OTPs will be flooded and 7 OTPs have a reachability (i.e., service coverage) less than 15 sq. miles in Year 2020 scenario. The reachability disruption risk continues to grow to 9 facilities in 2035 and 10 facilities in 2050 if no proper flood mitigation is implemented.
The risk of access loss is not equally distributed across Delaware. Communities like Middletown in New Castle County have a large population at risk of losing access to OTPs. However, the median household income of Middletown residents is nearly 30% higher than the state median income.11 Other communities which will be severely affected by flooding - Bridgeville and Millsboro in Sussex County - have median household incomes over 20% lower than the state median income. Higher socioeconomic status and other social determinants of health may allow affected populations to utilize additional resources - financial and otherwise - to mitigate negative impacts of flood disasters. Future research should consider the synergies between factors like income that contribute to social vulnerability and access to OTP and other types of acute care during a flooding disaster.
DISCUSSION
The importance of maintaining operational capacity for OTP in post-disaster contexts is multidimensional. First, individuals in treatment programs need to closely adhere to their treatment regimens to reduce the risk of relapse. Because medication-assisted treatment programs require access to methadone (or equivalent medications) and, in most scenarios, oversight by clinical staff, the physical security and operability of OTP facilities is vital to the provision of care.12 As flood risks increase over time, it is critically important to ensure that Delawareans who utilize
131
Figure 1. Flood disrupted road access to OTPs in Delaware
OTPs are able to quickly access services in flood disaster contexts to maintain treatment progress. Second, individuals who use opioids experience lapses in availability of opioids pre-and post-disaster. This, in conjunction with disturbances to treatment protocols, results in an increase in the number of emergency services consults for drug withdrawals. Quick resumption of OTP services can not only mitigate the negative health impacts on Delawareans but also relieve pressure on Delaware health systems as a whole. Further, because of the specialized nature of and federal regulations for OTP facilities, it is nearly impossible for these facilities to reopen in new locations in a timely manner.6 This is particularly problematic because the care provided by these programs is highly time-sensitive. Program, local, and state officials should account for these federal regulations in emergency planning and continuity of operations planning. Moreover, strengthening resilient and equitable postflooding access to acute care services should not be the health sector’s responsibility alone. Transportation infrastructure development and hazard mitigation decision-making should also consider the project’s impact on the community’s accessibility to OTP, especially those disadvantaged ones who repeatedly suffer from accessibility loss while having limited capacity to cope with and recover from the flooding.
PUBLIC HEALTH IMPLICATIONS
Flooding and other types of disasters can disrupt access to many types of infrastructure and services, including access to acute medical care such as OTPs. The negative health impacts of these disruptions can be particularly severe for people with OUDs. In the case of a 100-year flood in Delaware, more than 600,000 Delaware residents would potentially be unable to access an OTP because of a flooded road or the isolation of an OTP facility by floodwater. Missing treatment has been consistently associated with mental distress and psychological consequences, as well as relapse, overdose, and death. Therefore, planning and policy interventions that address increasing flood hazards and associated risks to OTPs in Delaware are needed to prevent disaster-associated program closures.
Dr. Horney may be contacted at horney@udel.edu
REFERENCES
1. Arnold, C. (2019, February). Death, statistics and a disaster zone: The struggle to count the dead after Hurricane Maria. Nature, 566(7742), 22–25.
https://doi.org/10.1038/d41586-019-00442-0
2. Green, H. K., Lysaght, O., Saulnier, D. D., Blanchard, K., Humphrey, A., Fakhruddin, B., & Murray, V. (2019). Challenges with disaster mortality data and measuring progress towards the implementation of the Sendai Framework. International Journal of Disaster Risk Science, 10(4), 449.
https://doi.org/10.1007/s13753-019-00237-x
3 IPCC WGII. (2021). Climate change 2022 impacts, adaptation and vulnerability summary for policymakers [Sixth Assessment Report of the Intergovernmental Panel on Climate Change]. Intergovernmental Panel on Climate Change.
https://www.ipcc.ch/report/ar6/wg1/downloads/report/IPCC_AR6_ WGI_SPM.pdf
4. National Center for Health Statistics. (2020). Drug overdose mortality by state.
https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_ mortality/drug_poisoning.htm
5. Centers for Disease Control and Prevention. (2022, Mar 1). Drug overdose mortality by state.
https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_ mortality/drug_poisoning.htm
6 Griffin, A. R., Der-Martirosian, C., Gable, A., WyteLake, T., & Dobalian, A. (2018). A crisis within a crisis: The extended closure of an opioid treatment program after hurricane sandy. Journal of Drug Issues, 48(4), 536–545
https://doi.org/10.1177/0022042618779541
7. Rutkow, L., Vernick, J. S., Mojtabai, R., Rodman, S. O., & Kaufmann, C. N. (2012, January). Legal challenges for substance abuse treatment during disasters. Psychiatric Services (Washington, D.C.), 63(1), 1–9.
https://doi.org/10.1176/appi.ps.2012000p7
8. Shuler-Baker, M., Suzuki, S., Podesta, A., QuallsHampton, R., & Wallington, S. (2017). A post-hurricane Katrina examination of substance abuse treatment discharges with co-occurring psychiatric and substance use disorders. Journal of Dual Diagnosis, 13, 00–00. https://doi.org/10.1080/15504263.2016.1277816
9 Elliott, L., Benoit, E., Matusow, H., & Rosenblum, A. (2017). Disaster preparedness among opioid treatment programs: Policy recommendations from state opioid treatment authorities. International Journal of Disaster Risk Reduction, 23, 152–159
https://doi.org/10.1016/j.ijdrr.2017.05.001
10. Gangwal, U., Siders, A. R., Horney, J., Michael, H. A., & Dong, S. (2023). Critical facility accessibility and road criticality assessment considering flood-induced partial failure. Sustainable and Resilient Infrastructure, 8(sup1), 337-355.
https://doi.org/10.1080/23789689.2022.2149184
11 US Census Bureau. (2022, Dec 6). Delaware; Millsboro town, Delaware; Middletown town, Delaware. US Census Bureau QuickFacts. Retrieved February 16, 2023, from https://www.census.gov/quickfacts/fact/table/ DE,millsborotowndelaware,middletowntowndelaware/PST045222
12 Substance Abuse and Mental Health Services Administration. (2022, Jul 7). Medication-assisted treatment (MAT). SAMHSA.
https://www.samhsa.gov/medication-assisted-treatment
132 Delaware Journal of Public Health - June 2023
Open your door to a healthier future, with the Home Visiting program.
The Home Visiting Program is free and voluntary, and can take place at your home or a location of your choice. The program is proven to improve the health of babies and parents, as well as help in a baby’s development.
Who?
Family Support Specialists are trained nurses, social workers, and parent educators.
What?
Family Support Specialists will get to know you so that they can offer support services to meet your situation. They can offer ways to help you make your home safer through things like promoting safe-sleep practices, helping you understand your child’s development, and more.
Why?
The results of the program are proven, and the benefits for families have been clear. Families who have chosen to participate in the free Home Visiting Program have experienced:
• Improved maternal and child health
• Earlier detection of possible developmental delays or disabilities

• Improvement in school readiness and achievement
• Regular health care provider visits, reduction in stress levels, and smoking cessation
• Completion of educational and/or training programs as well as more financial independence

When?
Now. To learn more or sign up for the program, call 2-1-1, text your ZIP code to 898-211, or visit DEThrives.com/Home-Visiting.
We support families where help is needed, one step at a time.
Family Support Specialists are not intended to replace office-based OB-GYN, family, or pediatric care, but rather to supplement and reinforce it. Welcome a chance for a brighter, healthier tomorrow. 133
Postpartum Contraceptive Use, Pregnancy Intentions in Women With and Without a Delivery of a NAS-Affected Infant in Delaware, 2012-2018
Khaleel Hussaini, Ph.D.
Division of Public Health, Delaware Department of Health and Social Services; Division of Reproductive Health, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services
George Yocher, M.S. Division of Public Health, Delaware Department of Health and Social Services
ABSTRACT
Objective: Assess differences in postpartum contraceptive use and pregnancy intentions in women with a recent live birth who delivered a neonatal abstinence syndrome (NAS) affected infant. Study Design: Using linked Delaware Birth Certificate Data, Hospital Discharge Data and PRAMS data for 2012–2018 (n = 6,358 singleton births), we assessed differences among women with and without a delivery of an NAS-affected infant by effective postpartum contraceptive use and pregnancy intentions. We calculated prevalence estimates, crude (cPOR), and prevalence odds ratios adjusted (aPOR) for NAS by maternal characteristics. We used alpha ≤ 0.05 to determine statistical significance. Results: Prevalence of NAS was 2.2% (95% CI: 1.8 – 2.6). Effective postpartum contraceptive use was 60.4% (95% CI: 51.9-69.0) among women with delivery of an NAS-affected infant compared with a nonNAS delivery 56.4% (95% CI: 55.1-57.8%) and cPOR was 1.2 (95% CI: 0.8-1.7). Prevalence of intended pregnancy was 26.5% (95% CI: 18.9-34.0) among women with delivery of an NAS-affected infant compared with a non-NAS delivery 53.0% (95% CI: 51.7-54.4) and cPOR was 0.3 (95% CI: 0.2-0.5). After adjustment, women who delivered an NAS-affected infant had lower odds (aPOR = 0.5; 95% CI: 0.3-0.8) of indicating that their pregnancy was intended as compared to those who did not deliver an NAS-affected infant. Conclusions: Our study found no association between delivery of an NAS-affected infant and use of an effective postpartum contraceptive method. However, we found that pregnancy intendedness was lower among women delivering an NAS-affected infant compared with women without an NAS delivery even after accounting for maternal characteristics.
INTRODUCTION
Neonatal abstinence syndrome (NAS) is a withdrawal syndrome and a complex multisystem disorder that varies in signs, symptoms, and severity among infants. NAS occurs shortly after birth in infants born to women with chronic opioid use (heroin, prescription pain medicines), or with maternal medications for opioid use disorder such as methadone or buprenorphine, as well as exposures to cocaine, selective serotonin reuptake inhibitors (SSRIs) and nicotine.1–10 The rates of NAS and maternal opioid use disorder have also shown to vary across states in the U.S. and Delaware’s NAS rate is among top five in the U.S.9
Reddy et al. discuss the importance of providing postpartum care support such as contraceptive counseling to women affected by opioid use disorder (OUD), because accessing reproductive life planning services may be particularly challenging for women with OUD due to stigma and discrimination.11
There are limited studies on contraceptive choices, use, and pregnancy intentions of women who deliver an NAS-affected infant. In a retrospective U.K. cohort study of 376 women aged 20-61 years in active treatment for opioid addiction, Cornford et al.,12 noted lower use of planned contraception. In another retrospective cohort study, Krans et al.13 used data for Medicaid enrolled women in Pennsylvania and found that women with OUD were less likely to use highly effective postpartum contraception. In an experimental study of 31 women in Vermont
at an opioid maintenance treatment program, Heil et al.14 found that all women in the experimental condition, initiated prescription contraceptive use. In another study of 946 pregnant women who misused opioids, Heil et al.15 found that 86% of the pregnancies were unintended.
Apart from Krans et al.’s study that was specific to Medicaid enrolled women, other studies have focused on participants in opioid use treatment, or a sub-population of opioid users limited by generalizability, and small sample size. Given the limited number of studies on contraceptive choice, use, and pregnancy intentions in this population, and high maternal OUD and NAS rates in Delaware, our primary aim was to assess differences in postpartum contraceptive use, and our secondary aim was to assess pregnancy intentions in women with a recent live birth who delivered an NAS-affected infant16–18 versus those who did not.
METHODS Data and Sample
We utilized linked Pregnancy Risk Assessment Monitoring System (PRAMS) data, Hospital Discharge data (HDD) and Birth Certificates data (BCD) for 2012-2018 for Delaware. PRAMS is administered by the Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health and operates through cooperative agreements between CDC and the states. It is a dual-mode survey that uses U.S.
134 Delaware Journal of Public Health - June 2023 Doi: 10.32481/djph.2023.06.025
mail as the primary method for data collection with telephone follow-up for respondents and comprises a stratified random sample of women from the birth certificate records who had a recent live birth19,20 and complete the questionnaire between two to six months postpartum. Delaware PRAMS was established in 2006 and has continually collected data on a variety of topics of women’s experiences before, during, and after pregnancy. The HDD for inpatient admissions from all Delaware licensed hospitals are collected under Delaware law (16 Del.C. Ch. 20, § 2001-2009) and include all non-federal facilities. Records are collected quarterly based on the uniform claims and billing dataset (UB-82 or successor form) for all hospital inpatient discharges.
Unique identifiers (e.g., hospital identifiers, medical record numbers, first name, last name, date of birth, etc.) were used to identify all hospital births to Delaware residents between 2012 and 2018. We used these identifiers to first link HDD data containing information on all newborns (e.g., diagnoses including NAS, procedures, discharge summary, length of stay, etc.) with hospital births in BCD that contain information on demographics, insurance status, information on prenatal care. The HDD-BCD linkage yielded about a 99 percent match using a deterministic linkage method. Since PRAMS respondents are a subset of BCD (i.e., sampled from birth certificate data), we re-linked PRAMS data that contains information on postpartum contraceptive use, health and health-related behaviors before, during, and after pregnancy, pregnancy intentions, healthcare quality, etcetera to the linked HDD-BCD dataset for 2012-2018. Our analytic sample comprised of 6,358 singleton deliveries during 2012-2018 with linked HDD-BCD-PRAMS data. PRAMS data contain weights to account for the survey and sampling design and produce estimates generalizable to the population of women who deliver a live birth. Because we use multiple years of survey data, we recreated a weight for combined years of PRAMS based on Korn et al.21 methodology. As we used secondary analysis of data that involved no human participants, our study was reviewed by the Delaware Division of Public Health review board and exempt under applicable federal law and the activity was determined to meet the requirements of public health surveillance as defined in 45 CFR 46.102(l)(2). The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Measures
Use of postpartum contraception was ascertained from PRAMS. The PRAMS question asks women, “Are you or your husband or partner doing anything now to keep from getting pregnant?” with response choices: (yes/no). Respondents who indicate “no” to this core question are classified as using no method. Respondents who answer “yes” are further asked, “What kind of birth control are you or your husband or partner using now to keep from getting pregnant?” with response choices: 1) tubes tied or blocked (female sterilization, Essure®, Adiana®); 2) vasectomy (male sterilization); 3) birth control pill; 4) condoms; 5) injection (Depo-Provera®); 6) contraceptive implant (Implanon®); 7) contraceptive patch (OrthoEvra®) or vaginal ring (NuvaRing®); 8) intrauterine devices (IUD including Mirena® or ParaGard®); 9) natural family planning (including rhythm method); 10) withdrawal (pulling out); 11) not having sex/abstinence; and 12) other methods. Respondents who answer “yes” and indicate specific contraceptive methods were categorized into: a) most effective
(items 1, 2, 6, and 8); b) moderately effective methods (items 3, 5, and 7); and least effective methods (items 4, 9, 10, 12) based on CDC and previous studies.20,22,23 Respondents who answered “yes” but indicated not having sex/abstinence (item 11) were also classified as no method because, while abstinence may theoretically be 100% effective if used perfectly, the effectiveness of abstinence may approach zero, in typical use.24 We dichotomized this further into effective (i.e., most, and moderately effective) and other methods (i.e., least or no method).
We also ascertained pregnancy intentions from PRAMS which asks women, “Thinking back to just before you got pregnant with your new baby, how did you feel about becoming pregnant?” Response choices are: 1) I wanted to be pregnant later; 2) I wanted to be pregnant sooner; 3) I wanted to be pregnant then; 4) I didn’t want to be pregnant then or at any time in the future; 5) I wasn’t sure what I wanted. The pregnancy intention measure described here is consistent with use of PRAMS data in other studies20,21,25,26 as “wanted then or sooner” (i.e., items 2 and 3); “unsure” (i.e., item 5); and “wanted later or unwanted” (i.e., items 1 and 4). For purposes of simplicity, we further dichotomized this as “intended” and “other.”
For our primary exposure, we ascertained delivery of an infant with NAS from the HDD using International Classification of Diseases – Ninth Revision Clinical Modification (ICD-9CM) diagnosis of 779.5 and ICD-10-CM diagnosis of P96.1 excluding iatrogenic cases of NAS, very low birth weight, intraventricular hemorrhage, periventricular leukomalacia, necrotizing enterocolitis, spontaneous intestinal perforation, or bronchopulmonary dysplasia similar to Patrick et al.,6,8 and similar to the current tier 2 definitions from the Council of State and Territorial Epidemiologists.27
Covariates
We include maternal characteristics from BCD that were shown in previous studies22,23,25,26 to be associated with contraceptive use and pregnancy intentions: maternal age (<25 and 25 years or more), maternal education (<12 years of school; high school graduate; more than 12 years of school), race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic other races i.e., includes Asian, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, and two or more races), marital status (married vs. other), parity (0, 1, 2, or 3 or more) and insurance status (i.e., Medicaid vs. non-Medicaid).
Statistical Analysis
We estimated the overall prevalence estimates with 95% confidence intervals (CIs) for each outcome stratified by delivery of an NAS-affected infant and each maternal characteristic. We calculated the crude prevalence odds ratio (cPOR) for the association between each of the maternal characteristic. Finally, we calculated the adjusted prevalence odds ratio (aPOR) for the association between delivery of a NAS-affected infant and each outcome, adjusted for all maternal characteristics. As we had less than 2.0% missing data, we used listwise deletion. All tests were two-sided with alpha at 0.05 level of significance. All analyses were weighted and carried out using SAS v9.4 (SAS Institute, Inc., Cary, NC) with complex survey module.
135
RESULTS
For the 6,358 deliveries in Delaware during 2012-2018, Table 1 shows the prevalence of delivery of an NAS-affected infant, postpartum contraceptive methods and pregnancy intentions. NAS was identified in 169 infants (Table 1) for an estimated prevalence of 2.2% (95% CI:1.8-2.6) of deliveries, consistent with statewide population estimates.29 Prevalence of most effective postpartum contraceptive methods in Delaware women with a recent live birth was 26.3% (95% CI: 25.1-27.5); moderately effective methods was 30.2% (95% CI: 29.0-31.5); least effective methods was 23.2% (95% CI: 22.0-24.3); and no method was 20.6% (95% CI: 19.3-21.4). Overall, 56.5% (95% CI: 55.2-57.8) of Delaware women with a recent live birth indicated effective use of contraceptive methods. Regarding pregnancy intentions, 52.4% (95% CI: 51.1-53.8) indicated that their pregnancy was intended (i.e., wanted then or sooner), 16.1% (95% CI: 15.1-17.1) were “not sure”, and 31.5% (95% CI: 30.2-32.7) indicated that their pregnancy was unintended (i.e., wanted later or unwanted).
All maternal characteristics were associated with effective postpartum contraceptive method and pregnancy intentions (Table 2). Although, the prevalence of postpartum effective contraceptive method was slightly higher in women who delivered an NAS-affected infant as compared with a non-NAS delivery (60.4%; 95% CI: 51.9-69.0 vs. 56.4%; 95% CI: 55.1-57.8), the difference was not statistically significant and the estimated cPOR was 1.2 (95% CI: 0.8-1.7) and after adjusting for maternal characteristics the aPOR (Table 3) was 0.8 (95% CI: 0.6-1.2).
In contrast, the prevalence of intended pregnancy was lower in women who delivered an NAS-affected infant as compared with a non-NAS delivery (26.5%; 95% CI: 18.9-34.0 vs. 53.0%; 95% CI: 51.7-54.4). The difference was statistically significant and the estimated cPOR was 0.3 (95% CI: 0.2-0.5). After adjusting for maternal characteristics, women who delivered an NAS-affected infant had 50 percent lower odds (aPOR = 0.5; 95% CI: 0.3-0.8) of indicating that their pregnancy was intended as compared with women without an NAS-affected delivery (Table 3).
Notes: N is unweighted count of pregnant women with weighted percent and 95% confidence intervals (CI). NAS = neonatal abstinence syndrome; International Classification of Diseases – Ninth Revision Clinical Modification (ICD-9-CM) diagnosis of 779.5 and ICD-10-CM diagnosis of P96.1
136 Delaware Journal of Public Health - June 2023
Table 1. Prevalence Estimates with 95% Confidence Intervals for Delivering an Infant with Neonatal Abstinence Syndrome, Contraceptive Methods, and Pregnancy Intentions in Delaware Women with a Live Birth, 2012-201828
Exposure/Outcome N Prevalence (95% CI) NAS Delivery Yes 169 2.2 (1.8-2.6) No 6,189 97.8 (97.4-98.2) Postpartum Contraceptive Methods Most effective 1,620 26.3 (25.1-27.5) Moderately effective 1,889 30.2 (29.0-31.5) Least effective 1,465 23.2 (22.0-24.3) No method 1,273 20.6 (19.3-21.4) Unknown/missing 111 N/A Effective Postpartum Contraceptive Method Effective 3,509 56.5 (55.2-57.8) Other 2,738 43.5 (42.2-44.8) Unknown/missing 111 N/A Pregnancy Intentions Intended (wanted then or sooner) 3,286 52.4 (51.1-53.8) Not sure 1,029 16.1 (15.1-17.1) Unintended (wanted later or unwanted) 1,961 31.5 (30.2-32.7) Unknown/missing 82 N/A Intended Pregnancy Intended 3,286 52.4 (51.1-53.8) Other (i.e., unsure/unintended) 2,990 47.6 (46.2-48.9) Unknown/missing 82 N/A
Table 2. Prevalence Estimates and Crude Prevalence Odds Ratios of Postpartum Contraceptive Methods and Pregnancy Intendedness by Maternal Characteristics in Delaware, 2012-201828
137
Maternal Characteristics Postpartum Contraceptive Methods Pregnancy Intended Effective % (95% CI) Other % (95% CI) cPOR (95% CI) Intended % (95% CI) Other % (95% CI) cPOR (95% CI) NAS Delivery Yes 60.4 (51.9-69.0) 39.6 (31.0-48.1) 1.2 (0.8-1.7) 26.5 (18.9-34.0) 73.5 (66.0-81.1) 0.3 (0.2-0.5)*** No 56.4 (55.1-57.8) 43.6 (42.2-44.9) Ref 53.0 (51.7-54.4) 47.0 (45.6-48.3) Ref Age (in years) Less than 25 61.7 (59.1-64.4) 38.3 (35.6-40.9) 1.3 (1.2-1.5)*** 31.3 (28.7-33.8) 68.7 (66.2-71.3) 0.3 (0.3-0.3)*** 25 and older 54.7 (53.2-56.2) 45.3 (43.8-46.8) Ref 59.8 (58.3-61.3) 40.2 (38.7-41.7) Ref Education < 12 years of schooling 57.8 (54.5-61.2) 42.2 (38.8-45.5) 1.2 (1.0-1.4)* 40.9 (37.6-44.2) 59.1 (55.8-62.4) 0.4 (0.3-0.4)*** High school graduate 61.8 (59.2-64.4) 38.2 (35.6-40.8) 1.4 (1.2-1.6)*** 37.9 (35.3-40.5) 62.1 (59.5-64.7) 0.4 (0.4-0.5)*** > 12 years of schooling 53.8 (52.0-55.5) 46.2 (44.5-48.0) Ref 62.3 (60.6-64.0) 37.7 (36.0-39.4) Ref Marital Status Married 49.5 (47.7-51.3) 50.5 (48.7-52.3) 0.5 (0.5-0.6)*** 70.1 (68.5-71.8) 29.9 (28.2-31.5) 4.8 (4.3-5.4)*** Other 64.3 (62.4-66.2) 35.7 (33.8-37.6) Ref 32.9 (31.0-34.8) 67.1 (65.2-69.0) Ref Parity 0 53.7 (51.5-55.8) 46.3 (44.2-48.5) 0.6 (0.5-0.8)*** 54.6 (52.5-56.8) 45.4 (43.2-47.5) 2.4 (2.0-2.9)*** 1 57.5 (55.1-59.9) 42.5 (40.1-44.9) 0.7 (0.6-0.9)*** 60.4 (58-62.7) 39.6 (37.3-42) 3.1 (2.5-3.7)*** 2 59.6 (56.3-62.9) 40.4 (37.1-43.7) 0.8 (0.6-1.0)*** 45.5 (42.1-48.9) 54.5 (51.1-57.9) 1.7 (1.3-2.1)*** 3 or more 64.8 (61.0-68.6) 35.2 (31.4-39.0) Ref 33.3 (29.6-37) 66.7 (63-70.4) Ref Race and Ethnicity White (non-Hispanic) 55.3 (53.5-57.1) 44.7 (42.9-46.5) 2.3 (1.9-2.9)*** 60.4 (58.7-62.2) 39.6 (37.8-41.3) 1.1 (0.9-1.4) Black (non-Hispanic) 63.3 (60.6-66.0) 36.7 (34.0-39.4) 3.2 (2.6-4.1)*** 34.5 (31.9-37.2) 65.5 (62.8-68.1) 0.4 (0.3-0.5)*** Hispanic 60.3 (56.9-63.7) 39.7 (36.3-43.1) 2.9 (2.2-3.7)*** 51.4 (47.9-54.8) 48.6 (45.2-52.1) 0.8 (0.6-1.0)* Other races 34.7 (30.1-39.4) 65.3 (60.6-69.9) Ref 58.0 (53.2-62.8) 42.0 (37.2-46.8) Ref Medicaid Yes 63.8 (61.9-65.7) 36.2 (34.3-38.1) 1.7 (1.6-2.0)*** 35.4 (33.5-37.3) 64.6 (62.7-66.5) 0.3 (0.2-0.3)*** No 50.2 (48.4-52.0) 49.8 (48.0-51.6) Ref 68.0 (66.3-69.7) 32.0 (30.3-33.7) Ref ****p < .0001 **p < .01 *p < .05 Notes: Weighted percent and crude prevalence odds ratio (cPOR) with 95% confidence intervals (CI). NAS = neonatal abstinence syndrome; International Classification of Diseases – Ninth Revision Clinical Modification (ICD-9-CM) diagnosis of 779.5 and ICD-10-CM diagnosis of P96.1
Notes: Adjusted prevalence odds ratios (aPOR) with 95% confidence intervals (CI). Models adjusted for maternal age, education, marital status, parity, race and ethnicity, and Medicaid status.
NAS = neonatal abstinence syndrome; International Classification of Diseases – Ninth Revision Clinical Modification (ICD-9-CM) diagnosis of 779.5 and ICD-10-CM diagnosis of P96.1
DISCUSSION
Using statewide linked PRAMS, birth certificate, and hospital discharge data, our study aimed to assess differences between women who delivered an NAS-affected infant (i.e., a proxy for opioid use) versus those who did not for postpartum contraceptive use and pregnancy intentions in Delaware. Our study found no association between delivery of an NAS-affected infant and use of an effective postpartum contraceptive method. Cornford et al., found lower use of planned contraception in a U.K. cohort of women with OUD.12 Similarly, Krans et al., study of Pennsylvania’s Medicaid enrolled women found that women with OUD were less likely to use highly effective postpartum contraception.13 Heil et al. found that in the experimental group, all women in the OUD treatment program who received free prescription contraceptives, and “financial incentives” initiated prescription contraceptive use following delivery, when compared to the control group who received usual care (i.e., free condoms, received emergency contraception, referral to providers) although such strategies may be coercive.14,30,31
During our 2012-2018 study period, Delaware saw a significant increase in use of long-acting reversible contraceptives in Title X and Medicaid populations.32,33 A statewide data brief indicated that there was 107% increase in reversible contraceptive methods during 2012-2018, and a 17% percent increase in the percent of Delaware women indicating their pregnancy was intended.34 Although our study did not find statistically significant differences in effective postpartum contraceptive use among women with an NAS-affected and non-NAS delivery, the low prevalence of effective postpartum contraceptive methods for both groups suggest that sustained and continued statewide efforts that are non-coercive and culturally appropriate may be needed to increase access to effective methods of contraceptives. With regard to pregnancy intention, our study found that Delaware women with delivery of an NAS-affected infant had lower odds of indicating that their pregnancy was “intended” as compared to women without an NAS-affected delivery even after we account for maternal characteristics. Our study findings are consistent with Heil et al.’s study who also found that unintended pregnancy was highly prevalent (nine of every 10 women screened) and intended pregnancies were low among women with OUD.15 Unintended pregnancy is associated with increased risk
for postpartum depression and lower levels of perceived support,35 and OUD treatment is lower among women who reported unintended pregnancies.36 Women with OUD who already contend with several life stressors, may benefit from treatment for opioid use disorder, increased access to preconception and interconception resources including reproductive health planning.
Limitations
Despite the strength of linked administrative data and PRAMS survey data, the cross-sectional nature of our study limits our ability to draw causal inferences. PRAMS data are based on selfreport and may be subject to recall bias, although this may have been minimized for contraceptive use in our analysis because we focused on contraceptive use at the time the PRAMS survey was completed in the postpartum period (typically 2-6 months after delivery). Our contraceptive estimates did not account for women who were trying to get pregnant and were not sexually active. Identification of NAS was based on administrative data such as HDD and may be prone to coding errors.6 In addition, not all neonates chronically exposed to opioids develop NAS postdelivery.5 Even though PRAMS is a probability-based representative sample from birth certificates generalizable to all Delaware women with a recent live birth, low numbers of total NAS cases during 2012-2018 (n = 169), limited our ability to conduct sub-group analyses to examine effect modification. Linked datasets such as ours from other states may provide a sufficient sample size to allow discernment of how a delivery of an NAS-affected infant (i.e., proxy for opioid use disorder) may be associated with contraceptive use and choices, and pregnancy intentions. Lastly, our dataset was limited as we did not have information on NAS due to appropriate use of prescription opioids, misuse of opioids, or maternal opioid use disorder.
CONCLUSION
Using representative statewide data, we assessed whether an NAS delivery was associated with effective postpartum contraceptive methods, and pregnancy intendedness. Although we did not find an association among women who delivered an NAS-affected infant and effective postpartum contraceptive method, our data suggests that intended pregnancies were lower in women who delivered an NAS-affected infant as compared with those without a delivery of an NAS-affected infant even after accounting for maternal characteristics. The importance of
138 Delaware Journal of Public Health - June 2023
Maternal Characteristics Adjusted Prevalence Odds Ratio Effective Postpartum Contraceptive Method (95% CI) Pregnancy Intended (95% CI) NAS delivery Yes 0.8 (0.6-1.2) 0.5 (0.3-0.8)** No Ref Ref ****p < .0001 **p < .01 *p < .05
Table 3. Adjusted Prevalence Odds Ratios of NAS Delivery, Postpartum Contraceptive Methods, and Pregnancy Intendedness in Delaware, 2012-201828
reproductive counseling to women affected by opioid use disorder has been well-established. However, there is limited research on postpartum contraceptive use and pregnancy intentions in women with and without a NAS delivery. Our findings suggest an opportunity to improve outreach efforts in this population during preconception and interconception periods to develop a reproductive life-plan, counsel women on effective postpartum contraceptive use methods, and increase their access to effective contraceptive methods. Strategies to prevent the incidence of NAS deliveries through CDC’s opioid prescribing guidelines37 and access to preconception and family planning services, pregnancy intention screening, improving access to reproductive counseling and a full-range of contraceptive methods that include long-acting reversible contraception (e.g., intrauterine devices, and implants) may help reduce this disparity in unintended pregnancy. Dr. Hussaini may be contacted at Khaleel.hussaini@delaware.gov
REFERENCES
1. Jansson, L. M., & Patrick, S. W. (2019, April). Neonatal abstinence syndrome. Pediatric Clinics of North America, 66(2), 353–367.
https://doi.org/10.1016/j.pcl.2018.12.006
2 Jansson, L. M., & Velez, M. L. (2019, August). Optimal care for NAS: Are we moving in the wrong Direction? Hospital Pediatrics, 9(8), 655–658
https://doi.org/10.1542/hpeds.2019-0119
3 Jansson, L. M., & Velez, M. (2012, April). Neonatal abstinence syndrome. Current Opinion in Pediatrics, 24(2), 252–258. https://doi.org/10.1097/MOP.0b013e32834fdc3a
4. Kocherlakota, P. (2014, August). Neonatal abstinence syndrome. Pediatrics, 134(2), e547–e561. https://doi.org/10.1542/peds.2013-3524
5. McQueen, K., & Murphy-Oikonen, J. (2016, December 22). Neonatal abstinence syndrome. The New England Journal of Medicine, 375(25), 2468–2479 https://doi.org/10.1056/NEJMra1600879
6. Patrick, S. W., Schumacher, R. E., Benneyworth, B. D., Krans, E. E., McAllister, J. M., & Davis, M. M. (2012, May 9). Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA, 307(18), 1934–1940 https://doi.org/10.1001/jama.2012.3951
7 Patrick, S. W., Burke, J. F., Biel, T. J., Auger, K. A., Goyal, N. K., & Cooper, W. O. (2015, October). Risk of hospital readmission among infants with neonatal abstinence syndrome. Hospital Pediatrics, 5(10), 513–519. https://doi.org/10.1542/hpeds.2015-0024
8. Patrick, S. W., Dudley, J., Martin, P. R., Harrell, F. E., Warren, M. D., Hartmann, K. E., Cooper, W. O. (2015, May). Prescription opioid epidemic and infant outcomes. Pediatrics, 135(5), 842–850
https://doi.org/10.1542/peds.2014-3299
9 Hirai, A. H., Ko, J. Y., Owens, P. L., Stocks, C., & Patrick, S. W. (2021, January 12). Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA, 325(2), 146–155.
https://doi.org/10.1001/jama.2020.24991
10 Winkelman, T. N. A , Villapiano, N., Kozhimannil, K. B., Davis, M. M., & Patrick, S. W. (2018, April). Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004-2014. Pediatrics, 141(4), e20173520
https://doi.org/10.1542/peds.2017-3520
11. Reddy, U. M., Davis, J. M., Ren, Z., & Greene, M. F., & the Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers (2017, July). Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes: Executive Summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Society for Maternal-Fetal Medicine, Centers for Disease Control and Prevention, and the March of Dimes Foundation. Obstetrics and Gynecology, 130(1), 10–28
https://doi.org/10.1097/AOG.0000000000002054
12. Cornford, C. S., Close, H. J., Bray, R., Beere, D., & Mason, J. M. (2015, March 4). Contraceptive use and pregnancy outcomes among opioid drug-using women: A retrospective cohort study. PLoS One, 10(3), e0116231.
https://doi.org/10.1371/journal.pone.0116231
13 Krans, E. E., Kim, J. Y., James, A. E., III, Kelley, D. K., & Jarlenski, M. (2018, April 1). Postpartum contraceptive use and interpregnancy interval among women with opioid use disorder. Drug and Alcohol Dependence, 185, 207–213
https://doi.org/10.1016/j.drugalcdep.2017.12.023
14. Heil, S. H., Hand, D. J., Sigmon, S. C., Badger, G. J., Meyer, M. C., & Higgins, S. T. (2016, November). Using behavioral economic theory to increase use of effective contraceptives among opioid-maintained women at risk of unintended pregnancy. Preventive Medicine, 92, 62–67.
https://doi.org/10.1016/j.ypmed.2016.06.023
15 Heil, S. H., Jones, H. E., Arria, A., Kaltenbach, K., Coyle, M., Fischer, G., . . . Martin, P. R. (2011, March). Unintended pregnancy in opioid-abusing women. Journal of Substance Abuse Treatment, 40(2), 199–202
https://doi.org/10.1016/j.jsat.2010.08.011
16. Faherty, L. J., Kranz, A. M., Russell-Fritch, J., Patrick, S. W., Cantor, J., & Stein, B. D. (2019, November 1). Association of punitive and reporting state policies related to substance use in pregnancy with rates of neonatal abstinence syndrome. JAMA Network Open, 2(11), e1914078
https://doi.org/10.1001/jamanetworkopen.2019.14078
17 Faherty, L. J., Matone, M., Passarella, M., & Lorch, S. (2018, June). Mental health of mothers of infants with neonatal abstinence syndrome and prenatal opioid exposure. Maternal and Child Health Journal, 22(6), 841–848
https://doi.org/10.1007/s10995-018-2457-6
18. Kozhimannil, K. B., Graves, A. J., Jarlenski, M., KennedyHendricks, A., Gollust, S., & Barry, C. L. (2017, May 1). Non-medical opioid use and sources of opioids among pregnant and non-pregnant reproductive-aged women. Drug and Alcohol Dependence, 174, 201–208
https://doi.org/10.1016/j.drugalcdep.2017.01.003
139
19 Centers for Disease Control and Prevention. (2021). PRAMS model surveillance protocol, 2015 version. http://www.cdc.gov/prams/methodology.htm
20. Shulman, H. B., D’Angelo, D. V., Harrison, L., Smith, R. A., & Warner, L. (2018, October). The Pregnancy Risk Assessment Monitoring System (PRAMS): Overview of Design and Methodology. American Journal of Public Health, 108(10), 1305–1313.
https://doi.org/10.2105/AJPH.2018.304563
21. Korn, E., & Graubard, B. (1999). Analysis of health surveys. New York: Wiley.
22. Kortsmit, K., Williams, L., Pazol, K., Smith, R. A., Whiteman, M., Barfield, W., Warner, L. (2019, July 1). Condom use with long-acting reversible contraception vs non-long-acting reversible contraception hormonal methods among postpartum adolescents. JAMA Pediatrics, 173(7), 663–670
https://doi.org/10.1001/jamapediatrics.2019.1136
23 Zapata, L. B., Murtaza, S., Whiteman, M. K., Jamieson, D. J., Robbins, C. L., Marchbanks, P. A., Curtis, K. M. (2015, February). Contraceptive counseling and postpartum contraceptive use. American Journal of Obstetrics and Gynecology, 212(2), 171.e1–171.e8
https://doi.org/10.1016/j.ajog.2014.07.059
24 Dailard, C. (2022). Understanding ‘abstinence’: Implications for individuals, programs and policies.
https://www.guttmacher.org/gpr/2003/12/understanding-abstinenceimplications-individuals-programs-and-policies
25 Kost, K., & Lindberg, L. (2015, February). Pregnancy intentions, maternal behaviors, and infant health: Investigating relationships with new measures and propensity score analysis. Demography, 52(1), 83–111. https://doi.org/10.1007/s13524-014-0359-9
26. Lindberg, L., Maddow-Zimet, I., Kost, K., & Lincoln, A. (2015, May). Pregnancy intentions and maternal and child health: An analysis of longitudinal data in Oklahoma. Maternal and Child Health Journal, 19(5), 1087–1096. https://doi.org/10.1007/s10995-014-1609-6
27. Council for State and Territorial Epidemiologists. (2019). Standardized surveillance for diseases or conditions, revised 2019. https://cdn.ymaws.com/www.cste.org/resource/resmgr/ ps/2019ps/19-MCH-01_NAS_updated_5.7.19.pdf
28. Delaware Department of Health and Social Services, Division of Public Health. (2018). Pregnancy Risk Assessment and Monitoring Survey, Delaware, 2012-2018
29 Hussaini, K. S., Drummond, D.E., Bartoshesky, L., Acheson, A., Stomieroski, K.A., Paul, D., & Kirby, R. S. (2021, January 15). Assessing the relationship between neonatal abstinence syndrome and birth defects in Delaware. Birth Defects Research, 113(2), 144–151
https://doi.org/10.1002/bdr2.1811
30. Brandi, K., Woodhams, E., White, K. O., & Mehta, P. K. (2018, April). An exploration of perceived contraceptive coercion at the time of abortion. Contraception, 97(4), 329–334
https://doi.org/10.1016/j.contraception.2017.12.009
31 Grace, K. T., & Anderson, J. C. (2018, October).
Reproductive coercion: A systematic review. Trauma, Violence & Abuse, 19(4), 371–390
https://doi.org/10.1177/1524838016663935
32. Boudreaux, M., Choi, Y. S., Xie, L., & Marthey, D. (2019, June). Medicaid expansion at Title X clinics: Client volume, payer mix, and contraceptive method type. Medical Care, 57(6), 437–443
https://doi.org/10.1097/MLR.0000000000001120
33. Weiti, K., & Manlove, J. (2021). Estimated reductions in unintended pregnancy among Delaware Title X family planning clients after a contraceptive access intervention. Child Trends.
https://www.childtrends.org/blog/estimated-reductions-inunintended-pregnancy-among-delaware-title-x-family-planningclients-after-a-contraceptive-access-intervention
34. Delaware Department of Health and Social Services, Division of Public Health. (2018). Reproductive health, Delaware Profile, 2012-2018, data Brief No.4.
https://dethrives.com/wp-content/uploads/2020/08/Data_Brief_ Reproductive_Health_PB_reviewed_team1.pdf
35. Barton, K., Redshaw, M., Quigley, M. A., & Carson, C. (2017, January 26). Unplanned pregnancy and subsequent psychological distress in partnered women: A crosssectional study of the role of relationship quality and wider social support. BMC Pregnancy and Childbirth, 17(1), 44 https://doi.org/10.1186/s12884-017-1223-x
36. Martin, C. E., Terplan, M., O’Grady, K. E., & Jones, H. E. (2018, July 11). Pregnancy intention and opioid use disorder treatment retention in the MOTHER study. The American Journal on Addictions https://doi.org/10.1111/ajad.12735
37. Frieden, T. R., & Houry, D. (2016, April 21). Reducing the Risks of Relief—The CDC Opioid-Prescribing Guideline. The New England Journal of Medicine, 374(16), 1501–1504. https://doi.org/10.1056/NEJMp1515917
140 Delaware Journal of Public Health - June 2023
Many people don’t think of themselves as caregivers, but if you offer support to someone living with a disability or an older adult, you are. Anything from taking someone to a health care appointment to helping with daily living is considered caregiving — and it’s hard work. But we can help you find reliable services and support, because your needs matter too. For help with resources, visit

they
to you, you can
us.
rides, meals, time? Get support.
If
turn
turn to
Give
DelawareADRC.com
1-800-223-9074. 141
or call
Blueprint Communities®
Provides training, technical assistance, coaching, and nancial support to groups of people from selected communities who seek to develop and implement plans that revitalize their communities.
https://www.bidenschool.udel.edu/ccrs/service/blueprint-communities-program
Bronchopulmonary Dysplasia
A form of chronic lung disease that a ects newborns, most o en those born prematurely and who need oxygen therapy.
Iatrogenic
Relating to illness caused by medical examination or treatment.
Necrotizing Enterocolitis
A life-threatening illness almost exclusively a ecting newborns due to extensive damage to the intestine and colon.
Periventricular Leukomalacia
A type of brain injury that a ects premature infants; small areas of brain tissue around the ventricles are a ected.
Ubiquitous
Found everywhere.
LEXICON
142 Delaware Journal of Public Health - June 2023
RESOURCES
The Arc of Delaware
https://thearcofdelaware.org
Delaware 2-1-1
https://delaware211.org
Delaware Housing Search
https://delawarehousingsearch.org
Delaware State Housing Authority
https://destatehousing.com
• Delaware State Rental Assistance Program (SRAP)
http://www.destatehousing.com/supportivehousing/media/srap.pdf
• Delaware Section 811
http://www.destatehousing.com/supportivehousing/media/811_faq.pdf
• Housing Development Fund
http://www.destatehousing.com/Developers/dv_hdf.php
• Low Income Housing Tax Credit Program
http://www.destatehousing.com/Developers/dv_lihtc.php
• Multi-Family Mortgage Revenue Bonds
http://www.destatehousing.com/Developers/dv_mfmrb.php
• Projects for Assistance in Transition from Homelessness (PATH)
https://dhss.delaware.gov/dhss/dsamh/pathgrant.html
Housing Alliance Delaware
https://www.housingalliancede.org
Housing Solutions & Service Organizations
https://helpingamericansfindhelp.org/delaware/delaware-housing-assistance/delaware-homeless-service-organizations/
United Way of Delaware
https://uwde.org
143
of

Index
Advertisers The Nation's Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23 American Public Health Association The DPH Bulletin - June 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 Delaware Division of Public Health The DPH Bulletin - May 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 91 Delaware Division of Public Health The DPH Bulletin - April 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 120 Delaware Division of Public Health Submission Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 146 Delaware Journal of Public Health 144 Delaware Journal of Public Health - June 2023
n Works best if taken within five days of symptoms starting.
n Helps reduce symptoms.
n Especially important for those age 50+ or unvaccinated.
Talk to your health care provider or learn more at de.gov/covidtreatments.
GOT COVID-19? GET TREATMENT.
If you test positive, treatment is available.
145
Public Health Delaware Journal of Submission Guidelines
updated April, 2020
About the Journal
Established in 2015, The Delaware Journal of Public Health is a bi-monthly, peer-reviewed electronic publication, created by the Delaware Academy of Medicine/Delaware Public Health Association. The publication acts as a repository of news for the medical, dental, and public health communities, and is comprised of upcoming event announcements, past conference synopses, local resources, peer-reviewed content ranging from manuscripts and research papers to opinion editorials and personal interest pieces, relating to the public health sector. Each issue is largely devoted to an overarching theme or current issue in public health.
The content in the Journal is informed by the interest of our readers and contributors. If you have an event coming up, would like to contribute an Op-Ed, would like to share a job posting, or have a topic in public health you would like to see covered in an upcoming issue, please let us know.
If you are interested in submitting an article to the Delaware Journal of Public Health, or have any additional inquiries regarding the publication, please contact DJPH Deputy Editor Elizabeth Healy at ehealy@delamed.org, or the Executive Director of The Delaware Academy of Medicine and Delaware Public Health Association, Timothy Gibbs, at tgibbs@delamed.org
Information for Authors
Submission Requirements
e DJPH accepts a wide variety of submission formats including brief essays, opinion editorials pieces, research articles and findings, analytic essays, news pieces, historical pieces, images, advertisements pertaining to relevant, upcoming public health events, and presentation reviews. If there is an additional type of submission not previously mentioned that you would like to submit, please contact a staff member.
The initial submission should be clean and complete, without edits or markups, and contain both the title and author(s) fulls name(s). Submissions should be 1.5 or double spaced with a font size of 12. Initial submissions must also contain a cover letter with concise text (maximum 150 words). Once completed, articles should be submitted via email to Elizabeth Healy at ehealy@delamed.org as an attachment. Graphics, images, info-graphics, tables, and charts, are welcome and encouraged to be included in articles. Please ensure that all pieces are in their final format, and all edits and track changes have been implemented prior to submission.
Cover Letters must address the following four article requirements:
1. A description of what the paper adds to current knowledge, in particular with respect to material previously published in DJPH, and if systematic reviews exist on the topic.
2. The public health importance of the paper.
3. One sentence summarizing the main message(s) of the paper, which may be used to disseminate the paper on social media.
4. For individual or group randomized trials, provide the date of trial registration and the NCT number from www.Clinicaltrials.gov or other approved registry. In the cover letter only, not in the paper. Do NOT include the trial registration or NCT number in the abstract or the body of the manuscript during the initial submission.
All manuscripts must be submitted via email to Elizabeth Healy at ehealy@delamed.org.
146 Delaware Journal of Public Health - June 2023
To view additional information for online submission requirements, please refer to the website for the Delaware Journal of Public Health: https://djph.org/sample-page/submit-an-article/

Submission Length
While there is no prescribed word length, full articles will generally be in the 2500-4000-word range, and editorials or brief reports will be in the 1500-2500-word range. If you have any questions regarding the length of a submission, or APA guidelines, please contact a staff member.
Copyright
Opinions expressed by contributors and authors do not necessarily reflect the opinions of the DJPH or affiliated institutions of authors. Copying for uses other than personal reference or interest without the consent of the DJPH is prohibited. All material submitted alongside written work, including graphics, charts, tables, diagrams, etc., must be referenced properly in accordance with APA formatting.
Con icts of Interest
Any conflicts of interest, including political, financial, personal, or academic conflicts, must be declared prior to the submission of the article, or in conjunction with a submission. Conflicts of interest are any competing interests that may leave readers feeling misled or deceived, and/or alter their perception of subject matter. Declared conflicts of interest may be published alongside articles in the final electronic publication.
Nondiscriminatory Language
Use of nondiscriminatory language is required in all DJPH submissions. The DJPH reserves the right to reject any submission found to be using sexist, racist, or heterosexist language, as well as unethical or defamatory statements.
Additional Documents and Information for Authors
Please Note: All authors and contributors are asked to submit a brief personal biography (3 sentences maximum) and a headshot along submissions. These will be published alongside final submissions in the final electronic publication. For pieces with multiple authors, these additional documents are requested for all contributors.
Abstracts
Authors must submit a structured or unstructured abstract along with their article.
The word limit is 200 words, including headings. A title page should be submitted with this abstract as well.
Structured abstracts should employ 4-5 headings: Objectives (begins with “To…”)
Methods Results Conclusions
A fifth heading, Policy Implications, may be used if relevant to the article.
Trial Registration information is required for clinical trials and must be included in the final version abstract
All abstracts should provide the dates(s) and location(s) of the study is applicable.
Note: There is no Background heading.
147
Delaware Academy of Medici ne / DPHA
P.O. Box 89 Historic New Castle, DE 19720 ISSN
www.dela med.org | www.djph.org
e Del aware Academy of Medicine is a private , nonprofit organization founded in 1930. O ur mission is to enhance the well being of our communit y through medical education an d the promotion of public health. O ur educational initiatives span the spect rum f rom consumer health education tocontinuing medical education conferences and symposia e Del aware Public Health A ssociation wa s officially rebor n at the 141 st Annual Meeting of the American Public He alth A ssociation (AHPA) hel d in B oston, M A in November, 2013. At this meeting, af filiation of t he DPH A wa s t ransferred to the Del aware Academy of Medicine officially on November 5, 2013 by action of the A PH A Governing Council . e Del aware Academy of Me dicine, who’s mission statement is “ to promote the well-being of o ur communit y through education and the promotion of public health,” is honored to take on t his responsibility in the First State
Follow Us: 2639-6378