



ISSUE 23.1 www.healthbusinessuk.net NET ZERO FACILITIES MANAGEMENT CYBERSECURITY PLUS: SIGNAGE | CLEAN AIR | CATERING | MEDICAL EQUIPMENT How can robots help patients and help the NHS? ROBOTIC SURGERY TECHNOLOGY
LET’S DO THIS!
At GE HealthCare, our insights come from you. First we listen. Then we act.
Community Diagnostic Centres can’t be silos within the system, and improving connectivity and digitisation across all aspects of diagnostics must be a priority.
Our digital solutions are designed to provide access to the right information at the right time. We help healthcare providers to aggregate and consolidate their data and turn it into actionable insights that help them to make the best decisions for their teams and ultimately their patients.

Let’s keep talking because together we can achieve amazing things.
Collaborate. Digitise. Transform.
Collaborate. Digitise. Transform.
www.gehealthcare.co.uk/campaigns/cdc
JB02285UK
Follow and interact with us on Twitter:
@HealthBusiness_
Tackling the twindemic
The NHS is coming through what has been described by many as its worst and most challenging winter on record, with the twindemic of Covid and flu.
Bed shortages, ambulance handovers and delayed discharges are all being highlighted as posing problems, along with the ongoing backlog.

Meanwhile many across the NHS are striking over pay, and concerns over conditions and patient safety, with little sign that these disputes will be solved soon.

This issue of Health Business includes features on the related topics of clean air, energy and net zero, the health problems these pose and what the NHS can do and is doing to tackle these issues.
There is a large technology section with articles on virtual health and how robotic surgery is helping patients as well as the NHS. Following the merge of NHS Digital and NHS England, we explore what NHS Digital does for the NHS.


As well as this, we investigate the cost of the NHS estate and include an interesting article on how to help patients, staff and visitors with wayfinding in hospitals.
 Polly Jones, editor
Polly Jones, editor
P ONLINE P MOBILE P FACE-TO-FACE
To register for your FREE Digital Subscription of Health Business magazine, go to www.healthbusinessuk.net/digital-subscription or contact Public Sector Information, 226 High Road, Loughton, Essex IG10 1ET. Tel: 020 8532 0055
www.healthbusinessuk.net
PUBLISHED BY PUBLIC SECTOR INFORMATION LIMITED

226 High Rd, Loughton, Essex IG10 1ET. Tel: 020 8532 0055 Web: www.psi-media.co.uk
EDITOR Polly Jones PRODUCTION MANAGER/DESIGNER Dan Kanolik PRODUCTION DESIGNER Jo Golding PRODUCTION CONTROL Deimante Gecionyte
ADMINISTRATION Enkelejda Lleshaj WEBSITE PRODUCTION Freya Courtney ADVERTISEMENT SALES Azad Miah, Maziar Movassagh
PUBLISHER Damian Emmins GROUP PUBLISHER Karen Hopps
© 2023 Public Sector Information Limited. No part of this publication can be reproduced, stored in a retrieval system or transmitted in any form or by any other means (electronic, mechanical, photocopying, recording or otherwise) without the prior written permission of the publisher. Whilst every care has been taken to ensure the accuracy of the editorial content the publisher cannot be held responsible for errors or omissions. The views expressed are not necessarily those of the publisher.ISSN 1478-7687
Health Business is a member of the Independent Press Standards Organisation (which regulates the UK’s magazine and newspaper industry). We abide by the Editors’ Code of Practice and are committed to upholding the highest standards of journalism. If you think that we have not met those standards and want to make a complaint please contact Polly Jones or Angela Pisanu on 0208 532 0055. If we are unable to resolve your complaint, or if you would like more information about IPSO or the Editors’ Code, contact IPSO on 0300 123 2220 or visit www.ipso.co.uk

ISSUE 23.1 www.healthbusinessuk.net NET ZERO FACILITIES MANAGEMENT CYBERSECURITY PLUS: SIGNAGE CLEAN AIR CATERING MEDICAL EQUIPMENT How can robots help patients and help the NHS? ROBOTIC SURGERY TECHNOLOGY
Comment
Issue 23.1 | HEALTH BUSINESS MAGAZINE 3
STAY SECURED WITH APOLLO


Soteria Dimension is an optical smoke detector that incorporates unique sensors that streamline the design and enable flush-mounting. There are two products for niche applications: Soteria Dimension designed to blend seamlessly into its environment, and Soteria Dimension Specialist designed with an anti-vandal and anti-ligature metal faceplate to protect the most vulnerable in care and custody.



DETECTION > REFINED
APOLLO-FIRE.CO.UK SCAN HERE TO FIND OUT MORE ABOUT SOTERIA DIMENSION! QR CODE
> SECURED
Contents Health Business 23.1
07 News
Urgent and Emergency Care delivery plan announced; Plans to cut delayed discharge in Scotland; 86 million vaccine appointments booked online
17 Facilities Management
NHS Digital recently published its Estates Returns Information Collection for 2021/22 which sets out information relating to the costs of providing and maintaining the NHS Estate including buildings, maintaining and equipping hospitals, the provision of services and the costs and consumption of utilities

22 National NHS Estates Conference
The National NHS Estates Conference takes place in London on 19th April with a focus on backlog, energy and the workforce
25 Signage
Dr Colette Jeffrey Associate Professor of Wayfinding at Birmingham City University on why hospital wayfinding is so difficult
31 Clean Air
In December, Chief Medical Officer Professor Chris Whitty, published his annual report, this time, on air pollution
34 The Health & Safety Event
The Health and Safety Event is the UK’s premier event dedicated to improving occupational health and safety standards, opening its doors on 25-27 April 2023 at the NEC in Birmingham
37 Energy
December 2022 marked the opening of Devizes Health Centre in Wiltshire to patients. But what makes this site so special? And how is it helping to tackle climate change? James Wakeham, principal construction manager at NHSPS explains
43 Net Zero
The NHS is the first health service in the world to embed net zero into legislation, with a goal of reaching net zero by 2040. Here we look at the Green Plan of the Leeds Teaching Hospitals NHS Trust


47 Catering
NHS England published updated national standards for healthcare food and drink in November. HB investigates
50 Winter Pressures
Helen Hunt, innovation programme manager (Workforce) at the West Midlands Academic Health Science Network explains how the NHS Insights Prioritisation Programme is helping to address winter pressures
53 IT
NHS Digital has now officially merged with NHS England; HB takes a look at what the NHS’s IT hub does

57 Cybersecurity
Phil Howe, CTO of Core to Cloud and Richard Staynings, cybersecurity strategist at Cylera on cybercrime prevention
60 UK Cyber Week
UK Cyber Week – Expo & Conference is taking place at the Business Design Centre, London on 4 and 5 April 2023

63 Digital Health Rewired
Digital Health Rewired returns on 14-15 March 2023 bringing the UK’s digital health community together at a pivotal time for the sector
73 Technology
Equipping the modern nursing workforce for realities they face using new technologies to enhance access requires new thinking around education, writes Professor Ann-Marie Cannaby, senior nurse and member of the clinical advisory board for BT
75 Technology
The 999 BSL service enables people with hearing or speech loss to be connected to a video call with a BSL interpreter in order to make 999 calls by video
77 Technology
NHS Golden Jubilee has recently performed its 1,000th robotic orthopaedic joint replacement - HB looks at the hospital’s robotics programme

81 Medical Equipment
Researchers at the University of Nottingham have recently been awarded a £6 million grant from the Engineering and Physical Sciences Research Council (EPSRC) in order to develop a toolkit for 3D printing. HB spoke to Ricky Wildman, Professor in Chemical Engineering at The University of Nottingham
Contents 37 53 57 77 Health Business magazine www.healthbusinessuk.net
43 Issue 23.1 | HEALTH BUSINESS MAGAZINE 5







Brilliance 7000 27” (68.6 cm) | Mini LED | Thunderbolt 4 | 4K UHD 27B1U7903/00 MINI LED Local Dimming MiniLED with Thunderbolt docking Simply brilliant Monitors
Urgent and Emergency Care delivery plan announced


(including 100 specialist mental health vehicles) and 5,000 more sustainable hospital beds.

The plan comes during record demand for NHS services, with the latest data showing more A&E attendances than ever before, growing numbers of the most serious ambulance call outs, and millions of NHS 111 calls a month over winter.
The NHS and the government have published a two-year delivery plan to help recover urgent and emergency care services, reduce waiting times, and improve patient experience.
The delivery plan for recovering urgent and emergency care services is a 49-page document which sets out how the government expects patients to be seen more quickly in emergency departments, with the ambition to improve to 76 per cent of patients being admitted, transferred or discharged within four hours by March 2024. Category two ambulance response times will be improved to an average of 30 minutes over the next year, with further improvements expected by in 2024/25.
Backed by a £1 billion dedicated fund, the plan provides for 800 new ambulances
MENTAL HEALTH
Urgent care provided in the community will be expanded to ensure people can get the care they need at home, without the need for a hospital admission.
The number of emergency medical technicians will also be expanded alongside greater use of student and apprentice paramedics and training more staff in mental health.
NHS chief executive, Amanda Pritchard, said: “The NHS has been under more pressure than I have ever known in my 25 years working in the service – the threat of the ‘twindemic’ of flu and covid became a reality and that was alongside huge demand for all services – from ambulance and A&E services to mental health and GP appointments.
“We are incredibly grateful to the NHS staff who work day-in, day-out to deliver care to hundreds of thousands of people and for the
extensive preparations put in place ahead of winter.
“We introduced more call handlers, more beds and 24/7 system control centres to manage increased demand, and this new plan sets out how we will boost that progress and help improve the experiences of patients who will benefit from quicker, better care, in the right setting.
“The front door to the NHS is often where we can see the pressures build up – and to relieve that pressure, we will continue to work with social care colleagues to free up space in hospitals so that people who are well enough to leave can be discharged and get the care they need at home or in the community.
“The history of the NHS is one of change and innovation and so, while striving to meet the needs of today’s patients, we are also looking to the future of the NHS and will shortly set out our workforce plan – which is a once in a generation opportunity to put the NHS on a sustainable footing.”

READ MORE
£150 million for mental health services
“These dedicated facilities will ensure patients experiencing a mental health crisis receive the care they need in an appropriate way, whilst freeing up staff availability including within A&E departments.
“These schemes – along with the up to 100 new mental health ambulances – will give patients across the country greater access to high-quality, tailored support when needed the most.”
The Department of Health and Social Care has announced £150 million for mental health services.

The money will be used to build 150 new facilities to support mental health urgent and emergency care services. Funding will be spent on more tailored emergency care and support in the community, with specialised mental health ambulances, more crisis services and improved health-based places of safety.
The funding will allow for the procurement of up to 100 mental health ambulances and 150 new projects centred on supporting the provision of mental health crisis response and urgent mental health care - this includes over 30 schemes providing crisis cafes, crisis houses and other similar safe spaces, as well as over 20 new or improved health-
based places of safety which provide a safe space for people detained by the police. Programmes will also focus on preventative measures, including improvement of sanctuary spaces, to improve mental wellbeing, and community mental health facilities that will work to help people before reaching crisis point.
There will also be improvements to NHS 111 and crisis phone lines.
The announcement comes amid recent report of crisis in mental health services. Health and social care secretary Steve Barclay said: “With the health systems facing huge challenges this winter from the rise in flu, ongoing Covid cases and the impact of the pandemic, we need to ensure people are still receiving the right specialist care.
NHS mental health director Claire Murdoch said: “Despite the disruption caused by the pandemic the NHS is on track to deliver its Long Term Plan commitment to boost mental health spending by £2.3 billion a year, enabling around 4.5 million adults and over 700,000 young people to access mental health services.
“As well as expanding capacity to meet record demand, the NHS is transforming mental health services to help people get more appropriate care when they contact services and this investment will see specialist mental health ambulances deployed, new crisis cafes opened, and existing facilities modernised, to deliver urgent and emergency mental health care to more people who need it.
“So as ever anybody in need of help should not hesitate in contacting the NHS so they can get the care they need.”
READ MORE
EMERGENCY CARE
News
7 Issue 23.1 | HEALTH BUSINESS MAGAZINE
Proud to be the People Who Care
ISS has developed forward-thinking facilities management solutions that transform healthcare for those who need it most. Providing services from cleaning and catering to hard FM, maintenance and portering, ISS prioritises patient wellbeing with a truly people-focused, patient-first approach. With more than 35 years of close collaboration with the NHS, discover why we’re the people who care .


SEARCH ONLINE:
ISS People Who Care

PEOPLE MAKE PLACES

Issue 23.1 | HEALTH BUSINESS MAGAZINE 8
Plans to cut delayed discharge in Scotland
discharged and who can safely move home or to another setting like an interim placement in a care home.
Patients are only to be discharged if deemed safe and clinical risk assessments will take into account the capacity of social care and social work and the potential impact on families or carers of patients.
The Scottish government has announced plans to reduce delayed discharge.
Patients who do not need to remain in hospital will be reassessed as soon as possible so they get the right care, in the right place, at the right time.
Each health board area is to identify patients who are clinically safe to be
IT professionals invited to share views on future of NHS IT systems



NHS England is to hold bi-monthly webinars to encourage people to get involved in how technology can meet the current and future needs of patients, staff and citizens.
The next webinar, Spine Futures, is scheduled for Thursday 23 February. The webinar is targeted for those working in IT in health and care who would like to hear about plans for the Spine of the future and share their needs.

Currently, NHS Spine joins together more than 28,000 healthcare IT systems and sends over 47 million messages a day, allowing messages to be shared securely through services like the Electronic Prescription Service, Summary Care Record and the e-Referral Service.
Work has been ongoing since April 2022 to develop a new platform to modernise NHS Spine over the next two to three years. The programme plans to make use of modern technologies to create a cloud-based Spine of the future.
Stephen Koch, executive director for platforms at NHS England, said: “We want the Spine of the future to make the best use of modern technologies and open standards to ensure it meets the needs of NHS users for many years to come.
“That’s why we’re actively engaging the health and care system with the development of the Spine Futures programme.
“Last year’s migration of the MESH service to the cloud was a massive achievement for the teams involved and a significant first step in our Spine Futures programme. §“We’re asking colleagues working in health and care to tell us what they need from the Spine of the future as we take the next steps of our journey to transform IT in health and social care.”
Last week the Scottish Government announced £8 million of funding for an extra 300 interim care beds.
Health Secretary Humza Yousaf said: “First and foremost, we know hospital is not a good place to be for people who are medically fit to leave, because it can lead to them becoming weaker or less independent. That’s why it’s so important they can
GENE THERAPY

move home, or to a homely setting, as soon as possible.
“We believe this will also help to alleviate pressure on our NHS by freeing up beds and improving the flow of patients through hospitals. It is also, crucially, in the best interest of the people concerned.
“If we can reduce delayed discharge there is more chance that beds will be available for people who need them. We hope that these reviews will also contribute to reducing some of the pressures our hospitals are facing.”
First baby receives NHS gene therapy

A 19-month-old has become the first child in the UK to receive a life-saving gene therapy treatment for metachromatic leukodystrophy (MLD).
MLD causes severe damage to a child’s nervous system and organs and those affected have a life expectancy of between five and eight years. The most common form of MLD usually develops in babies younger than 30 months and can lead to loss of sight, speech and hearing, as well as difficulty moving, brain impairment, seizures and eventually death in childhood.
The treatment is available on the NHS at Royal Manchester Children’s Hospital, in collaboration with Manchester’s Centre for Genomic Medicine at Saint Mary’s Hospital, which are both part of Manchester University NHS Foundation Trust (MFT). It is the only site in the UK providing the treatment and one of five sites in Europe.
The baby girl, Teddi, is the first person in the UK to receive the treatment outside of a trial. The treatment began when she was 12 months old, with the removal of stem cells at the end of June. The stem cells were treated and a transplant took place in August. Teddi was discharged back to her home in October. Teddi is healthy and showing no signs of the disease.
Teddi’s sister Nala was also diagnosed with MLD, however she was not eligible for the treatment, as the clinical guidance requires the gene treatment to be administered before the irreversible damage caused by the disease progresses too far.
Professor Rob Wynn, consultant paediatric haematologist at Royal Manchester Children’s Hospital director of the hospital’s Paediatric Bone Marrow Transplant Programme, said: “Being able to offer this first licenced treatment as part of NHS standard of care and, crucially, transform Teddi’s life, has been an exciting experience for all of us involved here in Manchester – staff, researchers, patients and families.
“Through the years, colleagues and I have looked after a range of patients with rare but severe conditions, where treatment has been limited. It is wonderful to be involved in this breakthrough moment and deliver a gene therapy which will transform outcomes for patients with MLD.
“It has been wonderful to care for Teddi and the Shaw family and our entire team wishes them well as she continues her recovery at home.”
DELAYED DISCHARGE IT
News
MORE READ MORE READ MORE
READ
9 Issue 23.1 | HEALTH BUSINESS MAGAZINE
Secure I.T. Environments Ltd

Is a leading UK-based international design and build data centre specialist, providing Modular, Micro, Edge, and Containerised secure data centres. We have a history of delivering high quality, energy efficient, and innovative solutions for NHS customers throughout the UK and channel islands, with a powerful combination of delivery excellence, management, and expertise.




For more information on how we can assist you plan and implement the most energy efficient data centre solution contact our design team on: 01983 885 182 www.siteltd.co.uk



Staff working with children and young people to receive mental health training
to help them spot the signs that a child or young person might need mental health support.
The programme will be delivered in partnership with the Anna Freud Centre, the National Children’s Bureau and the Charlie Waller Trust.
Thousands of staff who work with children and young people are set to receive mental health training thanks to a new pilot commissioned by Health Education England. Staff including youth workers, sports coaches and librarians will receive training

BACKLOG
10,000 staff across the pilot sites in Southampton, Portsmouth and Norfolk will be able to access the training. The training is currently being designed with children and young people, parents and carers and staff members, before the six-month pilot begins.
It is hoped the training will be rolled out nationally and cover sectors such as education, early years and childcare, physical
19 community diagnostic centres to open this year
health, library services, sports clubs, justice and crime prevention, youth and social, family and community services.



The training will cover emotional health, including how to speak to children and young people about mental health concerns and what to say, offering support and signposting resources, and where to go for more specialist help, as well as how to recognise signs of anxiety, low self-esteem and loss of social confidence, providing practical skills on how workers can help and when to ask for more specialist support.
DIGITAL
86 million vaccine appointments booked online

According to NHS England, more than 86 million Covid vaccinations have been booked on the NHS’s online booking system since its launch two years ago.

The national booking service launched in January 2021 and is managed by NHS England. The booking services allows people to book their vaccine online or via 119.
The service was integrated with the NHS App in December 2022 and around one in eight vaccination bookings are now made using the NHS App.
19 new community diagnostic centres (CDC) are to open later this year and are set to perform 1.1 million tests, checks and scans.
92 already-in-use CDCs have already delivered three million checks since the programme started in July 2021, as part of the elective recovery plan and aims to reduce the backlog.
CDCs are based in locations such as shopping centres and football stadiums and contain equipment including MRI, CT, X-ray and ultrasound scanners. They also provide blood tests or heart rhythm and blood pressure monitoring.
Milton Keynes, Nottingham and Dorset are set to get a new CDC this year.
Health and social care secretary Steve Barclay said: “Rapid diagnosis offers reassurance to patients, reduces waiting lists, and, crucially, saves lives.
“CDCs have been fundamental to this effort, delivering over 3 million extra tests which are helping to diagnose conditions from cancer to lung disease more quickly across the country.

“The new centres will take us even further, utilising cutting-edge MRI, CT and X-ray
machine to transform the way we deliver care closer to people’s homes helping tens of thousands of people.”
NHS national director of elective recovery, Sir James Mackey, added: “The NHS’s ambitious elective recovery plan, published just over a year ago, had these innovative ‘one stop shops’ at its heart. Since then they have played a key role in helping us virtually eliminate the number of people waiting more than two years for treatment and keeping the NHS on track to do the same for people waiting over 18 months by the end of April, with the centres – often based in convenient places such as in shopping centres, high streets and community hospitals - now having delivered an incredible 3 million tests and checks.
“These 19 new centres will boost access for tens of thousands more patients and build on the great work of NHS staff in recovering services, helping the NHS deliver an extra 9 million tests a year by 2025 – an increase in capacity of more than a quarter on prepandemic levels.”
The service has also been expanded to include flu vaccinations at pharmacies, with more than 207,000 flu jabs booked since the expansion in October 2022.
Helen Clifton, executive director of product delivery at NHS England, said: “Back in early 2020, no-one could have envisaged that we were about to design and create a system of this scale in such a short timeframe, so we’re immensely proud that the National Booking Service has enabled millions of people to book their jabs quickly and easily.
“The fact that it’s now being used for flu vaccinations is not only testament to its success, but also a great example of existing digital services being adapted and enhanced to meet the needs of patients.”
News
MENTAL HEALTH
MORE READ MORE READ MORE
READ
11 Issue 23.1 | HEALTH BUSINESS MAGAZINE










www.avereurope.com WE CARE! Medical Grade PTZ Camera PRECISION DIAGNOSIS
without boundaries in telemedicine, tele-ICU and live surgery broadcasts all over the world.
Connecting
NAO report highlights pressure on mental health services
survey of NHS mental health trusts highlighted specific concerns about shortages of medical and nursing staff, and psychologists. Reasons for shortages include difficulties recruiting and retaining staff, high turnover between service areas, and competition from health and nonhealth sectors.

In its latest report, the National Audit Office (NAO) estimates that as many as 8 million people with mental health needs are not in contact with NHS services.
The NAO report Progress in improving mental health services in England explains that whilst the NHS has taken some important first steps towards closing the gap between mental and physical health services, these services remain under pressure and many people using them are reporting poor experiences.
NAO interviews with stakeholders highlighted that some groups, including children and young people, ethnic minorities, LGBT people, and those with more complex needs or more than one diagnosis, had poorer
experiences accessing or using services.
A survey of NHS mental health trusts revealed that in response to demand and service pressures, they had allowed waiting times and lists to increase, while a minority had raised treatment thresholds (15 out of 33) and reduced provision in some service areas (6 out of 33).

The NHS mental health workforce increased by 22 per cent between 2016-17 and 202122, but staff shortages and the speed of expanding the existing workforce remain a major constraint. Retaining staff is also becoming an increasing challenge: during 2021-22, 17,000 staff (13 per cent) left the NHS mental health workforce. The NAO’s
Gareth Davies, the head of the NAO, said: “The Department for Health and Social Care and NHS England have made a series of clear commitments and plans to improve mental health services, but they have not defined what achieving full parity of esteem for mental health services will entail. It is therefore unclear how far the current commitments take the NHS towards its end goal, and what else is needed to achieve it and match the increasing public awareness and need.
“While funding and the workforce for mental health services have increased and more people have been treated, many people still cannot access services or have lengthy waits for treatment. With demand for mental health services having increased since the pandemic and being expected to increase further in the coming years, it is vital that DHSC and NHSE define what is required to meet the growing demand.”
READ MORE
Welsh Government launches workforce implementation plan
With the World Health Organisation predicting a worldwide shortfall of 10 million health workers by 2030, the Welsh Government has published a new strategy to address the challenges of staffing NHS Wales.
The National Workforce Implementation Plan is designed to ensure the NHS in Wales remains fully staffed and includes a campaign to ethically recruit more nurses from overseas.
A recruitment drive is planned for later in 2023, which follows on from last year’s successful ‘Once for Wales’ pilot campaign. This led to around 400 nurses joining the NHS.
There are also plans to create an ‘AllWales Collaborative Bank’ to enable the NHS to address short-term staffing issues and provide staff with choice and flexibility, while encouraging a move away from agency working which cost NHS Wales £260 million last year.
The Welsh Government will issue detailed plans for specific professions and services such as nursing, dentistry and pharmacy over the next two years.
Eluned Morgan, the minister for health and social services, said: “Our health workforce has reached record numbers in Wales, to help meet the increasing demand on its
services. But we are seeing demand for health and social care like never before, in Wales and across the world.
“Our plans are based on what NHS staff have been telling us - that rapid action is needed in key areas now.
“The message is clear: we must accelerate our action, with strong, collective and



compassionate leadership, if we are to improve retention and recruitment. It’s vital we provide our workforce with the working environment it needs to continue to provide world-class care for the people of Wales.”
READ MORE
News
MENTAL HEALTH
WORKFORCE
13 Issue 23.1 | HEALTH BUSINESS MAGAZINE

95 per cent of prescriptions now electronic
Almost one billion prescription items have been dispensed electronically in the last 12 months, with less than 1 in 20 still paper-based, according to NHS Digital (now merged with NHS England).
The Electronic Prescription Service (EPS) issued 996 million (95 per cent) prescriptions in 2021/22, compared with 532 million in 2016/17 when just under half (48 per cent) were still issued on paper.



The number of electronic prescriptions sent to community pharmacies has almost doubled in the past five years, with 11,400 pharmacies now signed up, according to figures highlighted by NHS England to mark the 18th anniversary of the service.
The total number of prescription items dispensed each year has also grown from
NET ZERO
Following the hottest summer on record, University College London Hospitals NHS Foundation Trust has added an additional 452 solar panels on its hospital roof as part of its strategy to reach net zero ahead of the wider NHS target.

The panels form part of a new strategy ‘Critical Care For Our Climate’, which aims to build sustainability in key areas such as clinical care, procurement and supply chain, estates, technology, transport, education and engagement.
The NHS has set a nationwide target of achieving a net zero carbon footprint by 2040. UCLH wants to achieve this by 2031. For indirect emissions (those it can influence along its supply chain), UCLH aims to achieve net zero by 2040, five years ahead of the NHS England target.
Including the panels, UCLH has invested over £2m in energy saving measures such as LED lights in the last week.
Elliott Westhoff, UCLH programme lead for sustainability, said: “The strategy has been put together after extensive consultation. We are grateful to all staff and our partner organisations for the ideas and enthusiasm they have contributed so far, and look forward to working with colleagues across UCLH to deliver net zero.”
1.02 billion in 2016/17 to 1.04 billion in 2021/22, with 11,400 pharmacies now signed up to using the electronic service.
Rahul Singal, chief pharmacy and medicines information officer at NHS England, said: “When you look at the number of transactions that are made via the service and how much it’s revolutionised practice in general practice and community pharmacy, we’d be pushed to think of another national system that’s had more success.
“Our next focus is to introduce EPS into more care settings, including more health settings such as hospital outpatient departments so the benefits can be realised for even more clinicians and patients across the NHS.”
CYBERSECURITY
Midlands Partnership NHS Foundation Trust is the first secondary care provider in England to implement EPS. Dr James Briscoe, consultant psychiatrist in their Early Intervention team, said: “It is not too dramatic to state that EPS has revolutionised my practice. I can now write and deliver prescriptions in five minutes compared to the time and effort it took to handwrite a prescription from scratch, arrange for it to be collected by the service user or a member of the team or hand deliver it to a pharmacy. A huge time saving with inbuilt safeguards to enable safe prescribing.”
READ MORE
NHS Digital adds new cybersecurity resources

NHS Digital has updated its security awareness toolkit Keep I.T. Confidential with more cyber security resources to help support clinical settings and social care organisations to improve security culture within their workplace.
NHS and social care organisations are urged to take advantage of the new resources, which are designed to raise awareness of the threat of ransomware.
There are two sets of campaign materials, one for staff in clinical settings and one for staff in the adult social care sector.
The resources are designed to help organisations run their own cybersecurity awareness when it suits them.
Launched by NHS Digital’s Data Security Centre, the aim of the materials is to improve staff knowledge of topics such as phishing, unauthorised data sharing, unlocked screens and weak passwords.

Materials that are included in the toolkit include screensavers, digital banners, sticky notes, social media graphics and an animation. NHS Digital’s executive director of cyber operations Mike Fell said: “Good security practices are our shared responsibility and being cyber aware can significantly reduce the chance of cyber events affecting people’s care.
“We know how busy staff are, but we encourage everyone to prioritise reducing security risks as much as they can to protect the NHS and social care against vulnerabilities.
“Taking small, simple steps and considering security in your day-to-day work can make a huge difference and we hope that these resources can really play a part in helping to drive that change.”
READ MORE
DIGITAL
New solar panels at UCLH aim to help hit net zero early
News
READ MORE
15 Issue 23.1 | HEALTH BUSINESS MAGAZINE



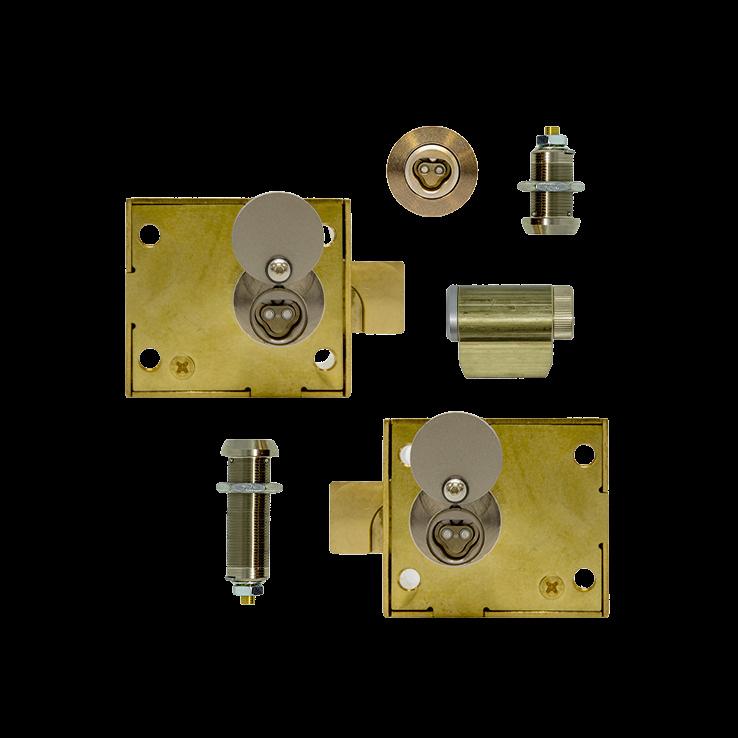



WWW.OPTIMUSIT.CO.UK CLICK HERE TO CONTACT US NOW BY EMAIL SAVE TIME AND MONEY WHILST GAINING GREATER EFFICIENCIES AND SECURITY. SUITABLE FOR HOSPITALS, CLINICS AND SURGERIES ONE KEY FOR ALL YOUR LOCKS DOORS | CABINETS | SENSITIVE EQUIPMENT | IT FACILITIES | MOBILE ASSETS www.sellox.co.uk www.cyberlock.com
The cost of the NHS estate
NHS Digital recently published its Estates Returns Information Collection for 2021/22 which sets out information relating to the costs of providing and maintaining the NHS Estate including buildings, maintaining and equipping hospitals, the provision of services and the costs and consumption of utilities
The results from the 2021/22 Estates Return Information Collection (ERIC) are a mandatory collection for all NHS trusts including ambulance trusts. The results include information on the costs of providing and maintaining the NHS Estate including buildings, maintaining and equipping hospitals, the provision of services such as laundry and food, and the costs and consumption of utilities.

Estates and Facilities is the third highest cost for the NHS, so the information from the report is useful and relevant in many ways.
NHS Digital worked with stakeholders and data providers during the data collection, to improve data quality. This cooperation included a data assurance exercise with stakeholders and data providers and data definition refinement.
Scope and use

The report includes national and local level information from the ERIC return covering the period 1st April 2021 to 31st March 2022, with data from all NHS organisations in England providing NHSfunded secondary care during the fiscal year ending 31st March. The data from ERIC is used by the Department of Health and Social Care (DHSC) and Arm’s Length Bodies (ALBs) to determine efficient use of funding. They also use it to make policy decisions.
Other government departments will also look at the data. For example, budgets for NHS expenditure are approved by the Treasury and ERIC provides evidence of expenditure in relation to Estates and Facilities. NHS regulators use the data in their review process and when making decisions on inspections. Trusts also use the data to benchmark themselves against other trusts to establish relative levels of efficiency, safety and quality. The data is also
Feature Heading
Facilities Management
Issue 23.1 | HEALTH BUSINESS MAGAZINE 17
andEstatesFacilities is the third highest cost for the NHS, so the information from the report is useful and relevant in many ways





The Key Replacement Service Tel: 020 8343 2943 Email: sales@keysplease.co.uk HELP! We’ve lost our keys! KEYS FROM AS LOW AS £1.79* CALL FOR DETAILS quoting BFK23 www.keysplease.co.uk *Contact us for further details on this offer NEW YEAR SPECIAL OFFER www.healthbusinessuk.net Click here for your FREE subscription and to receive the latest issue and newsletter direct to your inbox Follow us on Twitter: Published by 020 8532 0055 www.psi-media.co.uk BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 18
Costs
The results show that the total costs of running the NHS estate were £11.1 billion, which is an 8.8 per cent increase compared to 2020/21. 2.8 billion was spent on Hard FM costs and 3.3 million was spent on Soft FM. 215 million was spent on management of Hard and Soft FM costs.
Capital investment for new build saw a 23 per cent increase, while capital investment for changing/improving existing buildings saw a 3.6 per cent increase and capital investment for maintaining existing buildings saw a 4.25 per cent increase. Meanwhile capital investment for equipment saw an 8 per cent decrease.
Private sector funding investment decreased 38.5 per cent from £160.7 million to £98.9 million. Meanwhile, public sector funding investment increased 9.9 per cent from £3.7 billion to £4.1 billion and charity and/or grant funding investment saw a 77.7 per cent increase from £139 million to £247 million.
Energy
The total energy usage from all energy sources across the NHS estate was 11.7 billion kWh. This represents a 2.6 per cent increase compared to the previous year. Energy costs rose 21.08 per cent from £652.7 million to £790.3 million.
Electrical energy output of owned onsite renewables saw a 34.18 per cent increase from 5.7 million kWH to 7.7 million kWH.
The amount spent on backlog maintenance, was £10.2 billion – an 11 per cent increase
since 2020/21. Backlog maintenance is a measure of how much would need to be invested to restore a building to a certain state based on a state of assessed risk criteria. Planned maintenance work is not included in this stat. Cleaning services cost £1.2 billion – an increase of 7.5 per cent since 2020/21. Water and sewage costs increased 3.41 per cent to £89.1 million.
The total cost of waste disposal increased 7.15 per cent to £152.8 million. This includes incineration of clinical waste and alternative treatment of clinical waste and domestic waste including landfill, recycling and food.
Other costs
Interestingly, the cost of storing medical records is also included. For 2021/22, this was £234.3 million, of which £175.3 million was on site and £58.9 million was for offsite. The report also included information on how medical records were stored. 12 trusts (excluding ambulance trusts) use paper-based medical records – no change from the previous year. Four trusts use electronic medical records, this is down from seven. 186 use a mix of paper and electronic records – a decrease of one. 98 trusts have an in-house medical record
service provision, while 10 have an external or contracted one. 92 have a hybrid model. Car parking is also included. The cost of car parking services to the NHS is £71.4 million – an increase of 8.89 per cent. The number of electric vehicle charging points has increased 69.81 per cent from 1,411 to 2,396.
Inpatient food services saw a 6.85 per cent increase from £617.8 million to £660.2 million. Meanwhile, the total cost of laundry and linen saw an 8.89 per cent increase from £205.9 million to £224.2 million.

The cost of portering services increased 5.21 per cent from £351.5 million, to £369.9 million.
The report also presents fire safety metrics. In 2020/21, 1159 fires were recorded, compared to 1175 the year before. A small change of 1.36 per cent. There was a 4.88 per cent increase in fire alarms, with 20,511 false alarms recorded in 2021/22. 5982 of these resulted in a call out. There were no deaths resulting from fires for the second year in a row and the number of people injured in a fire decreased to 31, from 51 the previous year. L
FURTHER INFORMATION
View the report here
Facilities Management
The amount spent on backlog maintenance, was £10.2 billion – an 11 per cent increase since 2020/21
Issue 23.1 | HEALTH BUSINESS MAGAZINE 19

How can NHS Trusts stop paying more Business Rates than they need? By engaging trusted specialists. Knapman Roocroft Limited was awarded the top score of 93% by NHS Shared Business Services in 2022 for rating support services. We save NHS Trusts money, and operate on an ethical, carbon zero basis. Our service minimises the work burden on NHS Estates and Finance teams. Appoint us through an efficient, FTS compliant direct award, hosted by NHS Shared Business Services. Call: 01244 911 953 | Email: info@knapmanroocroft.co.uk Herons Way, Chester Business Park, Chester, CH4 9QR Visit our website: www.knapmanroocroft.co.uk/nhs Schedule a Call
NHS business rates: maximising savings, accurate budgeting and new responsibilities
Business rates have been a fact of life for the NHS since 1991 but following the Government’s Fundamental Review of Rating in 2021 the picture is changing. The average increase in Rateable Values for NHS healthcare properties from 1st April 2023 is more than 30% but irrespective of the increase, we know from our own research that many of the valuations are wrong. As a result, on the one hand you may need the tools to maximise rates savings and on the other you may not know you’re
not paying enough
property, information about the tenancy etc, trade, accounts and build cost information (where relevant to the valuation).
How can you make rates savings and fulfil your legal obligations without additional workload?
In this article, we will outline some of the key considerations for NHS Estates and Finance teams. We will suggest a trusted and efficient route to securing rates savings and also ensuring there are no nasty surprises in store from backdated increases.
Staying on top of rates liabilities for a dynamic NHS estate
NHS Estates teams are focused on core objectives; looking after NHS buildings and grounds for staff and patients and making sure goods and patients are where they need to be so care is received at the right time and the right place. They don’t have spare capacity for lengthy engagement with business rates advisors pursuing savings initiatives that may only serve the advisor’s interests with no realistic prospect of tangible results for NHS Trusts.
Fortunately, there are options available to appoint trusted specialist business rates advisors through NHS Shared Business Services. Trusted advisors know the right questions to ask and the information to assemble and won’t waste your time.
Trusted advisors will establish NHS Trusts’ key requirements at the outset including: Savings targets, benefits to host communities and satisfying HMRC reporting requirements.
How can you benefit from the NHS Shared Business Services Framework?
NHS SBS have completed a detailed procurement exercise to ensure a select group of suppliers meet all legislative requirements. NHS Trusts now have a route to market through the Hard Facilities Management 2 framework reference: SBS10166.

Key Benefits: Free and quick to access, FTS compliant for all UK public sector bodies, trusted specialist business rates advisors, competitive pricing, and skills, experience, and services specifically developed for NHS requirements.
What are your legal responsibilities (to HMRC) as the ratepayer?
Currently, there is no mandated requirement for ratepayers to notify either the Valuation Office Agency or Billing Authority about changes to properties, rental agreements etc. This means rating assessments are not accurate and local authorities are not receiving the correct amount of tax.
Following the Government’s ‘Fundamental Review of Rating’ there is a commitment to more frequent revaluations for business rates purposes and a fundamental change to ratepayer’s legal responsibilities.
Planned changes from 2023
In a move towards self-declaration to align with other forms of tax, the Government aims to strengthen the business rates system by improving the accuracy of rating lists and ensuring ratepayers pay the right tax to local authorities.
All ratepayers will be required to provide information to the Valuation Office Agency within 30 days, including: changes to property characteristics that affect business rates and mandatory disclosure of rent and lease information.
In addition, the Government is considering introducing a general ‘Duty to Notify’ to enable the Valuation Office Agency to carry out its valuation function. Ratepayers will be required to provide: Information about the
The Awarded Suppliers under NHS Shared Business Service Framework – Hard Facilities Management 2 are experts in valuation for business rates purposes of NHS hospitals and health centres. They have the resources to maximise rates savings and provide associated attendance to minimise the burden to NHS colleagues. Under flexible contract terms, the Awarded Suppliers can handle all communications with the Valuation Office Agency/ HMRC and Billing Authorities as new responsibilities are introduced from 2023.
Accurate budgeting forecasting and latent liabilities
The inaccuracies in many NHS rating assessments brought on by a lack of resources at the Valuation Office Agency over many years can present problems for NHS Trusts. Valuation corrections and separate assessments for different occupations on hospital sites can be backdated, triggering large and unexpected rates bills as many NHS Trusts have discovered over the last few years. An NHS SBS Framework Agreement Supplier will have in-depth experience dealing with the complexities of NHS estates combined with expert knowledge of rating law. They can ensure you have accurate estimates for budgeting purposes, for errors in existing rating assessments and proposed capital expenditure. They will ensure you’re not paying too much and be able to identify unexpected latent rate liabilities. L
Advertisment Feature
INFORMATION
info@knapmanroocroft.co.uk knapmanroocroft.co.uk/nhs
FURTHER
01244 911 953
Issue 23.1 | HEALTH BUSINESS MAGAZINE 21
Building a smarter, greener healthcare estate with community at its centre
The National NHS Estates Conference takes place in London on 19th April with a focus on backlog, energy and the workforce

Our healthcare sector has seen significant changes in its estates over the past few years, with evolving technology, improved energy substitutes and sustainable building practices and materials being at the forefront of the sector’s crucial patient care initiative. However, while waiting periods for treatment are not new, a report by the British Medical Association has shown that more patients than ever are now on the NHS waiting list for consultant-led elective care, with a record high of 7.21 million people as of October 2022. Figures from a recent King’s Fund report show how the total cost to eradicate the building and equipment maintenance backlog in the NHS has doubled from £4bn in 2011/12 to £10bn in 2021/22. In a time of COVID-19 recovery, funding and workforce shortages and risks of increased health and safety risks, an investment in current and new facilities is desperately needed for a more sustainable future, focused on highquality patient care and staff wellbeing. In last year’s Smart Asset and Estate Management Conference, top public sector leaders and industry experts convened to cover various solutions and strategies to tackle the growing maintenance backlog, achieve Net Zero targets and transform civil
service workplaces through the creation of government hubs. The healthcare estate faces similar challenges which have been amplified post-pandemic. The reconfiguration and utilisation of space have become ever more important as the need to meet growing patient demand and staff satisfaction is dire.
The elephant in the room: backlog
The healthcare estate is ageing and plans for new facilities are drawn as the backlog of maintenance issues grows. The latest figures for 2021/22 show that while the cost of lowrisk maintenance in the NHS has fallen by 23 per cent (to £1.2 billion) since 2004, the cost of high-risk has risen by 256 per cent, to £1.8 billion. Urgent repairs and replacements are required in the healthcare estate to prevent disruption in the service provision and avoid significant risk of damage or harm. The collaborative sessions at this year’s National NHS Estates Conference will address capital funding challenges and the best resources available to renovate and repurpose old and dilapidated buildings. We will also look at the prioritisation of the effective use and maintenance of IT systems in the NHS to reduce delays in patient care and uphold interoperability standards.
Professor Kiran Patel, chief medical officer at University Hospital Coventry and Warwickshire NHS Trust explains how: “There is clearly a challenge when it comes to clearing the elective care backlog across the NHS and of course, across the NHS organisations are doing their best to manage elective demand and deliver care. Additionally, there is a need to ensure health inequalities do not widen as we restore services and restore services inclusively. At UHCW we have developed a way of restoring services inclusively and furthermore, developed a capability to go a step further to see if we can prioritise care for those who are deprived of access to employment opportunities, education etc. Whilst this is possible, public and citizen engagement is important to see if applying social value judgments are aligned to public expectation. Pressures on elective recovery are perhaps an opportunity to consider how we generate intersectionality with strategies such as health inequality.”
Case studies from healthcare facilities at the forefront of innovation will unpack smart solutions using data generated by IoT-enabled equipment to allow performanceenhancing, energy-saving decision-making. Methods of reconfiguring hospital buildings in a fundamentally different way to increase resilience against climate change and reduce carbon emissions will also be addressed with reference to the benefits of the NHS Energy Efficiency Fund.
Energy, energy, energy
The energy trilemma as defined by the World Energy Council is finding a balance between energy security, affordability and sustainability. The healthcare estate is one of the most affected industries. Even in the current energy crisis, the estate can’t just turn off the lights. The NHS also has high sustainability targets – being net-zero by 2040 – and Trusts across the country will be pushed towards cleaner and greener energy. On top of that, they will be expected to achieve targets within budgetary constraints.
So how can the healthcare estate navigate through this energy trilemma? Several projects are being rolled out across the country to combat the crisis. The NHS Property Services, which owns 10 per cent of the
Event Preview BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 22
healthcare estate, has recently published its Green Plan in hopes of helping achieve the sector’s net-zero targets. The Plan aims to create fit-for-purpose and sustainable spaces for delivering world-class patient care. The eight areas the Plan focuses on include: workforce and leadership, sustainable models of care, digital transformation, travel and transport, estates and facilities, supply chain and procurement, adaption and biodiversity and responsible landlord. Cameron Hawkins, head of energy and environment at NHS Property Services reiterates, “Becoming net zero carbon by 2040 is not just a nice-to-have but a must-have. The impacts of climate change are an increasing threat to the NHS estate. To counteract these, we need to continue investing in energy-efficient and naturebased solutions. So far, we’ve invested over £20 million in technologies such as LEDs and solar panels to lower energy bills and our carbon footprint. In doing so, we reduced carbon emissions by over 20 per cent and generated over £36 million in cost savings. Other NHS organisations and trusts around the country are also doing great work in reducing the impact of the NHS estate on the environment. Seeing all of us work towards the same goal, delivering a greener NHS for patients and the planet, brings me hope.”
Workforce for the future
The pandemic has emphasised the importance of all NHS staff and, alongside the clinical staff, the estates and facilities management workforce (EFM) rose to the challenge. The EFM workforce consists of approximately 100,000 people across England, representing 8 per cent of the entire NHS workforce. This small but important group of workers are the backbone of the NHS. As the NHS and wider community grapple with the lasting impact
of the pandemic, it is clear that not only the healthcare estate needs upgrading, but also the estates and facilities management team. In June 2022, the NHS launched the NHS Estates and Facilities Workforce Action Plan. The plan aims to look at how the EFM team can fulfil the ambitions of the overall NHS People Plan. The four key areas of work include: developing our people: this includes future-proofing skills so as infrastructure upgrades and new technologies are put in place, staff will be upskilled at the same time; building the next generation of estates and facilities management people: making the NHS the UK’s EFM employer of choice and working with the National Retention Programme to support people who might want to leave; embedding equality, diversity and inclusion: the EFM have work to do to increase the diversity in its team, currently, 50 per cent of women in the team are working in lower bands and only 20 per cent of women hold leadership positions. This is a stark difference from the wider NHS which has 74 per cent of the workforce made of women and 64 per cent of Band 7 and up roles held by women. There is a similar trend for ethnicity in the workforce; and improving the health and well-being of the staff: most EFM staff do not work in an office setting and often have shift work. The goal will be fostering a community within these varied workplaces and ensuring that everyone has access to services.
Looking to the future, the NHS Estates Conference on 19th April will bring together leading professionals and officials to build on this and plan the way forward for a more connected, fit-for-purpose and greener estate. Join us at etc venues St. Paul’s as we bring together estate, property and facilities management leaders from across the NHS and wider public sector for a day of collaboration and learning. Methods of innovating and redefining the NHS estate will be at the forefront of our progressive panel sessions, case studies and in-depth presentations driven by strategy and policy leaders. They will share the latest guidance on the design and planning of new healthcare buildings and improvements in facilities as well as share examples of how integrated care systems are establishing fit-for-purpose interoperability standards and providing enhanced care while improving cost savings. Complimentary passes are available for the NHS and the wider public sector. Your conference pass gives you access to 8 hours of CPD-certified content sessions, 2+ hours of dedicated networking time, lunch and refreshments throughout the day. Register your pass today by clicking below. L


FURTHER INFORMATION
https://hubs.la/Q01zbtsJ0
Event Preview Issue 23.1 | HEALTH BUSINESS MAGAZINE 23
























































Take A Look at Our Website Our customers save an average of IN PARTNERSHIP WITH 48% • Increased Fire Protection • Environmentally Friendly • No Annual Maintenance Charges • Lighter and Safer In ation proof for 10 years Environmentally Friendly • 20 Year Life Cycle • No Service Parts and Fewer Re lls • Watercourse Safe Biodegradable Foam • Low Energy Manufacturing • 100% Recyclable Extinguisher Increased Fire Protection fire@cherryproducts.co.uk 01608 678197 www.cherryproducts.co.uk CHERRY PRODUCTS New Generation Composite Extinguisher 34A Eastern Foam Extinguisher 3.4m 13A Standard Foam 1.3m Increased Fire Protection 1.5% Standard 13A Foam 98.5% Water 11.5% High Performance 34A Foam 88.5% Water - Kevlar Aramid Type Woven Core for Super Strength - UV Protective Casing - 15% Lighter Than Steel - Marine Grade Anti-Corrosive Components - 10 Year Guarantee Composite Construction BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 24
Losing your patients?
Dr Colette Jeffrey Associate Professor of Wayfinding at Birmingham City University on why hospital wayfinding is so difficult
Successfully finding your way in an unfamiliar hospital is challenging for most people even with clear wayfinding signs. Giving consistent, legible information that uses simple language and standard symbols is important, but your patients and visitors may still lose their way. Our ability to process information on signs and make wayfinding decisions is affected by anxiety, worry and pain. People who are stressed will struggle to remember medical destination names and complicated spoken directions. So what can hospitals do to make wayfinding systems simpler?
Wayfinding strategy

Firstly, a hospital needs to understand the wayfinding problems at their site, then

a single main corridor can cause confusion when patients don’t realise they need to use a specific lift to get to another floor and they use the wrong lift and get lost. Hospitals built on a hill will always have issues naming entrances and levels as people expect to enter the hospital on Ground Level in the UK, or Level 1 in other countries, so when going to a department on Level 2, they are likely to enter the building and look for a lift and go up two floors. Having very prominent sign saying ‘You are on Level Y’ at every entrance point and on every floor is essential for hill-side hospitals. Some use Level A, B, C, D to avoid level numbering confusion, others use generic theme names such as Forest Level and Sky Level. But are level
letters and names still problematic, especially at a site that also uses letters and names for zones, or buildings or wards?

Simplification
Most large hospitals have too many facilities, departments, wards and buildings to list on one sign or map, so site simplification is critical to avoid creating enormous signs that are not easily updated and are visually overwhelming. Finding ways to enable grouping of wayfinding information into smaller ‘chunks’ creating a hierarchy of information that is easier to scan through is challenging, but an important stage in developing your wayfinding strategy. There are many ways to simplify a site and no single approach is appropriate for all hospitals. Simplification enables patients to create a ‘mental map’ or simple image of the site layout and for designers to create simpler maps and signs that are as simple as possible and therefore easier for everyone to understand. In a 1960 study published as Image of the City, Kevin Lynch first introduced the concept of ‘way-finding’ and identified five elements that affect people’s ability to create an image of a place such as a hospital. These are nodes, districts, landmarks, paths and edges. “A legible city [or hospital] would be one whose districts or landmarks or pathways are easily identifiable and are easily grouped E
Outpatients
Feature Heading
Signage
Written by Dr Colette Jeffrey Associate Professor of Wayfinding at Birmingham City University
Our ability to signsinformationprocesson and make wayfinding decisions is affected by anxiety, worry and pain
A&E Department
Issue 23.1 | HEALTH BUSINESS MAGAZINE 25







“My storage solutions were sorted after booking my FREE consultation with the Business Services Team” Warehouse Manager Rob Thomson 0330 332 6312 WWW.BiGDUG.CO.UK BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 26
into an overall pattern” Thirty years later, in Wayfinding: People, Signs and Architecture, architect Romedi Passini and graphic designer Paul Arthur identify four more complicated, but useful types of circulation system patterns a hospital could use to make a place wayfindingfriendly – shoestring pattern, gestalt pattern, systematized pattern and network or repetitive pattern, believing “it is the combination of too many decision points and not enough information that gets people lost.”
Models
More recently in The Wayfinding Handbook, David Gibson identifies four models for organising a hospital signage scheme (see image below). The Connector model is where a connecting corridor links together other routes and is used at Queen’s Medical Centre and Nottingham City Hospital in Nottingham, UK. The Districts model is where the site is divided into geographical groups of buildings such as named wings and is also used at Queen’s Medical Centre. The Landmark model is where features, such as public lifts, are named or numbered to create landmarks for wayfinding and is used at St Thomas’ Hospital in London. The fourth model is the Street model where corridors are given street names making it easier to direct people, but also potentially causing confusion with external street names. Many sites use two of these models to create a simplification system that works.

Hospital changes
Hospital site layouts are constantly changing, with new buildings being added, old ones being demolished, entrances moving and
departments relocating. Having a wayfinding strategy that considers future changes and simplifies the site in some way will make it easier for people to overcome these inevitable changes. An effective wayfinding system considers three interconnected factors –people, information, and the environment. If your information is well-designed and consistent, and people giving spoken directions use the same names that are on the signs, patients will find wayfinding easier. If reception staff have been trained to give clear directions, using simple language and the same terms that appear on the signs, patients are likely to find their way. If you have distinct, recognisable landmarks along main routes and at key decision points that direction-givers can refer to, patients may remember it on their return journey.
Time saving and safety
Can you reduce the amount of time your staff spend helping lost patients find places by improving your wayfinding system? Are people missing appointments at your site and arriving late or so anxious that their
test results are affected? Getting lost usually results in a negative patient experience but has even been fatal. In 2018, a new mother got lost in a UK hospital trying to find her way back to the maternity ward from the special care baby unit. She mistakenly entered a dis-used staff area where she collapsed and remained unfound for seven hours and tragically she died from a brain haemorrhage two days after being found. A similar tragedy occurred in a shopping centre in Australia in 2017 when a man aged 71 mistakenly entered a fire stairwell and was not found until three weeks later, by which time he had sadly died. In both these cases, getting lost was not the main cause of death, but had they not got lost, they may both still be alive. Understanding how different people find their way, and how a patients’ cognitive state affects their wayfinding decision making is important for all hospitals to develop an effective wayfinding strategy will help make it easier for people to avoid getting lost in your hospital.
Research
In Design That Cares, Jane Carpman and Myron Grant state that “wayfinding involves five deceptively simple factors: knowing where you are, knowing your destination, knowing and following the best route to your destination, recognising your destination upon arrival and finding your way back out”. In Wayshowing, Per Mollerup agrees, believing that “wayfinding is a spatial problem-solving process” and he identifies three different activities “search, decision and motion – to seek, to decide and to move”. Mollerup also introduces the concept of ‘wayshowing’ where “wayfinding and wayshowing relate to each other as do writing and reading... or cooking and eating. One activity deals with sending, the other with receiving. The purpose of wayshowing is to facilitate wayfinding.”
The author of this article co-wrote the official NHS Wayfinding: Guidance for Healthcare Facilities in 1999 and hopes to be commissioned to produce a revised version, with digital wayfinding ideas. It is out-of-print but can be downloaded for free from here.
Technology
Through our research we found that “many factors affect how people orientated themselves and find their way, but wayfinding is essentially a series of inter-related decisions influenced by personal and environmental factors and also by the availability and understandability of information”. The theory seems relatively straightforward and consistent, but we found E
Signage
Most large hospitals have too many facilities, departments, wards and buildings to list on one sign or map, so site simplification is critical to avoid creating enormous signs that are not easily updated and are visually overwhelming
Issue 23.1 | HEALTH BUSINESS MAGAZINE 27
Illustration drawn by Colette Jeffrey




INTRODUCING
safety curtain track NEW reduced-ligature Curtain separates from gliders under excess load Easy to re-attach the curtain Gliders are fixed to the track Fits flush to wall The K2500 is supplied with two types of gliders, which enable three different release weights, 10kg, 15kg and 20kg. For more information on this new reduced-ligature track, to receive a sample or demonstration contact Grant on 01268 570900 or email enquiries@yewdale.co.uk K2500 safety curtain track Release Weight - 10kg Release Weight - 15kg Release Weight - 20kg
K2500
the reality of solving wayfinding problems in complex, ever-changing hospitals, with many different users, was not a simple task. Over a period of twenty years, Colette’s design teams have audited more than thirty UK hospitals, developed wayfinding strategies and designed information based on the NHS Estates guidance.
How people find their way to a hospital appointment has changed over the last ten years. People with disabilities plan their journey in detail so the content and accessibility of a hospital’s wayfinding information is important.
In 2009, 28 per cent of car users in the UK had a Satellite Navigation device (SatNav), and with the number of in-car SatNavs fitted as standard, this figure has increased significantly. A hospital’s postcode was rarely used for wayfinding ten years ago but now hospitals need to provide their full address, including a postcode for people to enter into their SatNav. They also need to check online mapping such as Google Maps shows the site in the right place when the postcode is entered.
Many companies in the UK offer touch screen technology used for wayfinding and hospitals that have been audited recently have screens in patient areas, but they are more often used for surveys and information messages, rather than offering interactive mapping and site directories. The future for cost-effective interactive information for hospitals is most likely to utilise mobile phones, with specific wayfinding information sent direct to a
Whose job is it to make sure signs and maps are kept up to date when departments are relocated, merged, renamed or closed down?
phone at each stage of the journey, giving relevant information as the user needs it, using global positioning technology to tell users where they are and where they need to go, creating routes shown on the phone screen, supported by audio information.
Communication
Communication is the key. A hospital wayfinding system should use consistent terminology at every stage of the user’s journey and should be kept up-to-date.
Achieving these two key goals requires clear and regular communication between different departments – the estates and facilities team, management teams, the capital projects team, strategy planners and most importantly the staff who deal directly with patients on a day-to-day basis. Hospitals in the UK are large, multi-disciplinary organisations, located in multiple buildings and operating across different sites. They are managed by even larger NHS Trusts and funded by the government. Whose job is it to make sure signs and maps are kept up to date when departments are relocated, merged, renamed or closed down? Often wayfinding strategies are given to the estates department to try to implement. At a
large UK hospital, a new privately financed (PFI) building for main outpatients had been erected and occupied but the estates manager had never been inside and he had not been allocated funding to update internal or external signs in the rest of the site to show the routes to the new building. L

About the author
Dr Colette Jeffrey is Associate Professor of Wayfinding and Inclusive Design in the School of Visual Communication at Birmingham City University. She is currently advising Birmingham Children’s Hospital on their wayfinding system and writing a book to be published early 2024 on why people get lost in buildings based on her PhD study of indoor wayfinding and waylosing.
FURTHER INFORMATION
David Gibson (2009) The Wayfinding Handbook, Information Design for Public Spaces. Princeton Architectural Press.
Wayfinding: Guidance for healthcare facilities. London, UK, NHS Estates out of print. Available online here
Signage
Issue 23.1 | HEALTH BUSINESS MAGAZINE 29
Pioneering digitisation in radiology
Radiology services are becoming increasingly decentralised and personalised, offering a far more convenient pathway for diagnosis and treatment
A major enabling factor for this shift is sector-wide digital transformation, providing new technology and information systems that allow data consolidation and sharing between clinicians. These tools will make it easier for healthcare professionals to access the necessary information from any location and at any time, helping them to diagnose and treat their patients better and sooner.
However, the transition to digitisation within radiology brings with it many challenges, as picture archive and communication systems of each hospital and department may differ greatly. Therefore, compiling the data silos from different sites into one central location inevitably creates vastly disparate data sets that need to be standardised and integrated to form the overall picture of a patient’s health, and to guide their personalised care pathway. This slows down the diagnostic process, causing delays in the onset of treatment, as well as stress to both staff and patients.
Until recently, IT systems in radiology lagged behind other industries, and even other areas of healthcare. With hospitals under increasing pressure to care for more patients with a smaller budget, the burden of data handling is only set to continue, highlighting the need for a novel knowledgesharing platform to enable the rapid digital transformation of radiology services at scale.
Embracing technology to enhance patient care
An example of this type of digital radiology platform can be seen at the East Midlands Imaging Network (EMRAD), where the deployment of new digital solutions and a dedicated image insourcing model has significantly decreased turnaround times, alleviating staff workload and improving patient experience. EMRAD is a network of hospital radiology departments spanning 14 hospitals within eight NHS trusts, and serves a population of over five million people. The collaboration was launched in 2013 to create a cloud-based digital radiology system to share radiology images and data between connected hospitals, making them available to relevant clinicians from any site, at any time.
EMRAD chose GE Healthcare to implement a range of picture archiving and communications software platforms for radiology, including a set of digital solutions to cover its storage and sharing needs
across the different hospitals and trusts within the imaging network. Adopting this image-sharing system has set the national benchmark for a new collaboration model within the field of radiology in the NHS. The open-access approach to image sharing furthers EMRAD’s goals of achieving the highest standards of clinical care for patients, delivering short reporting times on images, alleviating staff workload, and optimising the use of strained NHS funding and resources.
Recognising success with insourcing
The EMRAD insourcing program has provided additional financial support to radiologists and radiographers reporting images outside of their core hours, which proved crucial in successfully shifting the backlog accumulated during the COVID-19 pandemic. Image insourcing began in August 2016, with six insourcing reporters sharing images in real time across the EMRAD network. This number has since grown dramatically, and the network now has 131 reporters, including 100 radiologists and 31 reporting radiographers across seven NHS trusts. Through this team, EMRAD has insourced over 440,000 studies to date – spanning plain film, MRI and CT scans – and averaged 9,400 studies every month throughout 2022. This has so far saved the NHS over £3.3M by reducing its dependence on external third-party service providers*.
Accelerating change in community healthcare

The GE Edison™ Accelerator programme is an initiative launched in 2021 that brings together start-ups, healthcare providers, leading technology suppliers, developers and academic institutions under a single connected ecosystem, with the ultimate goal of providing validated solutions to enhance patient outcomes and staff satisfaction. The programme acts as EMRAD’s validation partner and enables it to develop valuable plug-and-play AI tools that will soon form part of an anticipated
full-blown machine learning system.
The network is also investigating solutions to staffing and recruitment issues in radiology, how to procure services more cost-effectively for the NHS, and possibilities for harnessing the power of AI in diagnostics. These advances aim to improve the quality and safety of patient services, and help ensure long-term sustainability and staff retention in radiology. Reflections on the journey to digitisation A cornerstone of EMRAD’s success over the past decade has been its high level of transparency and openness, both within and between its hospitals and NHS trusts. This has helped the participants build mutual trust and strong working relationships, forming the backbone of the system’s longevity and functionality. Since its inception almost 10 years ago, this has resulted in an altruistic and cooperative approach across the entire collaborative, with knowledge and resources being shared equitably to improve patient care. The 14 hospitals and eight trusts now work together with a strategic focus to explore new technologies and workflows for standardising radiology protocols, better supporting the burnt-out NHS workforce and enhancing patient experience and outcomes. EMRAD is committed to continuous improvement and learning, and supports ongoing professional development in the imaging field, maintaining the network’s forward-thinking focus and future-proofing radiology services across the East Midlands.
*The numbers provided in this study are generated and maintained by EMRAD as part of an ongoing economic analysis on the insourcing program, and are specific to the 8 NHS trusts and 14 hospitals that form the EMRAD network.
Advertisement Feature
L
FURTHER INFORMATION https://www.gehealthcare.co.uk/ campaigns/cdc
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 30
Achieving cleaner air



In December, Chief Medical Officer Professor Chris Whitty, published his annual report, this time on air pollution
Outdoor air pollution poses significant threats to health including heart disease, stroke, lung disease, cancer and asthma exacerbation. It is known to lead to increased mortality and is also linked to impacts on lung development in children.
The report acknowledges the problems posed by indoor air pollution as well.

Chief Medical Officer Professor (CMO) Chris Whitty said: “Everyone is affected by air pollution, and it is everyone’s problem.
“Air pollution has improved and will continue improving provided we are active in tackling it. We can and should go further – and it is technically possible to do so.”
Health problems
Some of the health problems associated with air pollution that are highlighted by the report include a low birth weight and asthma across every age group. In children, the problems include slower development of lung function, development problems, more wheezing and coughs and the start of atherosclerosis. In adults, problems may be coronary heart disease, stroke, lung cancer, chronic obstructive pulmonary disease and diabetes. In the elderly, problems include accelerated decline in lung function, lung cancer, diabetes, dementia, heart attack, heart failure and stroke.
Dr Charmaine Griffiths, chief executive of the British Heart Foundation, said: “We’re pleased to see the CMO focusing on air pollution
in his annual report this year. Research the British Heart Foundation has funded has helped to show just how damaging air pollution can be to our cardiovascular health.
“We have the tools and understanding to make better air quality a reality, but we need to do more. Making sure this report’s recommendations are implemented will help to clean up the air in all our communities and deliver real improvements to the nation’s health.”

It is estimated that the mortality burden of air pollution in England is between 26,000 and 38,000 a year. It has also been noted that improved air quality is associated with improved health outcomes – reductions in air pollution in London have led to reduced hospital admissions for asthma.
Sarah Woolnough, chief executive of Asthma + Lung UK said: “This report by the CMO
pollution. From our very first breath, air pollution has a significant impact on our health. Toxic air not only puts people at risk of potentially life-threatening asthma attacks and dangerous COPD flare-ups, it can also lead to the development of lung conditions including lung cancer.
“Chris Whitty is right to highlight the devastating impacts of air pollution and it is now vital that meaningful steps are taken to protect public health from this invisible threat. This includes schemes that work to get the most polluting vehicles off our roads.”
Achievements
The report highlights the improvements made to air pollution and also sets out solutions to continue the progress. The report points out that individuals have little control over the level of pollution that they breathe and that it needs to be seen as a societal problem to solve.
Since the 1980s, outdoor air quality has improved significantly, with air pollutants such as sulphur dioxide from coal and lead from petrol at fractions of their previous levels. Emissions of most outdoor air pollutants have declined steadily, though some, such as ammonia have been static.
Whitty’s recommendations for outdoor air pollution include: accelerating the electrification of light vehicles and public transport; innovation to reduce air pollution from nonexhaust sources such as tyres, and the need for a greater range of options for reducing air pollution from heavy and specialised vehicles; local urban planning supporting reducing air pollution locally – such as reducing air pollution near schools and healthcare settings; and in agriculture, reducing ammonia air pollution emissions through modified farming practices, such as applying slurry directly to soil.
Transport
Road vehicles are a main source of air pollutants, including PM2.5 and NO2, and the problem is worse in urban areas where there is large population exposure.
Road vehicle emissions have significantly reduced in line with regulations. It is anticipated that emissions from petrol E
Clean Air
Issue 23.1 | HEALTH BUSINESS MAGAZINE 31
“We can and should go further –and it is possibletechnically to do so”
and diesel engines will continue to fall as electric vehicle use becomes more widespread. However, the report points out that this switch should be accelerated. It is also expected that PM2.5 emissions from brakes will continue to fall as regenerative braking becomes more prominent.
Rail transport already uses electrification as its main power source, and compared to fossil fuel combustion, this can lead to reduced air pollution emissions – this is important in urban areas and enclosed spaces such as train stations. The report points out that further electrification is the ideal, but there are other technical solutions that could improve air quality in the interim or permanently. These solutions include power by bi-mode, battery or hydrogen fuel cells.
Aviation and shipping also emit air pollution, especially around ports and airports, which can affect the local population and these industries are lagging behind road and rail when it comes to reducing
emissions. The report recommends further reducing the sulphur content of ship and aviation fuels and also using electric power and tugs when aircraft are on the ground.
Government action
The report points out that government action can have a significant impact on air pollution, with central and local government able to influence air quality through regulation and the use of cleaner vehicles for public transport.
Urban planning can have an effect on how people use different forms of transport and can also influence the concentration of pollutants in areas of high building density.
Active travel is an area highlighted in the report that could be improved, with walking, wheeling and cycling having fallen significantly since the 1950s. Reversing this decline would have health benefits outside of reductions in air pollution, with an increase in physical
activity. The report calls for improvements to infrastructure for active travel.
Industry
Several industries have reduced their emissions over recent decades, with a large improvement in sulphur dioxide emissions, due to a move away from coal and engineered solutions. Regulations have encouraged transition from processes that resulted in high air pollution emissions. The report points out that industries can still reduce their emissions.

Agriculture
The report highlights agriculture as a sector which could significantly reduce its contribution to air pollution, with ammonia pointed out as an important air pollutant. Ammonia emissions have changed very little over the last few decades, though the report points out it is possible to reduce ammonia by using a combination of liquid manure (slurry) covering and changing techniques to apply slurry to fields - moving from broadcast (splash plate) slurry spreading, where much of the NH3 ends up in the air, to more direct methods such as narrow band spreading, trailing shoe or injection significantly reduces emissions.
NHS
The report has a whole section dedicated to the NHS: “The health sector, and specifically the NHS, needs to contribute to the effort
Clean Air
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 32
Several industries have reduced their emissions over recent decades, with a large improvement in sulphur dioxide emissions, due to a move away from coal and engineered solutions
to improve outdoor air quality and is taking steps to do so.” The report mentions the large estate, workforce and fleet and recommends reducing the combustion of fossil fuels used to heat hospitals and other buildings, as well as electrification of the vehicle fleet.
Indoor air pollution
It is estimated that people spend around 80 per cent of their time indoors, though not as much is known about the sources of and people’s exposure to indoor air pollution. Some pollutants may enter the building from outside, though there are indoor sources as well. Volatile organic compounds and carbon monoxide are emitted indoors and tend to have higher concentrations indoors as well. The report recommends reducing emissions and concentrations of known pollutants and identifying other chemical indoor pollutants with significant health harms.
For indoor air pollution, the recommendations include addressing a major engineering challenge – ensuring effective ventilation while minimising energy use and heat loss and increased research into tackling indoor air pollution including finding ways to reduce sources of indoor air pollution.

The report points out the role of ventilation as central to reducing indoor air pollution. There is an engineering challenge around maximising ventilation, but at the same time keeping buildings warm in winter
and cool in summer and therefore minimising energy and carbon use.
Research
The report highlights the need for research and innovation. While knowledge of the sources, impact and potential solutions for some air pollutants already exists, there are some research gaps.
The report identifies gaps in understanding how certain pollutants are generated, transformed and interact with the human body, and in designing countermeasures and mitigations – this includes the health effects of different components of PM, a better understanding of indoor air pollution, and economic analyses of air pollution interventions. Further development is also needed in counter measures including tyre design and research on energy-efficient and heat-retaining building ventilation.
Dr Sarah Clarke, president of the Royal College of Physicians (RCP), said:
“Air pollution is a growing and significant public health challenge and we strongly welcome the Chief Medical Officer making this the focus of his annual report for 2022.
“The RCP has been highlighting the harmful impacts of air pollution on ealth since 2016, when we published our report Every Breath We Take with the Royal College of Paediatrics and Child Health. We estimated then that around 40,000 deaths were attributable to outdoor air pollution, and since then a coroner found it to be a cause of death for the first time, that of 9-year-old Ella Adoo Kissi Debrah.
“The CMO’s report is an important contribution that makes clear why we must be proactive and ambitious in our efforts to improve both outdoor and indoor air quality for everyone.” L
FURTHER INFORMATION
Read the report here
Clean Air
While knowledge of the sources, impact and potential solutions for some air pollutants already exists, there are some research gaps
Issue 23.1 | HEALTH BUSINESS MAGAZINE 33
Health and Safety Event set to reunite OSH community
The Health and Safety Event is the UK’s premier event dedicated to improving occupational health and safety standards, opening its doors on 25-27 April 2023 at the NEC in Birmingham
Health and safety professionals will be able to network in-person with their peers, share best practice and explore the latest innovations and trends in the sector. Hosting over 250+ exhibitors, there is no event on this scale where delegates can meet directly with experts to compare thousands of the latest products and solutions for their health and safety management.
As part of the Safety & Security Event Series; the event is uniquely co-located with The Fire Safety Event, The Security Event, Professional Officer Security Live, The Workplace Event and National Cyber Security Show. With one registration, delegates will have free access to all these industry-leading events. Covering the entire buying chain of the safety and security of people, places and assets; its comprehensive offering
will save delegates time and money by travelling to this all-encompassing event.
Industry-leading exhibitors
At The Health & Safety Event, you will find 10,000+ products and solutions for your health and safety management in the workplace. Hosting all the major players from the industry including MSA safety, Dräger, Barbour, JSP limited, Polyco Healthcare, Portwest, PUWER Machinery Guarding, UVEX and many more - delegates will be able to speak to the experts directly to solve their health and safety challenges and discuss all upcoming projects.

Brand new to The Health & Safety Event, Start-Up Street is a dedicated area for startups to exhibit, that are less than 5 years old. They will be showcasing their cutting-edge
products and solutions that are shaping the future of risk management and saving lives.
Products and solutions
Over 10,000 products and solutions will be showcased at the show including Asbestos Control, Respiratory Prevention, Driver Safety, Drug & Alcohol Testing, Emergency/ First Aid Equipment, Environmental/Waste Management, Fall Arrest & Prevention, Hazardous Material Handling, Legal Advice, Manual Handling Equipment, Material Handling, Noise Control, Working at Height, Occupational Hygiene, Occupational Health & Wellbeing, Personal Protective Equipment, Plant/Machinery Safety, Risk Assessment/ Management, Safety Software, Slip & Trip Prevention, Training & Qualifications, Warehouse Safety, Workplace Cleaning, Workplace Ergonomics and Lone Worker. This is a brilliant opportunity to discover what is new on the market and condense months of research in finding new suppliers across 3 days.
Backed by the industry
IOSH, Health & Safety Executive, BOHS, BSIF, BOHS, UKATA, Highway England, SAFed, UK Safety Group and many more industry bodies and associations have confirmed their attendance at the show and will be onsite. Providing an unmissable opportunity to speak directly to the industry experts, the knowledge sharing and insight on offer will be invaluable to thousands of organisations to ensure they are up to date with industry standards and best practice..
Networking opportunities
Visitors come from every level of the buying chain and are from a diverse range of industries. Some of the confirmed visitors include: The Science Museum Group, Shell Energy, Siemens, Suez, Live Nation, NHS, Puregym, DHL, HomeServe, Dyson, Carlsberg, Bristol Water, ABB, Abbott Diabetes Care and more. To meet the business needs of health and safety professionals, CONNECT+ Live will return for another fantastic year of specialised networking. Matching the visitor’s buying requirements and needs with carefully curated exhibitors, the CONNECT+ Live team of matchmaking experts will fast-track access to key suppliers. Visitors can save valuable time and effort by making invaluable contacts through this outstanding and everpopular hosted meeting programme.
Back by popular demand, two networking reception drinks from 4:00pm on days 1 and 2 will take place across all the shows. Taking
The Health & Safety Event
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 34
place at the Networking Café, this is the perfect opportunity to unwind and meet industry peers and professionals, enjoy a drink with friends and colleagues, and make those vital new connections in an informal and affable setting.

Specialist features and zones
This year, The Health & Safety Event will have specialist features and zones to maximise your time onsite, with a number of exciting features, including the Registered Safety Supplier Trail in partnership with The British Safety Industry Federation (BSIF). All suppliers of this trail are members of BSIF and have signed a binding declaration that the safety equipment and services they offer meet the appropriate standards, fully comply with the PPE regulations and are appropriately marked. Follow the trail and be assured that the PPE you are buying is from a Registered Safety Supplier.
In partnership with the Highways England Driving for Better Business campaign, there will also be a dedicated feature Driver Safety Zone. This will share vital information and resources with safety professionals who have responsibility for work-related road risk. Driving for work is one of the most dangerous activities that employees ever undertake and government statistics show there are around 40,000 injury collisions every year involving someone who was driving for work at the time. Visitors will be able to speak to the experts and suppliers who provide specialist road risk management.
The new Machinery Safety Zone, which is sponsored by PUWER Machinery Guarding, will also showcase industrial machine safety products and solutions and host live demonstrations and workshops. Visitors will be able to upskill and educate businesses on how to ensure their machinery complies with the requirements imposed by the Provision and Use of Work Equipment Regulations (PUWER 98).
CPD-accredited content
The Health & Safety Event will boast CPDaccredited content across five theatres across the three days. The Knowledge Exchange sponsored by RS Components will return and will cover a series of panel discussions and presentations on challenges faced by health and safety professionals and
practitioners. Key speakers include Steve Perkins, managing director who will be speaking on workplace health culture and respiratory exposure, Bruce Durham, director - human resource from Huddle Culture on behaviour safety and BSIF’s own CEO, Alan Murray will be sharing his knowledge.
A show first and exclusive, IOSH will be hosting their dedicated conference on the first two days of the show at the Keynote theatre. Day 1 is focused on tomorrow’s OSH practitioner. Health and safety professionals have a vital part to play in creating resilient organisations. Their function is evolving from providing a technical support function to an enabling role, helping business to thrive and maintain productivity in an uncertain, fastchanging world. Their importance is growing as investors, supply chains and the public insist on more accountability from businesses for their impacts on people and places. IOSH, the world’s leading chartered professional body for people responsible for safety and health in the workplace, hosts sessions examining the broadening professional agenda, from OSH as a human right to managing mental health and wellbeing.
On Day 2, IOSH focuses on the professional journey. Anyone choosing a career in safety and health has more reasons than those
in other disciplines to want to be the best professional they can. The wish to do a good job for their employers and to achieve their full potential is boosted by the imperative to protect others from harm. IOSH’s sessions in the Keynote Theatre will give practitioners food for thought on how to achieve all three aims, whether it is maximising their impact in organisations or raising their professional standing. As the business landscape changes, experts will consider the place of professional ethics in OSH management and the value of increasing workforce diversity and helping develop others.
Another show exclusive includes The Health & Safety Executive’s conference on day three, who will cover pressing topics such as mental health, musculoskeletal disorders, risk assessments and more.

Brand new to The Health & Safety Event, the Practice Safety Theatre sponsored by MSA Safety will feature a panel of esteemed speakers sharing their knowledge and practical knowhow and tools on how to protect yourself and employees from danger. Visitors will be able to gain the practical tools and knowledge to protect themselves and their employees from danger, whilst helping to look after the future of their business or organisation. Register in advance for free entry to all industry-leading events.
Free to attend and based in Hall 3, health and safety event visitors will be able to access The Fire Safety Event, The Workplace Event, The Security Event, Professional Security Officer Live and National Cyber Security Show. Covering over 33,000 sqm at the NEC Birmingham, the series of events is guaranteed to maximise your time and investment in improving your business operations in all things security, fire safety, health and safety, and workplace/facilities management. L
Parking at the NEC for show visitors is free. Register in advance for free entry to all industryleading events with a single pass below.
FURTHER INFORMATION
www.healthandsafetyevent.com
The Health & Safety Event
Issue 23.1 | HEALTH BUSINESS MAGAZINE 35




www.powell-systems.co.uk/services | 0044 (0) 1689 879000 EMAIL US HERE Sustainability is a team pursuit - that’s why we work with you, not just for you WE ARE PART OF THE NHS HARD FACILITIES FRAMEWORK
Pioneering sustainable health centre opens to patients in Wiltshire
December 2022 marked the opening of Devizes Health Centre in Wiltshire to patients. But what makes this site so special? And how is it helping to tackle climate change? James Wakeham, principal construction manager at NHS Property Services (NHSPS), explains
Climate change affects not only the environment, but also our health. It can exacerbate conditions like cardiovascular disease, asthma, and cancer, which contribute to further issues such as health inequalities. By tackling climate change, we can concurrently reduce the burden of disease from factors like air pollution.



Role of the NHS
The health service has a particularly large role to play in tackling this. The NHS is responsible for 5 per cent of the UK’s total carbon emissions across all its activities. The NHS estate and its supporting facilities services comprise 15 per cent of the Health

of A+, utilising the latest green technology, including heat pumps and solar panels that generate heat and electricity, to enable self-sufficiency. This is a significant marker that demonstrates the site’s potential to run as a net zero health centre. In addition to this, Devizes has achieved a BREEAM (Building Research Establishment Environmental Assessment Method) rating of excellence, showing the high green building credentials that set a
3,000 NHS properties across England, from GP practices to hospitals, which see close to six million patients daily. We strive to be at the forefront of sustainable real estate, creating an NHS that is fit for the future and one that supports greener and healthier communities. The building of the new integrated care centre in Devizes, which meets the needs of the local community, had been a topic of conversation among the local community for some time. After many years of deliberation, plans for the new build were approved during the first half of 2021, with construction
Feature Heading
Energy
Written by James Wakeham, principal construction manager at NHSPS
Issue 23.1 | HEALTH BUSINESS MAGAZINE 37
siteThe has an EPC rating of A+, utilising the latest green includingtechnology, heat pumps and solar panels that generate heat











Read our whitepaper on how Powerstar supports NHS Trusts and healthcare providers to balance their energy priorities.
Benefits
The Devizes Health Centre provides many benefits to the NHS because of the way the building functions. For example, the building’s reliance on renewable energy sources provides a certainty of energy supply that can withstand market and supply changes. The provision of renewables ensures not only ensures a constant supply, but it also enables us to better manage budgets, which is especially important during periods of economic uncertainty when energy prices are rising at a dangerous rate. The centre has given much-needed additional space for health services in the area, making it easier for patients to access the care they need locally and all under one roof. A number of local health and care providers share the building and provide a range of services that you would find at a GP practice, as well as hospital outpatients and mental health services, creating a hub where patients can get urgent primary care. This means a quicker and more efficient service for patients, which all supports in tackling the NHS’ backlog of care.
Services
Patients of four local GP surgeries are now able to access same-day or next-day medical care and will be directed to the centre for routine blood tests and medical reviews for conditions like asthma and diabetes, as well as some specialist clinics. The services currently provided by Wiltshire Health and Care at the Devizes Community Hospital are moving to the new health centre. Royal United Hospitals Bath will be providing outpatient services including audiology, care of the elderly, paediatrics, rheumatology and urology services. The Avon and Wiltshire
Mental Health Partnership will be providing some of their community services from the new health centre. Supported by the Bath, North East Somerset, Swindon and Wiltshire Integrated Care Board, a wide range of organisations can now work together in a more joined-up and collaborative way in one of most state-of-the-art healthcare environments in the country.
Greener NHS
Devizes is just one of the many different projects that NHSPS is working on to improve patient care whilst delivering a greener NHS. Last year, we published our new Green Plan, part of our wider ‘Delivering a Greener NHS’ programme, which supports NHS England’s Greener NHS campaign.
My hope is that in the future, sustainable healthcare sites like this become the norm. Climate change has been widely recognised as one of the greatest threats to public health globally and nationally, and we at NHSPS are committed to reducing our environmental impact and promoting sustainable healthcare, enabling the NHS to deliver excellent patient care now and in the future. It has also been fantastic to work with the people of Devizes and our local NHS partners on this centre, to ensure the new site is fitfor-purpose and works best for them. L
FURTHER INFORMATION
Find out more on the Devizes Health Centre website here



Energy
EThe building’s reliance on renewable energy sources provides a certainty of energy supply that can withstand market and supply changes
Issue 23.1 | HEALTH BUSINESS MAGAZINE 39

We are helping to decarbonise Eastbourne District General Hospital
Veolia, the leading resource company supporting customers to achieve Ecological Transformation, has been awarded a £27m energy management contract to upgrade the 459-bed Eastbourne District General Hospital, part of East Sussex Healthcare NHS Trust
availability in the event of component failure. To ensure the heat is efficiently used, the project covers the fitting of insulated roofing, replacing older single glazed windows with high efficiency double glazing, and insulating cladding, along with insulated roofing which will be fitted as part of the contract.
How does it work?
The contract, which extends to 2040, includes a multi-million-pound construction project during 2023 that will deliver wide-ranging energy upgrades and target carbon savings of 4,129 tonnes per year. Delivered through Veolia’s “Building a Zero Carbon Future” programme, with funding provided through the Public Sector Decarbonisation Scheme for affordable, low-carbon energy efficiency upgrades across the public sector. The scheme is one of the first to take a whole building approach, which finds savings opportunities to reduce energy consumption. This utilises a holistic approach that accounts for how facilities and energy delivery systems interact while maintaining a comfortable indoor environment that enhances patient care.
How we have helped
Hospitals are the main energy users among government facilities which depend on energy to run their services, operate critical equipment and save lives. It’s a vital operation but also a demanding and expensive one. We are actively supporting the NHS decarbonisation programme and delivering lower cost energy for the healthcare sector, using wide-ranging energy upgrades. Our specialist energy team installed additional cladding and roof insulation, so the hospital will create a more comfortable environment for both patients and staff. Replacing the fossil fuel heating with lower carbon, electric dual stage heat pump system, and installing solar arrays gave a total of 1.1MWp renewable electricity, which is roughly equivalent to supplying enough electricity for 330 homes in the UK. The supply varies due to night-time, seasonal variation and gloomy winters. The weather also makes a big difference solar wise, for
example a 1.1MWe CHP running 24/7 would generate enough electricity for 2,900 homes. By targeting annual carbon savings of 4,129 tonnes, this project will make a significant contribution to achieving the trust’s decarbonisation goal of Net Zero, and will enable us to work together to deliver ecological transformation. Veolia has been working with East Sussex Healthcare NHS Trust since 2009, and currently provides energy and facilities management to over 100 hospitals in the UK.
Why is a secure energy supply important?
A secure energy supply is essential to maintain a modern patient care environment for the hospital which has 457 beds and treats more than 470,000 patients per year. With energy consumption in hospitals growing steadily, the access to reliable and clean energy is important to ensure the delivery of essential health care services for disease prevention and treatment. As the NHS is funded mainly through general tax payers’ money, funding is limited. To meet this energy demand and achieve carbon and energy cost savings, Veolia will manage projects covering the design, delivery, and installation of a range of energy upgrades. These will guarantee the hospital meets the NHS carbon reduction targets for 2030 and is supported by a 24/7 operations and maintenance contract.
What do the energy upgrades to the site include?
The energy plant upgrades include desteaming the site, solar arrays giving a total of 1.1MWp renewable electricity, improved ventilation systems, and a dual stage heat pump system to supply 3.2 MWth of low carbon heat with N+1 redundancy that gives system
Heat pumps work by extracting energy from the surrounding ground, air or water, and transferring it from one area to another. In a process similar to a refrigerator or air conditioning unit, extremely cold fluid circulates through tubes in the heat pump’s external network. This is then vaporised and compressed to generate heat.
How does this solution make a difference?
Heat pumps are an attractive option as part of a cost-effective energy mix. It is a fast and cost-effective way to decarbonise heat and reduce your carbon footprint, without increasing your energy bills. Although they do consume a large amount of electricity (one unit of electrical energy to produce three units of heat energy), by using renewable energy sources, heat pump systems can also become carbon neutral.
Value delivered for you
Our expert energy teams can design, install and operate a heat pump system on your site, taking care of the technology so you can concentrate on your core business activities. Not only can we integrate heat pumps into your existing heating infrastructure, we can also power them using innovative renewable electricity solutions, such as those powered by biogas. So you can achieve a zero carbon future, for less than you thought possible.
How can we help you?
Explore our Ecological Transformation solutions for healthcare visit: https:// www.veolia.co.uk/sectors/healthcare
Follow us on LinkedIn: VeoliaUK L

FURTHER INFORMATION www.veolia.co.uk
Advertisement Feature Issue 23.1 | HEALTH BUSINESS MAGAZINE 41




The zero-waste textile of the future We have the lowest verifiable carbon footprint in the world scrubs per day, a year for would recycle equating to The production of hospital standard PET bottles kilograms of general PET waste 1000 1 11M 203K 100% recycled and recyclable medical clothing made in the UK Order now and find out more at: www.upcycledmedical.com T: 0330 133 4192 E: info@upcycledmedical.com E
The Green Plan at Leeds Teaching Hospitals NHS Trust
The NHS is the first health service in the world to embed net zero into legislation, with a goal of reaching net zero by 2040. Here we look at the Green Plan of the Leeds Teaching Hospitals NHS Trust

Leeds Teaching Hospitals NHS Trust has a vision to be the best for specialist and integrated care and improve the health of patients through the provision of high-quality care. In order to provide the best quality care and improve quality of life for patients, the Trust recognises that it needs to reduce its impact on the environment.
Since Leeds City Council declared a climate emergency in 2019, organisations and individuals across the city have been working towards the goal of making Leeds a zero-carbon, nature-friendly and socially just place to live.
The Trust, which is one of the largest teaching hospital trusts in the UK, aims to become one of the greenest NHS hospital trusts in the UK and play a central role in reducing carbon emissions across the city.

The Trust said: “Reaching net zero is a key agenda at present, and the Trust has
incorporated sustainability measures into the day-to-day running of our hospitals for several years. We know that to reach our target of becoming net zero by 2040 we will have to make some tough decisions and introduce radical changes.
The key to our success will be our people and ensuring everyone understands the important role they can play both individually and within their CSUs.”
The Trust recognises the threat that climate change presents to the environment and the impacts that we are already seeing including increases in heatwaves, droughts, storms and floods. Of course, these changes also have an impact on population health, including areas such as heat-related mortality, infectious diseases and mental health, which
in turn have an impact on hospital services. The NHS has set two targets in an attempt to meet the goal of becoming the world’s first net-zero national health service, this means net zero for the emissions the NHS control directly (the NHS Carbon Footprint) by 2040 and net zero for the emissions they can influence (the NHS Carbon Footprint Plus) by 2045.
Achievements so far
Leeds Teaching Hospitals NHS Trust has 2013/14 as its baseline year and has already seen a 33 per cent reduction in its direct carbon footprint since then. In 2021/22, the Trust treated 1,321,593 patients (an increase of 23 per cent since 2013/14), but reduced the CO2e per patient by 45 per cent.
The Trust has already improved biodiversity by maintaining grass and wildflower areas and planting over 1,100 trees; introduced Attend Anywhere software for remote appointments; moved to a digital online patient record system and invested £20 million in energy saving projects.
They have reduced the carbon emissions of anaesthetic gas; won the Green Surgery Challenge for sustainable practice in E
Feature Heading
Net zero
“Reaching net zero is a key agenda at present, and the Trust has sustainabilityincorporated measures into the day-to-day running of our hospitals foryears”several
Issue 23.1 | HEALTH BUSINESS MAGAZINE 43
Bexley Wing, St James’s University Hospital
laparoscopic appendectomy; signed the NHS plastic reduction pledge; become the first Carbon Literate NHS Teaching Hospital Trust and reduced processed and red meat options.
The Trust has also refurbished the combined heat and power units, used leak detection software to reduce downtime and costs; upgraded shuttle buses to low and ultralow emission; consolidated deliveries to the Trust to a centralised site; and competed in the Green Ward competition to develop sustainable innovation in clinical areas.
Aims
The key elements of the Trust’s green plan are to ensure the Trust aligns with the wider NHS ambition to be the first healthcare system in the world to reach net zero carbon emissions; prioritise interventions that will enable the Trust to continue improving patient care whilst delivering carbon reductions and improving sustainability performance; and support increasing efficiency throughout the organisation.
“To deliver truly sustainable healthcare, we need to achieve environmental, social and economic sustainability, which link strongly to the Leeds Way Values.
“By recognising that climate change is a health emergency, we aim to be accountable for our environmental impact.
“We will create social value through sustainable, fair and patient centred decisions and take a holistic approach to sustainable and resilient models of care.
“We have taken a collaborative approach to improve sustainability within our organisation and the region. We will continue to engage with staff, our partner organisations and supply chain to empower people to deliver sustainable change.”
Actions
The Trust has a sustainability team with a dedicated head of sustainability and energy and waste managers tasked with progressing the sustainability agenda and holding the Trust accountable for taking action.
Mott MacDonald was commissioned to produce an Estates Decarbonisation Strategy, with a roadmap of initiatives designed to increase the number of connections to the Leeds Pipes district heating network and improve the fabric of the buildings, including windows, fascias, roofs and wall insulation. If the roadmap is followed, the Trust will reduce carbon emissions by 80 per cent by 2030 and by 92 per cent by 2040.
Between 2022 and 2025, several actions will be taken. This includes a transition to Leeds Pipes district heat network for St James’s University Hospital; the installation of air source heat pumps at Chapel Allerton Hospital; upgrades to lighting, glazing and building upgrades across the estate; and the inclusion of climate change in the Trust Risk Register. Over this period, all NHS procurements will include a minimum 10 per cent net zero and social value weighting and the trust will ensure that waste is managed and disposed of at the highest level of the waste hierarchy.
Between 2025 and 2032, there will be lighting, glazing and building fabric upgrades across the whole estate and a reduction in the operational emissions of the Hospitals of the Future (HoTF), with the aim of achieving BREEAM Excellent and Well Gold standards. There will be a large-scale roll-out of the electrification of heat initiatives and a review and upgrade of the electrical infrastructure capacity.
Between 2032 and 2040, there will be a major investment in energy centres, alongside the installation of heat pumps and a continued electrification of the Trust’s vehicle fleet.
On an ongoing basis, light fittings at the end of their life will be replaced with LEDs and glazing upgrades will continue. Climate change adaptation will be integrated into decision making and ventilation upgrades will be carried out, with the installation of heat recovery and energy efficiency interventions.
Sustainable action plan
The trust also has a sustainable action plan with interventions in workforce, leadership and partnerships; sustainable care models; medicines; estates and facilities; digital transformation; travel and transport; food
Net zero
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 44
Climate change adaptation will be integrated into decision making and ventilation upgrades will be carried out, with the installation of heat recovery and energy efficiency interventions
and nutrition; supply chain and procurement; biodiversity and climate change adaptation.
In the realm of workforce, leadership and partnerships, this means supporting and engaging staff to improve sustainability at work and home; ensuring sustainability is embedded within decision making and working with partner organisations to achieve sustainability goals, as well as with the local community.
Sustainable care models means being mindful of the environmental impact of the care provided, promoting walking for health, welfare support and remote consultations and working collaboratively to provide holistically sustainable care models, including providing care closer to home.
On the subject of medicines, action will be taken to reduce the carbon impact of inhalers, and reviews will be carried out on the impact of nitrous oxide within the Trust and on the current procedures for prescribing medication.
In estates and facilities, the environmental impact of the estate will be reduced to ensure it is fit for the future and provides high-quality healthcare services. Energy efficient technologies will be embedded and the Trust will continue to reduce clinical and non-clinical waste.
In terms of the digital transformation, the Trust will continue to support remote working for staff, embrace new technologies and provide accessible digital patient care and drive efficiency and minimise resource consumption from paper, printing and postage.
Travel and transport includes working with local organisations to improve public transport, reducing the number of vehicles commuting to the sites and increasing the use of sustainable and active travel, as well as increasing the provision of cycle storage and showers across the Trust.
From a food and nutrition point of view, healthy food options, from sustainable sources will be provided and a digital ordering system to enable meals to be easily adapted to patients’ needs and reduce over ordering will be used. Alternative disposal options for food and packaging waste will also be explored. Focussing on the supply chain and procurement, KPIs will be set for the carbon emissions of procurement and it will be ensured that staff are aware of sustainable procurement practices. Product lines will also be streamlined to reduce waste. In terms of biodiversity, KPIs will be established to increase biodiversity and the impact of the supply chain on global biodiversity will be assessed. Finally, a climate change adaptation plan will be developed and the potential impacts of climate change will be included in the Trust’s Risk Register. A climate change risk assessment will be developed and staff will be educated on the adaptation plan and its connection to the Green Plan and major incident plan.
Staff engagement
In order to deliver the Green Plan, the Trust recognises that everyone needs to play their part. GRASP (be Green, Recycle, be Aware, be Sustainable for our Patients) champions will be recruited to embed and share sustainable practices across the Trust. GRASP rewards encourage staff to take positive environmental actions, with green points awarded for actions they log and those with the most points winning a £20
voucher. More than 550 people are now taking part with 55 tonnes of CO2e saved. Chris Kelly, associate director for estates compliance and risk at Leeds Teaching Hospitals, said: “We now have a decarbonisation road map for each of our five hospital sites, which details the interventions and capital investment needed to decarbonise the Trust estate scope 1 and 2 emissions. The focus will be on reducing the use of harmful fossil fuels, improving energy efficiency and transitioning to low carbon energy sources. Works will include building fabric upgrades, LED lighting, integration of renewable technologies and expanding our connections to the local district heating network, Leeds Pipes.” Craige Richardson, executive director of estates and facilities, Leeds Teaching Hospitals, said: “The Trust recognises that if we are to provide the best possible care to our patients and improve their quality of life, we need to reduce our environmental impact. Working with industry experts such as Mott MacDonald demonstrates our commitment to making radical changes and being at the forefront of creating a greener NHS. We will continue to embed sustainability into all our core activities so that it can become an integral part of our culture.”
With such a detailed Green Plan, and a long list of actions already taken and planned, Leeds Teaching Hospitals NHS is well on track to delivering net zero targets. L

FURTHER INFORMATION
Find the Green Plan here
Net zero
Travel and transport includes working with local organisations to improve public transport, reducing the number of vehicles commuting to the sites and increasing the use of sustainable and active travel, as well as increasing the provision of cycle storage and showers across the Trust
EIssue 23.1 | HEALTH BUSINESS MAGAZINE 45
Leadership recruitment for the public and third sector
Anderson Quigley (AQ) are a specialist executive search, interim management and advisory consultancy, supporting organisations that focus on society and social development. We are driven by our core values - integrity, diversity and hands-on project ownership, using our decades of knowledge and expertise to deliver leadership recruitment in health and social care, education, charities, cultural organisations, the arts and government
Consulting on highly complex public and third sector leadership assignments, we continually present gender-balanced, diverse, high-quality shortlists in both executive and non-executive recruitment. We challenge our clients to take positive action to promote diverse appointments and to think more creatively on cross sector hires - ensuring candidates are seen for more than just their skillset. Our highly experienced team are dedicated to the advancement of social development with a real enthusiasm for their respective sectors. Above all, we are a responsible business, focused on individual and collective development. We ensure our people work in a respectful, diverse environment, where every effort is made to support continual learning. We always act responsibly towards our clients and candidates, guaranteeing them fair, honest, and objective advice.
These are the fundamentals of our culture. They are the foundation upon which our business continues to grow and thrive.
What makes Anderson Quigley different?
Sector Insight – having worked with many NHS Trusts, professional regulators, and National Health organisations, we have a strong understanding and perspective on the market. We are also able to work closely with clients to identify the key challenges and opportunities and hone those to establish a clear candidate proposition. Candidate Engagement – when managing senior level appointments, most candidates will have at least two to three conversations with a head-hunter. We understand the importance of this relationship and that we are acting as your ambassadors. Candidates look to us for an honest appraisal of their skills and experience. We want to present to you a strong list of candidates that absolutely have the credentials, experience, and values to make a lasting contribution to the role.
Partner-Led Model – established in 2017, Anderson Quigley is a purpose-led

organisation founded and driven by a core values set of diversity, integrity and hands-on project ownership. As such, each assignment will be partner-led, with a senior member of our team taking personal responsibility for the delivery of your campaign.
Diversity – AQ is committed to diversity and was created to support clients and candidates in the public services. With a deep belief in equality, diversity and fairness, these values are at the heart of our business. Our role is to seek out talent in all its forms, identify future talent and challenge assumptions –we do this by having an open mind about sources of talent and we see it as our duty to actively challenge assumptions about what outstanding talent looks like.
Small is Beautiful – agile, fleet of foot, AQ’s size is our strength. We have your best interests at heart and can freely and independently search for the right candidates and work in the best interests of your organisation to produce a quality, results-led process that will result in the presentation of an outstanding shortlist.
Track Record – since our inception, AQ have worked with a variety of different organisations on executive and non-executive appointments. These have included in the past twelve months alone: Northern Care Alliance NHS Foundation Trust, South Western Ambulance Service NHS Foundation Trust, Herefordshire & Worcestershire Integrated Care System, Queen Victoria Hospital NHS Foundation Trust, Birmingham Women’s & Children’s Hospital NHS Foundation Trust, Northamptonshire Healthcare NHS Foundation Trust, Care Dorset, Camphill Village Trust, General Dental Council,
Innovate HealthCare Services, and Coventry & Warwickshire Integrated Care Board.
Helene Usherwood, AQ Partner, Health & Social Care
With over 20 years’ headhunting experience, Helene has appointed to senior roles within the arts, health and education fields as well as central and local government. Joining Anderson Quigley in 2018, Helene has established and continues her work specialising in the appointment of executive and nonexecutive directors in the NHS covering acute, ambulance service, primary care, mental health and regulatory bodies as well as national organisations and Royal Colleges. In addition to her work with NHS Trusts, Helene has developed Anderson Quigley’s Board Practice, working across all sectors to appoint chairs and non-executive directors. She has developed excellent networks across the public and private sectors to encourage greater levels of diversity around the boardroom table. As well as providing bespoke services, advice and guidance to her clients and candidates, Helene is highly motivated to provide careers advice and guidance to individuals, especially to those who have not previously considered a non-executive opportunity before but whom have unique insights and skills to offer the role. L
FURTHER INFORMATION
www.andersonquigley.com
helene@andersonquigley.com
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 46
Advertisement Feature
Setting the standards for food and drink
NHS England published updated national standards for healthcare food and drink in November. HB investigates
The national standards for healthcare food and drink “describe the methods by which organisations must ensure the quality and sustainability of their food and drink provision for patients, staff and visitors, and how they should be applied and monitored, as well as recommending future improvement aspirations and actions.”
The foreword to the standards, by Simon Corben, director and head of profession at NHS Estates, NHS England begins: “Every healthcare organisation has a responsibility to provide the highest level of care possible for their patients, staff and visitors. This includes the quality, nutritional value and the sustainable aspects of the food and drink that is served, as well as the overall experience and environment in which it is eaten.
“It is important that all healthcare organisations see the intrinsic value in the view of ‘food as medicine’ and that it remains a standing item on the board agenda. Senior NHS leaders must be held accountable for the standard and quality of food served in their organisation, and patient and staff nutrition must be prioritised.”
Corben mentions variation across the country when it comes to food and drink for patients, staff and visitors. He states that not enough healthy options are consistently available, too much food is wasted and sustainability is not well embedded. He says that the Food Leadership team is aware that things need to improve and that the publication of these standards is part of that.
It is chief executives who are ultimately responsible for ensuring that patients, staff and visitors are able
to access healthy, nutritious and sustainable food. The guidelines aim to provide chief executives and their teams with the tools and information to be able to do this.
NHS England set up the Healthcare Food standards and Strategy Group to follow
and impact of the standards in order to support organisations to meet them.
The standards themselves build on previous hospital food standards, and consider the recommendations from the independent review of NHS hospital food. They also take into account NHS and government priorities and will be updated as necessary.
The standards are part of the NHS Long Term Plan and will also form part of the legally binding standards in the NHS Standard Contract. There are eight standards in total and NHS organisations are required to meet them. Each organisation must have a designated board director responsible for food and must also report on compliance with the standards at board level.
The standards are as follows:
One
“Organisations must have a designated board director responsible for food (nutrition and safety) and report on compliance with the healthcare food and drink standards at board level as a standing agenda item.”

Feature Heading
Catering
Issue 23.1 | HEALTH BUSINESS MAGAZINE 47
“It is important that all organisationshealthcare see the intrinsic value in the view of ‘food as medicine’”

Two
“Organisations must have a food and drink strategy.” This means that every trust must develop its own “live strategy” for improving nutrition and hydration for patients, staff and visitors.
Three
“Organisations must consider the level of input from a named food service dietitian to ensure choices are appropriate.” Each trust needs to assess how many posts are needed for their hospital. The posts will be responsible for overseeing patient, staff and visitor food and drink. The standards provide a dietitian job description and person specification to help with this.

Four
“Organisations must nominate a food safety specialist.” Trusts need to recognise that they have legal obligations as food business operators and therefore ensure effective compliance with robust food safety procedures at every level. Trusts are responsible for ensuring that their supply chain is safe. The standards expect that trusts have a named Responsible Person, Competent Person, Authorised Person with the Chief Executive Officer being notified for assurance. The standards include a food safety specialist job description to help organisations meet this standard.
Five
“Organisations must invest in a high calibre workforce, improved staffing and recognise the complex knowledge and skills required by chefs and food service teams in the provision of safe food and drink services.” In recognising the complexity of delivering healthcare food and drink services, trusts need to ensure appropriate levels of staff at all levels and remunerate staff accordingly. This standard is intended to support food safety, nutritional safety and patient safety and provide a better working environment and therefore contribute to staff wellbeing, morale and retention.
Six
“Organisations must be able to demonstrate that they have an established training matrix and a learning and development programme for all staff involved in healthcare food and drink services.” This standard aims to provide assurance that staff are appropriately trained and are practising safely. This also includes non-catering staff such as nurses and porters who also handle food.
Seven
“Organisations must monitor, manage and actively reduce their food waste from production waste, plate waste and unserved meals.” Trusts need to understand where food waste comes from and why and take steps to reduce this. They must also recognise that reducing food waste will support funding for better food services for patients, staff and visitors. Figures on food waste will need to be reported and these will be published. Lots of support is available for this standard,
including WRAP – food waste reduction roadmap toolkit and webinars on reducing food waste. This standard is intended to have a positive impact on staff behaviour and accountability and deliver cost reductions.
Eight
“NHS organisations must be able to demonstrate that they have suitable 24/7 food service provision, which is appropriate for their demographic.” This may include: retail solution; auto cafés; staff break areas;
The standards are comprehensive and detailed and aim to improve food and drink standards across the NHS, in terms of nutrition and sustainability. The standards provide a large amount of support and advice to help trusts and individuals ensure these standards are met. The standards should go a long way to making sure the food and drink provided at NHS sites is healthy and sustainable and have a positive impact on the health and wellbeing of patients, staff and
Catering
Issue 23.1 | HEALTH BUSINESS MAGAZINE 49
Trusts need to understand where food waste comes from and why and take steps to reduce this
Tackling hospital winter pressures
Helen Hunt, innovation programme manager (Workforce) at the West Midlands Academic Health Science Network explains how the NHS Insights Prioritisation Programme is helping to address winter pressures
According to the Royal College of Emergency Medicine, approximately 4,000 patients a day are currently experiencing waiting times of more than 12 hours in A&E. With the onset of cold weather and flu exacerbating these pressures, there has never been a more important time for us to reduce unavoidable hospital admissions.
What’s more, the cold weather and the illnesses it brings presents an increased risk to our elderly population. Hospital admissions of this nature contribute to the growing pressures on A&E departments.
To minimise these risks and reduce hospital admissions for the elderly population, the NHS Insights Prioritisation Programme (NIPP) is being implemented. The NIPP is designed to accelerate the evaluation and implementation of innovation that supports
post-pandemic ways of working, builds service resilience and delivers benefits to patients.
The West Midlands Academic Health Science Network (WMAHSN) has been working alongside ARC West Midlands, as well as Sandwell and West Birmingham Foundation Trust and South Warwickshire Foundation Trust, who have implemented new models of care for admission avoidance for older people living with frailty.


In this region, two models of care for admission and conveyance avoidance have been identified. The first, which is

the South Warwickshire model, utilises geriatrician outreach and enhanced rapid response community services. The second, known as the Epicentre model and used out of Sandwell and West Birmingham Hospital, relies more on point of care testing, such as hand-held ultrasound and blood testing. Helen Hunt, innovation programme manager (Workforce) at the WMAHSN, is supporting the rollout of this innovative programme.
Can admission be avoided for older people living with frailty? New models of care can work to ease the burden on hospitals and emergency services by addressing health inequalities and providing point of care testing in the home. This can be done through diagnostics and acute medical intervention, as well as enhanced support from community teams with input from secondary care.
population

Winter pressures
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 50
Through this, the programme is working to avoid the conveyance of older patients with frailty to hospitals, as emergency departments are not the most appropriate setting to deal with this.
Supporting hospitals and emergency services
Delivering high-quality and frailty-attuned acute assessment and ongoing care outside congested acute hospitals is a very high priority for the NHS. These two solutions are being evaluated as part of the NIPP.
The average hourly cost of an ambulance unit is £500, and the West Midlands Ambulance Service responds to around 4,000 calls daily. Through this work, we are working to reduce this strain on emergency services and save vital costs in the process: giving back time and money.


Supporting the elderly population
No elderly patient wants to be admitted to hospital for minor ailments, and the new models of care support them in their wishes. By providing essential medical support in their homes, we can enable greater independence whilst improving overall safety and enabling them to safely stay in their own comfortable surroundings. One reason elderly patients prefer to receive care at home is due to fears surrounding the length of hospital stay. As age increases, so does the length of stay in hospital; patients under 75 have an average length of stay of 3.4 days, while the average for patients aged 75 and over is 8.6 days. Knowing what our patients’ wishes are when it comes to receiving care is very important,
and we hope that, through evaluating the new models of care, we can evidence a new model that suits both patients and care providers.
How are the new models of care making a difference?
Dr Tom Knight, from Sandwell and West Birmingham NHS Trust, is involved in the Epicentre project, which focuses on Emergency Admission Avoidance Through Point of Care Testing.
The Epicentre model is based on acute medical registrars working in the community; patients are essentially admitted to hospital but in their own home, and are still allocated a consultant, just as they would in hospital. There are no specifications on age or frailty, and the project takes referrals from GPs, ambulance services and hospitals.
Recently, Tom used the Epicentre model to allow an elderly patient to receive treatment and end-of-life care in his own home. The 81-year-old male was referred to the service through his GP and the ambulance service with symptoms of coffee ground vomiting, several months of progressive dysphagia and significant weight loss. With a previous history of a duodenal ulcer, there were suspicions that the patient had a UGI bleed, but on further inspection, it was found that he had a gastric outlet obstruction. Tom could deduce that the problem was not treatable, and the patient made it
clear that he would not go into hospital, so he was transitioned onto a supportive care plan. Conversations were able to be had with the patient and his family about his wishes and where he wanted to be, and a plan was enacted to manage his symptoms and keep him at home. As a result, the patient was cared for at home until the end of his life, meeting his wishes and relieving pressures on the hospital that he would have otherwise been admitted to.
What do we hope to achieve?
Since the NIPP started in early 2022, we have seen some initial findings which indicate success. In one month, 102 conveyances were avoided at 50 per cent call rate, and 450 patients over the age of 75 were conveyed to South Warwickshire Foundation Trust instead of 552. We hope this success will continue, and the primary findings will be available in spring 2023, followed by the ARC West Midlands evaluation and subsequent implementation guides. Our ambition is to continue alleviating the extreme pressures that the NHS is under, especially at this time of year, and ensuring that patient safety and comfort are continuously prioritised and improved. L

FURTHER INFORMATION
https://wmahsn.org
Winter pressures Issue 23.1 | HEALTH BUSINESS MAGAZINE 51
Since the NIPP started in early 2022, we have seen some initial findings which indicate success



NHS Digital merges with NHS England
NHS Digital has now officially merged with NHS England; HB takes a look at what the NHS’s IT hub does
The legal merger of NHS Digital and NHS England is intended to be one step in the process of creating a new single organisation to lead the NHS. The merger means that the NHS’s data and technology expertise are brought into one organisation, which is anticipated to create a closer link between the collection and analysis of data and therefore drive improvement for patient outcomes. The transfer means NHS England will become the custodian of national health and social care datasets and the single executive non-departmental public body with responsibility for digital technology, data and health service delivery in the NHS.
Amanda Pritchard, chief executive of NHS England said: “Digital, data and technology already underpin so much of our personal and professional lives. Harnessing the enormous potential they hold will be key to supporting our continued management of and recovery

from the pandemic, delivering on our Long Term Plan, and making services better and more sustainable – crucially in ways that support staff to do their best work, and deliver more convenient services for patients.
“Our colleagues from NHS Digital bring a wealth of experience, knowledge and expertise, and a track record of delivering major data and digital projects and services, which will continue to be invaluable in our aim to help the NHS transform and improve the health and care of the people it serves.”
Health Education
England, the body responsible for the education and training of the health workforce, will also be incorporated into NHS England in April. According to NHS England: “The integration of NHS Digital, Health Education England and NHS England will put workforce, data, digital and technology at the heart of plans to transform the NHS, enabling better, more joined-up decision-making at system, regional and national levels, and a more effective and efficient use of collective resources.”
The merger is intended to create a single, streamlined organisation, building on the strengths and expertise of its legacy organisations and at the same time avoiding duplicate activities. It is anticipated that the new organisation will be 30 to 40 per cent smaller that the current combined size of NHS England, NHS Digital and Health Education England by the end of 2023/34. Almost all systems, processes and job roles are due to remain the same until at least April 2023.
The new organisation is planned to support and accelerate a move to greater partnership working through integrated care systems, by speaking with a single national voice and modelling effective joint working. It is hoped the merger will help NHS England work more efficiently.
Simon Bolton, interim CEO at NHS Digital, said:
“Our merger with NHS England creates the opportunity to put digital at the heart of the NHS and build on what we’ve already achieved at NHS Digital. E
Feature Heading
IT
Issue 23.1 | HEALTH BUSINESS MAGAZINE 53
NHS anddesigns,Digitaldevelops runs national IT and data services that support clinicians at work, provide care to patients and use data to improve treatment







LapCabby is the smart way to keep your devices safe, charged and secured Chromebooks Tablets Surface Pros Smartphones Charging and storage solutions for Chromebooks, Surface Pros, Tablets and Smartphones. Easy to clean units that enhance service delivery and patient care. Some of our clients: West Suffolk NHS Trust | UCL Institute of Neurology | Frimley Healthcare NHS Trust Luton and Dunstable Hospital |NHS Greater Glasgow and Clyde | Royal Manchester Children's Hospital Barnsley Hospital NHS Foundation Trust | Southend University Hospital NHS Fund For more information please contact Marvin Douglas | LapCabby UK Sales Manager 07890 478 403 | 0115 982 1771 | marvin.douglas@lapcabby.com www.lapcabby.com | sales@lapcabby.com Lyte 10 WD Surface Pro Lyte 10 SD Mini USB Lyte 20 SD MP USB DeskCabby Charge Only GO2 Mini 5-device USB charging basket for tablets and smartphones up to 13” 12-device desktop USB charging cabinet for any USB devices up to 12” 20-device USB charging cabinet for smartphones and other USB devices up to 7” 10-device static USB charging cabinet for tablets, mobile phones and other USB devices up to 11” 10-device wall mounted AC charging cabinet for Surface Pros and other USB devices up to 13”
“Technology and data are helping to improve people’s lives every day, whether ordering a repeat prescription through the NHS App, getting the latest health advice from the NHS website, or arranging a Covid vaccine using our national online booking service.
“We’re proud to be making a real difference to both colleagues in the NHS and the people that it serves.
“The merger will help us continue that journey as one central organisation, using digital to transform the NHS and provide the best care possible for patients.”
History and role
NHS Digital was created as a special health authority by a merger of the National Programme for IT, part of the Department of Health, the NHS Information Authority, and the Prescribing Support Unit in 2005. Then known as the Health and Social Care Information Centre (HSCIC), the organisation changed from a special health authority to an executive non-departmental public body in 2013, following the Health and Social Care Act 2012. HSCIC took over parts of the NHS National Programme for IT from the agency NHS Connecting for Health (CfH) which ceased to exist at this time. In 2016, HSCIC was rebranded to NHS Digital.
NHS Digital designs, develops and runs national IT and data services that support clinicians at work, provide care to patients and use data to improve treatment.
Achievements
NHS Digital builds and runs the NHS App, NHS login and the NHS website. NHS 111 and most 999 centres use NHS Digital algorithms.
According to NHS Digital, their national digital systems and platforms operate with 99.98 per cent reliability.
NHS Login is used by patients and the public to access digital health and social care services with a single login. There are 44 million confirmed NHS login accounts. There are also 26.9 million verified users of the NHS App. NHS Digital is also responsible for cyber and data security, protecting the NHS
and care organisations from cyber attacks and constantly monitoring for new threats.
NHS Digital teams provide cyber advice, assessments, training and resources. NHS Digital sees 3 billion firewall transactions a day.
NHS Digital created the Electronic Prescription Service, which allows prescribers to send prescriptions electronically to a dispenser, which makes the process more efficient and convenient for patients and staff. It means patients can collect repeat prescriptions from a pharmacy without visiting their GP and it also means a reduction in the use of paper. 97.6 per cent of GP practices and pharmacies now use the Electronic Prescription service. NHS Spine facilitates messaging across key services and platforms and is run by NHS Digital. 1.6 billion transactions are carried out per month on NHS Spine allowing the secure sharing of information.
NHS Digital was also involved in the creation of the NHS Covid-19 App and the online National Booking Service to book Covid vaccinations.
The organisation is using the latest technology to help address the current NHS pressures, through expansion of virtual wards and 24/7 system control centres.
NHS DigiTrials supports clinical trials that are developing new treatments to improve health and care, by providing safe and authorised access to data.

Data protections
According to NHS England, all existing protections for data will be transferred. However, concerns have been raised..
Draft guidelines have been published setting out the new NHS England dataprotection obligations, which are intended
to ensure at least the same degree of protection, safeguards and transparency over data use as NHS Digital provided. However, in an interview with Health Service Journal, National Data Guardian Nicola Byrne voiced concerns about the implications for data following the merger of NHS England and NHS Digital and remarked that there is “an inherent tension in having one organisation be both data custodian and the organisation seeking to access the data”.
In May last year, former NHS Digital Chair Kingsley Manning wrote to The BMJ calling its merger with NHS England a “significant retrograde step in defending the rights of citizens with respect to the collection and use of their health data” and warning that it had “the potential for undermining the relationship between clinicians and their patients”.
Talking about the merger, health and social care secretary, Steve Barclay, said: “New technology and better data about how our health and care system is working at the frontline is key to improving care for patients.
“Bringing the latest digital tech into the heart of the NHS will help join up services and streamline decision making, boosting our recovery from the Covid pandemic and reducing waiting times.”
NHS Digital has previously done and continues to do a lot for the health service, to keep it running efficiently, modernising services and making improvements for health and social care.
It is hoped that the merger will continue to bring these benefits and more. L
FURTHER INFORMATION
Read more
IT
The organisation is using the latest technology to help address the current NHS pressures, through expansion of virtual wards and 24/7 system control centre
Don’t let this happen again!
In May 2017 a global ransomware attack known as WannaCry affected more than 300,000 computers in at least 100 countries, which in the UK particularly affected the NHS.

According to NHS England, the WannaCry ransomware affected at least 80 out of the 236 trusts across England, because they were either infected by the ransomware or turned off their devices or systems as a precaution. A further 603 primary care and other NHS organisations were also infected, including 595 GP practices. It was estimated to cost the NHS £92 million after 19,000 appointments were cancelled as a result of the attack.

Reduce the risk of this happening again and book a Vulnerability Assessment today from only £29 per user!
Its not a matter of IF you get hacked, but WHEN…

For more information, please click on the links below info@cybersecuresolutions.co.uk www.cybersecuresolutions.co.uk
How to support nurses in cybercrime prevention
The UK’s use of medical IoT is growing, with 75 per cent of all medical devices now connected to the internet. But despite the numerous benefits of these connected devices, it leads to inherent security vulnerabilities that are difficult to patch and secure. Since the healthcare sector stores large volumes of confidential data together with a network of connected medical devices, it makes healthcare organisations a prime target for cyber criminals.
Medical devices used in hospitals include everything from infusion pumps that administer lifesaving drugs, to radiological cancer treatment systems in the treatment of tumours. It has been reported by the Interim CIO at NHSX that 21 million items of malicious activity get blocked every month within the NHS. As the largest employer in the UK, the NHS is a target due to the sheer value of its medical data. At present, 30 per cent of the world’s data is generated through the healthcare sector, and this is due to increase to 36 per cent by 2025.
40 per cent of the 777 compromised email incidents managed last year by the National
Cyber Security Centre were aimed at the public sector. The level of security under which these medical devices should be placed should not be underestimated. In the past, even simple healthcare functions such as the scheduling of medications has been affected by ransomware. The issue of cybersecurity for medical devices is not isolated merely to patient confidentiality but can affect the ability and availability of the NHS services that are critical to ensuring patient safety. This calls for an urgent need of investment into cybersecurity training for nurses so they can help protect these critical devices used within hospitals. Through regular training for medical teams, nurses will be able to spot the vital signs and detect when a cyberattack is occurring, and how to mitigate any risks to patient safety.
Managing IoT medical devices to minimise threats
The need here is to address cybersecurity through the product lifecycle in a preventative and proactive way, as well as incorporate an approach to cybersecurity

that puts high quality IT at the centre of a healthcare organisation’s infrastructure. A risk-based approach that begins with the identification of at-risk IT assets, followed by management of trade-offs between risks and benefits, as well as different types of risks. The training of healthcare personnel is emphasised, alongside implementation of strategies that deal with vulnerability and device patch management, the controlled and restrictive granting of administrative privileges, and the development of incident response and business continuity plans.
Configuration management and change management are what the Information Technology Infrastructure Library (ITIL) describes as a systematic approach to handling all medical device changes in a standardised method. Proper management of these changes not only avoids unnecessary service downtime but is critical during a cyberattack. An incident response plan can be a version of change management. Similarly, strict audit logs and monitoring of data records are critical for IT functions to quickly recognise attacks and prevent a breach before it even occurs.
To minimise cyber threats and vulnerabilities, healthcare establishments are also encouraged to install intelligent cybersecurity systems which easily integrate and add value to existing healthcare infrastructure. With single dashboard views, such systems monitor and flag anomalies thanks to a streamlined approach to IoT cybersecurity. IoT and medical E
Feature Heading
Phil Howe, CTO of Core to Cloud and Richard Staynings, cybersecurity strategist at Cylera
Cybersecurity
Written by Phil Howe, CTO of Core to Cloud and Richard Staynings, cybersecurity strategist at Cylera
Issue 23.1 | HEALTH BUSINESS MAGAZINE 57
40 per cent of the compromised777email incidents managed last year by the National Cyber Security Centre were aimed at the public sector





Secure Configuration Management DON'T ASSUME, KNOW FOR SURE www.gytpol.com We are already helping the NHS transform ineffective manual methods via innovative automation FAST, ACCURATE, SECURE. Gytpol automates the detection & remediation of your misconfigurations and validates compliance on endpoint devices. All of this with zero impact and zero fuss. Saving you time and reducing your cost of ownership. Over 80% of ransomware attacks are attributable to device MISCONFIGURATIONS. A major pain-point for NHS organisations as existing tools don't detect them. Contact us to find out more.



Issue 23.1 | HEALTH BUSINESS MAGAZINE 59
UK Cyber Week begins in April
UK Cyber Week – Expo & Conference is taking place at the Business Design Centre, London on 4 and 5 April 2023
At 07:00 BST on the 4 August 2022 – NHS IT provider, Advanced, identified they had been compromised by a ransomware attack and immediately started responding to contain the hackers. They issued a statement to address the growing concern, “We are rebuilding and restoring impacted systems in a separate and secure environment” The NHS also responded with a statement “… the NHS has tried and tested contingency plans in place including robust defences to protect our own networks…”.
Over two months later, chief executive of Oxford Health Foundation Trust, Nick Broughton, said problems were still ongoing, “One shouldn’t underestimate the impact this has had on our organisation… it is compromising our ability to deliver the quality of care that we would like to…”. Advanced had initially said that only a “small number of servers” had been affected and that it might be able to recover in a week.
This attack and 2017’s shocking WannaCry ransomware attack are two examples which remind us that defending the NHS is, despite best efforts, a very tall order. The NHS is an enormous, complicated organisation with 1.22m full-time employees, 219 separate trusts and over 8,000 suppliers within its supply chain. It must fight on multiple competing fronts which include staffing, funding and the elective care backlog whilst trying to improve services, transform digitally and protect itself from increasingly sophisticated cyber criminals. But why would someone target the health sector though? It could be that health services
are often targeted because they have large vulnerable supply chains, plus their services are vital, so there is a good chance of extracting a ransom. Of course, there is also a huge reservoir of potentially valuable data to harvest which can be monetised without anyone even being aware there’s been a breach.
According to Experian, stolen patient records on the dark web sell for between $250 and as much as $1,000. As a comparison, credit card numbers sell for around $5 each and Social Security numbers can be purchased for as little as $1 each. Patient records are way more valuable because a credit card can be easily cancelled, whereas medical records contain lots of valuable persistent data, such as a patient’s medical health history, demographics, as well as their health insurance and contact information.
Once records are stolen, cybercriminals can harness the growing network on the dark web and connect with different criminal skill sets such as drug traffickers or money launders. They are eager to buy medical records for their own criminal activities, such as illegally obtaining prescription medications, false medical claims or using the patient’s identity to open credit cards and take out loans.
So, what is the way forward? Well, it’s not easy but lessons have been learned and there are some clear straightforward measures which can help. Ransomware attacks tend to be initiated using phishing emails, so it is important that all staff are aware of the dangers of clicking on suspicious links. Of course, it’s also crucial to make sure that there are appropriate data back-up processes, and that strong disaster
recovery and business continuity plans are prepared for ransomware attacks. Other simple precautions include ensuring software is up to date, patched and, crucially, adopting a mindset that cyber security is everyone’s responsibility.

The idea that cyber security is everyone’s responsibility is one of the key drivers behind a major new cyber conference and expo - UK Cyber Week. It is a completely free event focused on levelling up the cyber security knowledge for cyber, IT and operational leadership teams. There are over 100 seminar sessions covering all aspects of cyber security and there really is something for everyone no matter how much they know about cyber.
The organisers have developed a unique rating system which grades each session on how technical it is, ranging from level 1 – “Absolute Beginner” to level 6 “Engineer/ Hacker” this allows attendees to self-select the content that’s the right level for their understanding of cyber issues. It also ensures that the speakers know what level to deliver their session. Everyone’s time is precious, so we wanted to make sure that if you do spend your valuable time with us at UK Cyber Week, it is as efficiently used, and you will learn as much as possible.
There is a definite image problem for cyber security in the world of those who aren’t cyber security experts – it can be seen as complicated, or a nuisance, a distress purchase. “How much will it cost to be safe?” is a somewhat impossible question to answer and of course anyone can be hacked, Sony, Apple, and the NHS. Also, you can’t buy a product and make the problem simply go away so it can be neglected, or the concern simply outsourced to a siloed IT team – let someone else worry about it all! Fixing this image problem is one of the key missions of UK Cyber Week – how do you bring the subject to life for someone whose day job isn’t cyber but who does have influence over budgets or policy? How do you make it interesting, engaging, and educational. The organisers are particularly thrilled with one innovative session entitled “Confessions of a Hacker” – delivered by a real-life hacker. Back lit and speaking through a voice modulator off stage to protect their identity, they will share insight into how they hack facilities including critical national infrastructure, airports, and casinos. This is certainly one not to miss and their genuinely shocking insight into how it all works and how easily your own setting could fall to the techniques they use.
There is a fascinating live interview with Cecilie Fjellhøy, star of Netflix’s most watched documentary – The Tinder Swindler. Cecilie’s story is enough to scare anyone off dating apps, but we must be clear this is not about dating apps – it’s about fraud and deception. Cecilie is an intelligent, professional woman and shows how criminals are increasingly
ADVERTORIAL
Event Preview
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 60
sophisticated striking in unexpected ways. High-value NHS staff and leadership can represent tempting targets for fraudsters, and it is a genuinely shocking story.

Jayson E Street, somewhat of a rockstar in the hacking world, is jetting in from Austin, Texas to show how social engineering is used to trick people. By watching a bank robbery in real time (via a hidden camera) the audience will see that even in high security areas people can still be a victim of their assumptions. The audience will understand that while most people have biases, they may not even be aware of, they can be trained to spot suspicious behaviour. People will learn that untrained workers are a serious threat, yet workers educated in Security Awareness can be the biggest asset for a company’s security.
The content program also has lots of interesting speakers for the more technical audience too – speakers such as Google’s Chris John Riley exploring minimum standards in application security and Forescout’s Daniel Dos Santos who demonstrates a proof-ofconcept malware that exploits IoT devices for initial access, moves laterally on the IT network, and then holds OT devices hostage!
There is also a growing threat from outside the commercially motivated cyber criminals, these days nation states and activists are a very clear and present danger. Someone who has had exposure to this offensive computer network exploitation is ex US Department of Defence operative, Daniel Gericke. Daniel just doesn’t speak at conferences, so it is a real coup to be able to hear from him at UK Cyber Week.
The content program is hosted on a main keynote stage and 5 themed breakout theatres:
Resilience Theatre - Covering organisations ability to prepare for, respond to and recover from cyber attacks Strategy Theatre - Focusing on the latest threat landscape and trends, and how to develop a robust cyber strategy in response to a changing world Culture Theatre - How to build a strong human-based element to cyber security. Covering psychology, training, policies, leadership, recruitment, and retention Prevention Theatre - Arming you with the tools and thinking to prevent the next attack including monitoring, intelligence, zero trust and vulnerability management OT Security Theatre - Up-to-the-minute expertise covering the risks and best practices in protecting physical processes and devices, industry, and critical national infrastructure Networking is also a key part of UK Cyber Week’s philosophy and there are opportunities to immerse yourself into
the growing cyber community in the networking bars, the evening meet ups and at the big show party, organised in conjunction with Cyber House Party. UK Cyber Week is completely free to attend event and if you would like to visit you can register through the website

Tell your network and bring your colleagues - Cyber security is all about people and there is no doubt we are all in this together. Protecting everyone in the health sector, staff, patients, and the supply chain is something we can certainly all get behind. Everyone here at UK Cyber Week hopes that you enjoy your visit and come away with actionable insight which you can use right away. L


FURTHER INFORMATION
Find out more and get your free ticket here: https://hubs.la/Q01BgWcd0
Issue 23.1 | HEALTH BUSINESS MAGAZINE 61


BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 62 Improve patient safety in your organisation Scan the QR code shown to book a meeting with one of our team on the day www.radarhealthcare.com Talk to us about our event modules: • Incidents (PSIRF) • Learn from patient safety events (LFPSE) • Complaints and PALS • Claims • Freedom of Information Requests • Mortality Reviews • Bereavement Be ready for LFPSE and PSIRF We will be at the Digital Health Rewired Event on the 14th and 15th March at London’s Business Design Centre
Digital Health Rewired 2023
Digital Health Rewired returns on 14-15 March 2023 bringing the UK’s digital health community together at a pivotal time for the sector
Members of the fast-evolving, dynamic multi-disciplinary community – including NHS and social care, private healthcare, suppliers, start-ups, innovators, policy makers and patients – will convene at London’s Business Design Centre to debate the most pressing topics across eight CPD-accredited stages. Here’s a preview of what’s to come.
Future direction for national policy
Just months after NHS Digital’s planned merger with NHS England in January, Dr Tim Ferris the latter’s director of transformation will speak on the National Policy and Keynote Stage. With major changes in programmes and priorities afoot, Tim will share the next steps for digital and data to support NHS recovery, help alleviate pressures and underpin future delivery of safe, convenient, and equitable health services. Joining Tim will be the interim CEO of NHS Providers, Saffron Cordery. She will draw on experiences from NHS Provider’s digital board programme to outline the next steps for delivering digital at trust-level against the backdrop of political structural reform. Digital is an becoming an increasingly effective tool to address health inequalities, according to Richard Stubbs. The CEO of Yorkshire and Humber AHSN and vice chair of the AHSN Network will explore how digital solutions can be scaled to different geographical variations, ages and levels of affluence, sharing digital inclusion case studies
from the Yorkshire and Humber region. From policy to patient flow. In December Dr Vin Diwakar, the medical director for secondary care in NHS England’s national medical care and transformation directorates, announced the go-live of 40 new data-driven traffic control centres to help local NHS teams manage hospital capacity in real time. Rewired delegates will hear Dr Diwakar share how science, technology, digital and data is being used to address improvements in patient outcomes and relieve under-pressure NHS services.
Charting the digital course for integrated care
Fast evolving integrated care systems (ICSs) are finding their feet with digital leaders being appointed to explore new ways to deliver integrated health and social care. On Rewired’s Integrated Care Stage, you’ll hear from pioneering teams making integrated care a reality, with examples of work from across the country on delivering shared care records, population health, patient portals and remote care at scale. Rob Webster, CEO of West Yorkshire Health and Care Partnership is one of the true pioneers of integrated care systems. He will
discuss key challenges in delivering ICS digital strategy and investment priorities. While Lisa Emery, chief transformation, innovation and digital officer for NHS Sussex ICS, and chair of the CIO Network, will share her experiences of moving from an NHS trust to ICS-land and the required shift in focus and priorities.
Developing roles of digital nursing
The vibrant fields of digital nursing, midwifery, AHPs and pharmacy continue to develop at pace. Back for the second edition, the Digital Nursing Summit –which now runs across two days – will focus on latest developments and showcase digital leaders and initiatives of all four sectors from across the NHS.
Keynote speaker Dr Natasha Phillips, CNIO at NHS England will share findings from the May 2022 Phillips Ives Review, outlining the next steps for empowering England’s 300,000-strong nursing and midwifery workforce to deliver the NHS’s digital future. Key themes include how to reduce documentation burden, the influence of shared-decision-making councils, quick-fire career snapshots sessions and interactive debates around the digital roles across nursing, midwifery, AHPs and pharmacy. E

Digital Health Rewired
Issue 23.1 | HEALTH BUSINESS MAGAZINE 63
dataHow is being used to improvementsaddress in patient outcomes and relieve under- pressureservicesNHS

Confirmed speakers include national representatives Helen Balsdon, acting CNIO & director of digital clinical safety, NHS England, and Fran Beadle, CNIO of digital health and care Wales, NHS Wales.
Local digital leaders on the programme include Sarah Thompson, CCIO, Wirral University Teaching Hospitals NHS FT; Misbah Mahmood, digital midwife at Leeds Teaching Hospitals; Sarah Hanbridge, CCIO for nursing & AHPs, Leeds Teaching Hospitals NHS Trust, and chair, CNIO Network; and Ramandeep Kaur, CCIO, NHS University Hospitals of Northamptonshire.
Service transformation at scale
The Digital Transformation Stage will showcase how digital is enabling health service transformation at scale in the NHS and internationally. Delegates will learn lessons from leaders who will share their experiences of implementing successful digital transformation programmes.
Teams at Gloucestershire Royal Hospital and University Hospitals Birmingham are working to simplify Gloucester’s lung cancer pathway, which includes 34-87 steps, 14 clinical systems and 15 different specialities, through digitisation and automation. Doctors and researchers from the trusts will explain how at this key Rewired session. How do we prepare NHS staff to help deliver the digital future? Helen Thomas, CEO of Digital Health & Care Wales, named the best place to work in IT at the British Computer Society’s annual UK IT industry awards in December 2022, will speak about how to build a digital workforce, with FEDIP’s CEO, Andrew Griffiths.
Richard Corbridge will bring a patientfocused perspective on digital transformation. The CIO of pharmacy chain, Boots, will be talking about personalised health on the high street and the potential to support service transformation across the NHS.
The critical era of smart health Smart networks and infrastructure provide the essential basis for digital health and care. This is the focus on day one of the Smart Health Stage. Software, data and sensors are increasingly embedded into
worldwide networked medical equipment and physical fabric of healthcare buildings and facilities. We explore the questions such as where does the NHS stand on cloud, sustainability and green IT?
Day two of Rewired explores how health and care are now critically reliant on IT infrastructure, digital services, smart networks and medical IOT. What are the next steps in securing and ensuring the availability of vital digital networks, assets and data?
Cyber security is firmly back in the NHS spotlight again after the August cyber security attack on supplier Advanced which disrupted NHS 111 and has left 12 mental health trusts without access to vital patient records. At this must-attend Rewired 2023 stage, learn how the NHS can level-up its cyber security resilience to best protect patient data and avoid disruption to health services.
The NHS’s security chief Mike Fell is the day two keynote for the Smart Health Stage. Hear the NHS cyber security boss discuss the latest developments in national cyber strategy for healthcare, incidents, cyber threats and best practice in managing risk.
Where next for AI and analytics? How are AI, data and analytics being used to drive healthcare innovation?
The AI, Data & Analytics Stage explores the key emerging challenges and opportunities around research, and the latest use of new analytical and predictive capabilities to support patient care.
Renowned doctor, academic, writer and broadcaster, Prof. Ben Goldacre, returns as Rewired keynote speaker. Hear directly from the author of ‘Better, Broader Safer’, the review into better using health data for research and analysis published in April 2022. His recommendations included making Trusted Research Environments the model for accessing NHS patient records data, and creating more career and development opportunities for NHS data analysts.
Start-ups and scale ups square up Over 80 of the hottest digital health startups and scale ups across Europe, the
US and Canada have entered Rewired Pitchfest 2023. The live final of the entrepreneurial competition, which offers entrants a game-changing opportunity to win an NHS test bed site, takes place on day two, Wednesday 15 March.

Eight finalists will be put through their paces by a panel of VCs, investors and NHS tech leaders before one start-up or scale up is crowned Pitchfest 2023 champion. 2022 winner Dr Rachael Grimaldi, Chief Executive of CardMedic who returns as a judge, says: “There’s no better opportunity for young digital health companies to get in front of a relevant, interested, engaged audience.”
Pioneers share digital successes
Shining a spotlight on pioneering digital projects from across the NHS provides a shared knowledge base to enable transformation efforts to scale. Running across the two days of Rewired as a show-floor feature, the Best Practice Showcase blends curated open call sessions from NHS presenters with best practice sessions from suppliers. These quick-fire sessions will offer actionable takeaways from NHS pioneers and industry experts to take back to your organisation. They are ideal for anyone looking for insights and inspiration for your next highimpact digital project or programme.
Join the community at Rewired Rewired 2023 is the premier education and networking event for all members of the UK digital health community; bringing the best of NHS IT, digital, data and innovation under one roof. The event is free for NHS, public sector, charities and education. Follow updates via #Rewired23. Register your place at: www.digitalhealthrewired.com L
FURTHER INFORMATION
Register your place today at digitalhealthrewired.com/register
Issue 23.1 | HEALTH BUSINESS MAGAZINE 65 Digital Health Rewired

Your data is your best line of defense rubrik.com/ransomware
Changing the conversation around AI
Ahead of his session at Digital Health Rewired in March 2023, director of AI, imaging and deployment at the NHS Transformation Directorate, Dominic Cushnan, explains the need to focus on supporting NHS organisations to deploy AI technologies

Artificial intelligence (AI) has been hailed as a utopia to solve many healthcare problems, but so far, we have lacked much of the evidence to demonstrate its effectiveness or create frictionless mechanisms to allow NHS organisations to adopt AI technologies. We’ve had the pandemic, and now we face the challenges of waiting lists, backlogs and workforce recruitment. People are asking how we can apply technology such as AI to address these issues.
Research
One of the things we’re really good at in the UK is research and coming out with papers and models for how AI could help solve challenges in healthcare. However, we are still to crack the puzzle of how to translate this research into solutions that can be used by the NHS today.
Currently we’re testing and evaluating 77 projects, through the AI in Health and Care Awards to see which technologies can benefit the NHS. The next step is to take this work and scale it up so hospitals can start implementing these technologies to improve patient care. For the NHS AI Lab, that means moving the conversation onto prioritising our activities towards deployment, rather than research.
At the AI Lab we’re working on how to deploy AI based on existing evidence rather than the hype. In many instances algorithms are the end user case of the wider digital transformation programmes within NHS England (NHSE). There’s a lot we need to get right first like basic digitisation and getting infrastructure in place, so these models can be integrated into clinical pathways in an appropriate and safe manner. That needs to be wrapped round the work we’re delivering on AI ethics, clinical workforce training and ongoing patient safety programmes.
The programme of work at the AI Lab has been an enabler around how we can support these technologies and provide assurances.
We have a robust regulatory system, which requires several different agencies to bring a product E
Digital Health Rewired Issue 23.1 | HEALTH BUSINESS MAGAZINE 67
At the AI Lab we’re working on how to deploy AI based on existing evidence rather than the hype






to market. The AI Lab has funded the development of a multi-agency advice service (MAAS) to give innovators and health and care providers a one-stop shop for support, information and guidance on the regulation and evaluation of AI technologies. The MAAS is currently in beta testing stage and we plan to launch it as a service in Summer 2023.

Deployment and integration
I believe we should focus on deployment (machine learning operations) in a couple of areas, such as radiology and emergency medicine, where AI technologies are mature, and we can think about how to integrate these algorithms into the clinical pathway to support decision-making and enable clinicians to help patients. By starting with addressing one use case for deployment, such as radiology AI solutions, we hope to create blueprints and case studies which can be used to solve AI adoption problems from IG compliance to infrastructure to standards to scalability in other areas. That plays nicely into the work we’ve all been doing since the NHS Long Term Plan on building up imaging networks and community diagnostic hubs. We’re looking at how we can provide the appropriate level
of algorithm support in those areas quickly, rather than piecemeal by piecemeal. We have some good work that’s already underway. In 2022, we worked with the NHS Shared Business Services to launch the AI Software in Neuroscience for Stroke Decision Making Support Framework Agreement, allowing people to buy AI technology on the stroke framework. The use of AI has the potential to speed up the diagnostic process, which is crucial in stroke where significant harm and long-term disability can be caused if left untreated.
AI in use
One of the technologies we funded through the AI Awards is Oxford University spinoff Brainomix. The startup provides a set of tools that uses AI methods to interpret acute stroke brain scans and helps doctors make decisions about treatment and the need for specialist transfer of patients. Brainomix also provides a platform for doctors to share information between hospitals in real-time. This is now being deployed in nine stroke networks, which is around 50 per cent of stroke services in England. Another example is the deployment of startup Adience’s AI platform which is being
used for the NHSE Targeted Lung Health Check programme. It provides the Veye chest system that supports early lung cancer detection by acting as a ‘second reader’ to help relieve pressure on radiologists. We’re also supporting work in diabetic ophthalmology to make sure we don’t have any failure points around ethical decisions. The AI Lab is funding a programme of work to ensure that AI technologies that detect diabetic retinopathy work for all, by validating the performance of AI retinal image analysis systems that will be used in the NHS Diabetic Eye Screening programme in different subgroups of the population. AI technologies are one piece of the digital transformation picture, but sometimes they can be at odds with what clinicians need. With many technologies on the market, we need to make sure we are working with the Royal Colleges and clinical staff to understand where AI can help and provide them with the support and assurances they need to use it with confidence. We just published a second report with Health Education England (HEE) identifying workforce training needs to provide confidence in the use of AI. Ultimately the aim of using AI is to improve patient care and outcomes whilst freeing up clinicians’ time and making their jobs easier so they can spend more time with patients. These technologies have the potential to lead to faster diagnostics and more targeted interventions at a population health level. AI can improve the health of the nation long-term, but we need to deploy it safely and with the right evidence. L
FURTHER INFORMATION
https://digitalhealthrewired.com
Digital Health Rewired Issue 23.1 | HEALTH BUSINESS MAGAZINE 69
With many technologies on the market, we need to make sure we are working with the Royal Colleges and clinical staff to understand where AI can help and provide them with the support and assurances they need to use it with confidence
What’s in a name? The under-recognised role of digital midwives
By Misbah Mahmood,
digital midwife at Leeds Teaching Hospital NHS Trust, who will be speaking at the Digital Health Rewired Big Debate: What’s in a name? Titles, Roles and Teams in digital nursing, midwifery, AHP and pharmacy
The role of a digital midwife has traditionally been under-recognised, but that is now thankfully changing.


In March 2021, the Royal College of Midwives launched a position statement calling for every trust in the country to recruit, or train, digital midwives. And, in the same month, NHSX launched a new national digital midwife role.
I was among the first generation of digital midwives and was recruited into my role five years ago, initially as a six-month secondment. Since then, I’ve joined a huge online community of digital midwives and today I’m part of a team of seven. My role has evolved hugely over the years and I’m keen to highlight not only its unique importance, but – also – how much it resembles the work of digital nurses and chief clinical information officers (CCIO).
So, we need to all work together to deliver digital transformation.
A unique role
Digital Midwives are specialists in delivering digital transformation in maternity services. Whereas a digital nurse will understand bed care plans and the use of digital in nursing wards, the digital midwife focuses specifically on maternity.
There are some differences between digital midwives and other specialities. We have the baby to think about and safeguarding is an issue, especially if the child is fostered or adopted.
Also, one patient enters the maternity episode of care, but (hopefully) two patients leave.
What’s in a title?
But we shouldn’t get bogged down with titles. Most of the work of digital midwives resembles the digital nurse and CCIO roles closely and is equally important. On a day-to-day basis, I spend my time on similar tasks, but in a maternity context.
For example, I engage with suppliers and stakeholders about the scope of digital transformation projects. We work towards national initiatives, maintain computer systems, elicit feedback from service users, and help teach and train clinicians.
Most of my skills are transferrable to other digital roles. For example, data
analysis and considering how systems will affect patients. I have project thinking and management skills and have carried out large-scale digital implementations. I also try to understand how digital change can work in practice. For example, logging in and out of five different systems where half the data is missing is never going to be fit for purpose. Many of the challenges I face are also common to digital roles in other parts of the hospital. Interoperability is something CCIOs, digital nurses and midwives all think about in our job.
Working in collaboration
As such, it’s essential for digital midwives to avoid working in a silo. We need to work together with CCIOs and digital nurses to ensure seamless data sharing and delivery of digital care.
It’s important to realise that, when a woman or birthing parent’s data is managed through a Maternity Information System (MIS), this is only a single episode in that patient’s journey.
Once the patient (and baby) leaves the maternity services for postnatal care, they are no longer a maternity-specific patient. They move from the maternity ward, and their data also transfers to more general nursing and clinical information systems.
A growing role
Working together has grown more important with the growth of the digital agenda in the last five years. Increasingly NHS trusts are dealing with the introduction of artificial intelligence, for example, and patient expectations are also growing. Patients today can unlock their car with their mobile phone and even access their bank account,
so why do they still have to bring paper notes to their antenatal appointment?
No one wants to travel across Leeds with a paper folder when they could access it, from their phone, at the touch of a button. It’s much easier to transfer a woman or birthing parent to another trust if the clinical record is stored digitally. IT teams alone are often unable to keep up with demand. Midwives today, for example, are heavily dependent on laptops to do their job. Part of my team’s role is helping ensure midwives have the right hardware whenever they need it.

Pioneering the Future
I’ve been incredibly lucky that my trust pioneered the digital midwife role at a time when it had less recognition. Today I’m one of two digital midwives at the trust, aided by two band 6 support midwives and three band 3s. I was lucky to have the opportunity to complete a one-year Florence Nightingale Leadership Scholarship, which led me to be mentored by a CIO. Today’s digital midwives have even more opportunities thanks to a PG Cert for Digital Maternity Leaders at Imperial College
We look forward to being joined by two new digital midwives within the next couple of weeks, who have a great future ahead of them. L
FURTHER INFORMATION
https://digitalhealthrewired.com
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 70 Digital Health Rewired
Digital Midwives are specialists in delivering transformationdigital in maternity services
Redefining the modern laboratory
Clinisys is a global provider of intelligent diagnostic informatics solutions and expertise designed to redefine the modern laboratory, across healthcare, life sciences, and public health. Millions of diagnostic results and data insights are generated every day using Clinisys’ solutions in over 3,000 laboratories across 34 countries.
For more than forty years, Clinisys has served laboratories operating in a range of industries and disciplines. We have helped them to apply a variety of different scientific specialisations to solve their testing, research, and diagnostic challenges.
We equip labs with the efficient workflows, accessible data, and innovative tools needed to offer improved decision making, rapid testing, and advanced diagnostic services. We enable them to prosper and innovate within their specialisations.
By defining the optimum modern laboratory platform, we have
enabled labs to scale rapidly, respond to their customers with agility, and maximise the potential of a modern cloud architecture and data model to improve their services and capabilities.
Clinisys’ mission is to enhance the effectiveness of diagnostic workflows in any laboratory or testing environment to keep citizens and communities healthier and safer.
Please visit us at Digital Health Rewired, Stand A2, to discuss your requirements and to see our latest products and solutions. L
FURTHER INFORMATION
www.clinisys.com

Securing the world’s data
Market-leading records management consultancy

Rubrik is a cybersecurity company, and our mission is to secure the world’s data. We pioneered Zero Trust Data SecurityTM to help organisations achieve business resilience against cyberattacks, malicious insiders, and operational disruptions. Rubrik Security Cloud, powered by machine learning, delivers data protection and cyber resilience in a single platform across enterprise, cloud, and SaaS applications. Our platform automates policy management of data and enforcement of data security through the entire data lifecycle. We help organisations uphold data integrity, deliver data availability, continuously monitor data risks and threats, and restore businesses with their data when infrastructure is attacked. Rubrik Security Cloud is a data security platform that keeps
your data secure, monitors your data risks, and quickly recovers your data, wherever it lives.
Built on zero trust architectural principles, Rubrik Security Cloud empowers organisations to: preserve data integrity and keep data readily accessible to withstand cyberattacks, malicious insiders, and operational disruptions; reduce your data risks by continuously monitoring for emergent cyber threats such as ransomware and sensitive data exposure and surgically and rapidly restore your impacted apps, files or objects by containing threats and orchestrating recoveries while avoiding malware reinfection. L
FURTHER INFORMATION
For more information please visit www.rubrik.com
EDM Healthcare Consulting are a niche, market-leading consultancy focused on records management. With the current focus on frontline digitisation, EDM Healthcare Consulting are well placed to provide specialist support and subject matter expertise in helping healthcare organisations overcome the challenges of health records digitisation & electronic document management projects. When implemented correctly, EDM solutions can deliver tangible savings along with providing a foundation for digital maturity to be built upon. We offer full project lifecycle services to NHS Trusts and Health Boards, from strategic
review, gap analysis, business case development, through to implementation delivery and post implementation reviews. We also offer support for EDM software & scanning vendors. Come meet us at Digital Health Rewired (Stand D21) to discuss how we can help your organisation with your records management strategy and deliverables. L
Find out more at:
info@edmhealthcareconsulting.co.uk or visit our website below.
FURTHER INFORMATION
edmhealthcareconsulting.co.uk

4C Strategies – Independent ICT Consultants
4C Strategies is an independent ICT consultancy specialising in technology and infrastructure projects. The company covers all aspects of technology and infrastructure in the enterprise environment, with consultants showing demonstrable experience in helping clients to procure new technologies to meet their business requirements, providing endto-end support on ICT projects by delivering a portfolio of consultancy services to meet client requirements, from audit and strategy through to procurement, implementation and resourcing.
4C Strategies has been assisting organisations in the healthcare industry for over 20 years. Expertise covers

all aspects of IT technology and infrastructure, including: digital strategy, IT and technology strategy, data centres, servers and storage, patient data security, desktop telephony, Microsoft Teams and wide area networks.
Trevor Nelms, Director from West London Mental Health Trust, said: “4C Strategies has assisted in a range of complex ICT projects, from inception through to deployment, and demonstrated a rare ability to bring together technical expertise with business acumen and tight project management skills.”
Contact one of 4C Strategies’ qualified healthcare technology consultants today. L
Issue 23.1 | HEALTH BUSINESS MAGAZINE 71
FURTHER INFORMATION Tel: 01858 438938 nhs@4c.co.uk www.4c.co.uk
THIS tackling health inequalities with digital technology
How a digital approach has tackled health inequalities among minority ethnic and vulnerable patients
Significantly longer waiting times for elective surgery among certain patient groups, particularly those in minority ethnic communities and areas of deprivation, have been dramatically reduced thanks to digital innovation between a health trust and the informatics service it hosts.
Analysis carried out by The Health Informatics Service (THIS), which is hosted by the Calderdale and Huddersfield NHS Foundation Trust, found that in May 2021 patients from a minority ethnic background were waiting almost eight weeks longer, on average, than white patients for a ‘priority two’ (P2) operation – which NHS guidelines state should be treated within a month of prioritisation.
It also found patients from the most deprived communities were waiting 8.5 weeks longer than those from better off areas, prompting leaders at the trust, which runs Huddersfield Royal Infirmary and Calderdale Royal Hospital, to turn to THIS for a digital route into solving the issue.
Digital interventions created and implemented by THIS through its collaboration with the Trust’s executive team, performance analysis staff, general managers, senior clinicians and appropriate information staff resulted in waiting lists for ethnic minority patients dropping by almost five weeks on average within six months, while those from deprived areas saw the wait cut by an average of six weeks. Since then, average waiting times for both groups have virtually been eradicated and the digital prioritisation markers are being applied to patients with other characteristics, such as learning disabilities, frailty, obesity and mental health issues.
How the improvements were achieved
Calum MacIver, THIS’s corporate information manager, explains: “Our Information Team started pulling together figures from our data warehouse into the trust’s business intelligence platform, referred to locally as Knowledge Portal+ (KP+), using Qlik Sense and added in nationally available data, such as population information, deprivation and census data.
“This led to a larger, all-encompassing health inequalities model, where markers were attached to patient data at source. It created a new method of looking at waiting lists, that didn’t just examine total numbers but started to factor in the data from the perspective of the different patient characteristics, and it has created a new
culture within the trust and us, where we take account of inequality in everything we do.”
The results were achieved with the following, extensive, set of measures: Review and improved data quality; analysis of waiting time data; reviewing waiting times across pathways to establish points of divergence; dedicated contact team established for scheduling patients; new pathways being developed; weekly inclusion of data in leadership briefings in addition to internal and external engagement; and clinical reference group established and dataset by specialty and consultant developed.
This has led to the introduction of individual patient planning, a new care pathway in the trust’s electronic patient record, where a flag identifies patients on referral. Individual priority pathways for patients with a learning disability is sustaining the change, as is a children’s waiting list validation and prioritisation, and dedicated vaccine clinics.
The collaboration is now exploring cancer activity profiles and waiting list addition trends and more closely involving clinicians in the data analysis process.
Winning plaudits and attracting attention
The work done by THIS, and its host trust has been included as an exemplar case study in the NHS Healthcare Inequalities 2022/23 planning guidance advisory note, which says: “The analysis of the data contributed to the inequalities being cut significantly... Other systems could adopt a similar approach, making use of the Health Inequalities Improvement Dashboard (HIID).”
It goes on to say, “The total waiting list size, including disaggregation by deprivation and ethnicity, as demonstrated by this work should be included in the Key Performance Indicators to be assessed”.
The work has also attracted interest from NHS colleagues across the UK,
while the West Yorkshire Integrated Care Board has put together a business case to provide a project management resource to facilitate sharing the learning and supporting similar implementations where required across secondary care trusts.
Further enhancements include the development of a prioritisation matrix – that applies a vulnerability score at an individual patient level when considering their care pathway, and increased informatics and project support dedicated to health inequalities.
Calum MacIver adds: “A representative from the Information Team now attends monthly meetings of a learning disability group to share knowledge and gain greater understanding from key stakeholders.
“A further ripple effect is now taking place within the trust to specifically look at inequalities among asthma sufferers, and a community-based project is working with primary care stakeholders in a highly deprived area of Huddersfield, again to share knowledge and gain better understanding to influence positive health outcomes in the area.”
Innovation and collaboration
In addition to CHFT, The Health Informatics Service enables new, empowering, efficient and secure communications and IT services for clients including other health trusts, GP practices, laboratories, hospices and care charities. L

Advertisement Feature
FURTHER INFORMATION www.this.nhs.uk
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 72
Written by Nigel Wareing
Are nurses prepared for the challenges of virtual healthcare?
Equipping the modern nursing workforce for realities they face using new technologies to enhance access requires new thinking around education, writes
Professor Ann-Marie Cannaby, senior nurse and member of the clinical advisory board for BT
Virtual consultations and virtual wards have spread rapidly in the NHS since the onset of the Covid-19 pandemic. They have become a progressively important means to providing access to increasingly in-demand services. Today, clinicians continue to blend such approaches into their everyday practice.
Virtual approaches to care, in their various forms, are now regarded as an important part of NHS recovery initiatives, and also the future of technology in healthcare delivery.

And although remote care provision is not appropriate for every patient, it is likely to become a larger part of how clinical teams, as a limited resource, provide healthcare for people. As the NHS continues to deal with growing backlogs and other strains on services, this is about enabling healthcare professionals to monitor and oversee more patients, whilst also allowing the individuals in NHS care to best maintain their independence, and to live their lives outside of the hospital.
For those who work in the health technology sector, remote or virtual care provision might feel like it has been around for some time. But delivering virtual health and social care at the scale now required to cope with increasing demand and complexity of care, is still new for the NHS, and for nursing as a profession.
It is vital that healthcare professionals are appropriately equipped to practice their profession in this changing environment.
Equipping the workforce
As an experienced chief nurse, a key question for me is how we ensure the next generation of nurses are digitally ready.
Nursing education at both an undergraduate and post graduate level needs to embrace and prepare nurses for the demands and challenges we will see in the future.
Digital skills are important for more than chief information officers, digital and IT teams, and even clinical digital leaders like CCIOs or CNIOs. They are fundamental for frontline nurses to be able to deliver safe and effective care.
We need to produce modules for nurses in undergraduate courses that prepare them for the technology they will be expected to use, so they can help support patients in adopting new ways of monitoring and care. We need to give nurses the confidence to challenge and to work with their technology vendors to provide the right solutions. We need to encourage creativity in this sector. Clinicians at the frontline need to work with technology providers to cocreate and design the future of care.
How we assess and care for people virtually brings a whole new set of challenges. We might gain more timely observations, or gain more feedback about observations, movement and daily activities of patients. But clinicians may need to adapt their questioning, less proximity may require more skills. There may be more insights but caring for the person holistically should not be lost. Knowledge, practice and communication skills take years to perfect, as does the ability to instinctively know when something isn’t quite right. Nurses have been trained to observe changes in a person’s recovery, or deterioration,
based on physical interaction and often have therapeutic relationships developed in proximity. The question of how we overcome lessened social interaction and the face-toface contact that has been a fundamental part of nursing, is a significant one to tackle. How do nurses pick up on cues from patients in a virtual or remote environment? How do we overcome a potentially lessened ability to physically look and listen in virtual care environments that can be more formal? These are questions we need to address. Delivering care in new ways can help to address challenges and the evidence base in this area is growing. But our new models must allow us to maintain and improve quality of care, and to keep our patients, and their families, at the centre of our practice.
Modernising our approach to teaching
To modernise teaching to respond to these challenges, there are four core areas that need to be considered in undergraduate education and by healthcare providers. We need to increase knowledge of technology. Whether it’s machine learning, artificial intelligence, data platforms, or a whole range of other digital solutions, there is an ever-evolving health technology market of which nurses need to have an awareness. We need to enhance the skills of students for digital and technology readiness. This means training and educating with different digital technologies, and allowing students to practice with hardware and software, so that they can gain confidence.
Nurses and students need to practice augmenting their skills. We need to provide the opportunity for nurses to combine technology with their knowledge and practice. In the case of virtual consultations this might mean practising remote monitoring and feedback or monitoring long-term conditions virtually. Students, in their training, need to practice these skills. Considerations and adaptions may be required when caring for people they may not have physically met. Importantly we need to encourage curiosity for innovation – creating a culture where nurses are excited to review technologies of the future and understand the application of technologies within healthcare. Modernising our approach to education will be an ongoing process. But in doing so, we have an opportunity to better support the nursing profession at a time of rapid change in healthcare.
Recruitment and retention are not the only workforce challenges
Media headlines continue to highlight that the NHS is faced with substantial recruitment and retention challenges – with nursing often referenced. Technology may assist in enabling access and care to be provided differently. Thinking about the changing nature of professional clinical roles, and how we develop those individuals in order to create a workforce equipped with the right digital skills for a more virtual world, is therefore vitally important. L
Technology
Issue 23.1 | HEALTH BUSINESS MAGAZINE 73
Written by Dave O’Shaughnessy, Healthcare Practice Leader –Avaya International

The role of modern communications in an Integrated Care System
The NHS Integrated Care System (ICS) aims to remove existing silos between hospitals and Primary Care, physical and mental health services, NHS and council services, and instead deliver support as a joined-up health and care service from local councils, the NHS, and other partners
This approach presents healthcare providers with the opportunity to explore new service workflows and technologies as they seek to keep up with evolving patient expectation and demands.
The communications challenge
To successfully meet patient health and care needs, an ICS should consider how to best improve patient visibility and patient access across all care services in their region. Modern communications and collaboration services can potentially play a pivotal role with this. Technology solutions that can help ease the administrative burden on staff and patients are especially valuableanything that can alleviate the frustrating time-demands that get in the way of health service access and provision has to be a win.
For example, the automation of certain patient services such as management of appointments, renewal of prescriptions, servicepayments, or even some medical triaging could be beneficial for patients and hospital administrative staff. Likewise, improving clinical staff mobility using smartphones enabled with role-based communications that are integrated with a hospital’s electronic health records, will help to improve care-team reachability and ultimately improve patient-facing engagement.
Think connected
The challenge faced by ICSs is that, rather than solving pain points in isolation, they must both improve experiences at a local level and scale the solution across a whole region. They must enable secure and compliant cross-site communications and collaboration, as well as data sharing for integrated but remote multi-disciplinary teams in both primary, acute, and the wider community care area.
The answer is for healthcare providers to think connected about their communications services. When it comes to collaboration and communications, thinking connected is transformative because a well-designed system that spans the entire patient journey – before visit, during visit, after visit – has the potential to improve patient engagement and access to care, create a more satisfying patient
experience, and enable team members to focus on the delivery of great care. In addition, this kind of joined-up communications system can foster cooperation and enable consistent experiences for both patients and staff across multiple Trusts and organisations not just between healthcare provides within an ICS. An ICS that thinks connected across all its healthcare providers is not only aiming to improve patient outcomes. By using communications and collaboration services to ‘join the dots’ in practical ways between an NHS Trust and other organisations within an ICS body, duplication can be avoided which will help maximise return on investment.
Steppingstones to digital transformation
The idea of digital transformation can be daunting, especially if there is an all-or-nothing mindset. Instead, it can be helpful to take a ‘steppingstone’ approach that focuses on future-proofed, coordinated solutions that address the specific challenges currently being experienced by patients and staff. Communications and collaboration services are foundational first steps in a steppingstone approach of the digital evolution of health services and there are three key practice areas where they will help maximise the positive transformation of the patient and staff experiences and engagement:
1.Improving patient access to care
The best communications and collaboration solutions enable more compelling and engaging remote patient treatments and monitoring whilst continuing to maintain quality of care. They provide secure, reliable access to healthcare services over existing, and new, digital communication channels such as video and chatbots and allow integration and interoperability with patient data. Effortless, non-repetitive, digital data capture and organisation supports the management of administrative services such as appointments, prescriptions, testresults, and referrals, which should work in a way that suits all parties as well as provide controllable access to clinicians and specialists.
2.Creating a better patient experience
The aim is to be able to integrate digital therapeutics across a range of communications and collaboration systems and devices to create scalable, on-demand services without overwhelming staff. This involves making digital services understandable and accessible to all patients, no matter what their age or technical proficiency, and the ability to create more personalised care experiences, rooted in scientific understanding, which can be scaled cost-effectively.
3.Enabling team members to focus on great care
By removing silos and complexities from Trust-wide communications and collaboration services, inefficiencies across calendars and roles can be reduced along with resource reachability and better usage, which in turn reduces wait, diagnosis, and treatment times. At the same time, this helps maximise specialist resource utilisation for where it is needed.
Find out more about how thinking connected is enabling healthcare providers to streamline essential services, improve employee experiences, and enhance patient care by interconnecting and scaling their systems across multiple regions. Start the journey by benchmarking against industry standards to establish readiness for implementing foundational stepping stones and learn actionable insights and recommendations.
L
INFORMATION
FURTHER
https://www.avaya.com/nhs/
Advertisement Feature BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 74
999 calls with sign language
The 999 BSL service enables people with hearing or speech loss to be connected to a video call with a BSL interpreter in order to make 999 calls by video



The app and website connect 999 callers to a British Sign Language (BSL) interpreter, who can relay the conversation to the 999 call handler for all emergency services – ambulance, police, fire or coastguard.


British Sign Language is a form of sign language, which involves the use of hand movements, gestures, body language and facial expressions to communicate. It is mainly used by people who are deaf or hard of hearing.
How it works
The service is free to use and available 24/7, though users will need to be connected to the internet. 999 BSL can be used on a computer, laptop, tablet or smartphone, via the app or website. There is a 999 BSL app for iOS and one for Android and no registration is required.
Service users can use the app or website to make a call to 999, which will go through to a BSL interpreter first, who will be visible on the screen. The interpreter will then call the 999 operator through the landline and relay the conversation.
In January 2022, Ofcom set out a requirement for communications providers across the UK to make an emergency BSL service available from 17 June 2022 – 999 BSL was launched on this date. Sign Language Interactions is the sole provider of the service and is working with BT who is the wholesale supplier of the service to the telecoms industry.
How it helps
Before the service was available, people with hearing or speech loss had to use a text message service and call handlers were advised to ask fewer questions to avoid delays in organising help. Now, as reported by London Ambulance Service (LAS), handlers can ask the same questions as they would in a voice call.
The new service also enables call handlers to give deaf callers instructions on how to give CPR and research shows it is just as quick as a voice call– and takes about half the time of the text system.
Positive feedback
Paramedic Richard Webb-Stevens, who is deaf said: “This is such a brilliant innovation for the deaf community and means sign language users get the same access to emergency services as any other user.”
“If you haven’t already downloaded the 999 BSL app, please do it today – it could save your life or the life of a loved one.”
As with all emergency calls, calls made via 999 BSL are recorded and retained for 3 years – this is in case they are needed for evidence at a later date.
Sarah Clark, quality assurance manager at LAS, said: “I initially trained as a call handler and I’m passionate about helping patients and saving lives. This innovation means no deaf person is excluded. Everyone should have the same access to our services and treatment and care.
“Now deaf people get the same advice and the same instructions for helping patients. And the same chance for saving lives.” L
FURTHER INFORMATION
For further information you can visit the website: www.999bsl.co.uk
Feature Heading
Technology
EEEIssue 23.1 | HEALTH BUSINESS MAGAZINE 75
Buying cloud-based software with confidence
When the products you develop are relied upon by NHS trusts throughout the country, it’s important that the service you offer is reliable, secure and efficient, but how can you demonstrate those allimportant credentials to potential purchasers? At Asckey, we firmly believe the the answer lies in the latest evolution of G-Cloud

Trusted by the NHS
With 25-years of experience, we know a little something about cloud-based software solutions. At Asckey we provide unique IT services to a wide range of public and private sector organisations, with the majority of our clients being NHS trusts. The G-Cloud online directory provides public sector organisations such as the NHS with access to over 40,000 services and 5,000 suppliers. The front-end catalogue, ‘Digital Marketplace’, is the perfect storefront for companies like ours, offering cloud-based computing services such as hosting, software and cloud support to UK public sector organisations.
The place to be
For this reason alone, it matters that we are part of G-Cloud 13. Increasingly, NHS trusts will only deal with suppliers who are registered under a relevant government framework and G-Cloud ticks that box. In fact, although other frameworks exist for suppliers to sell service and maintenance provisions, or bespoke system software, G-Cloud is currently the only framework of its kind covering packaged and cloud-based software. Opened in 2012, the directory is managed by Crown Commercial Services, an agent for the Cabinet Office and is accessible to central government, charities, education, health, local authority, blue light services, devolved administrations and British Overseas Territories, which makes it a really influential resource to be part of.
Simple searching
Within G-Cloud 13, the framework is divided into different ‘lots’ depending what solutions each supplier offers. There are
currently four lots to choose from, covering everything from cloud hosting and software to support and end-to-end services.
You can find Asckey in Lot 2, Cloud Software. Lot 2 offers applications which can be accessed over the internet or via private network and are hosted in the cloud and includes all our fmfirst suite of products. Grouping suppliers together, speeds up the search process for trusts and ensures that it’s much easier to find the exact product to match their specifications.
Guaranteed quality
For Asckey, being part of a framework like G-Cloud is a great way for us to showcase our credentials to potential purchasers without the purchasers themselves having to spend time scouring the internet searching for a reliable, secure supplier. Although you don’t need any formal certification to be listed on G-Cloud, the search process allows purchasers to filter and see whether a company is ISO accredited. This means purchasers are only choosing between companies who they know are already meeting various measurable quality standards, so they can be confident that the products on offer are reliable and fit for purpose. At Asckey we take great pride in our ISO accreditations. We know that our integrity and capability are important not just to us but also the people we work with, so being able to showcase this within the marketplace is fantastic.
Quicker procurement
As well as information on accreditation, G-Cloud allows a supplier to input plenty of detail into their listing, including a clear description of the service, pricing
details and terms and conditions. Once an organisation has found a supplier they would like to hire, the process is simple, they complete the buying process online and can then award the contract directly, safe in the knowledge that the quality assurance piece has already been taken care of. It makes it quicker and easier to onboard new suppliers and get critical systems in place as soon as possible. The fact that all systems registered on there are cloud based and must be off-the-shelf products adds to the speed and simplicity of the process. The framework also gives trusts the flexibility to purchase services on a scalable basis, paying only for what they use and increasing or reducing the services as they need.
Let’s talk
The entire G-Cloud framework is regularly reviewed, giving purchasers the ability to change a service provider relatively easily and with minimum upheaval. It also gives them access to the latest technology and innovation, as with every refresh of the G-Cloud agreement new suppliers and new products are coming online.
Being part of G-Cloud has definitely made things clearer for us at Asckey in terms of how and where we market our products. G-Cloud 13 is the ideal solution for getting our products in front of those teams in large organisations who will really benefit from them. The fact that it makes the process fairer and more straightforward is an added bonus. Why not get in touch and let us talk you through our software solutions and how they could support your organisation? L
FURTHER INFORMATION www.asckey.com Advertisement Feature BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 76
Operating with robots
NHS Golden Jubilee has recently performed its 1,000th robotic orthopaedic joint replacement - HB looks at the hospital’s robotics programme
In November 2019, the orthopaedic team at NHS Golden Jubilee were the first in Scotland to use a Mako robot for routine total and partial knee replacement.
The Golden Jubilee University National Hospital, based in Clydebank, is one of Europe’s largest elective orthopaedic centres. In 2021-22, the centre carried out more than 30 per cent of all elective hip and knee replacements in NHS Scotland.
Benefits
Using the robots means patients get better implant accuracy, reduced soft tissue damage and reduced blood loss. In the long-term, it also means patients are less likely to need further joint replacements later in life, resulting in benefits for the NHS and the patient themselves. The robots are also helping to cut waiting times.
Talking about the milestone, consultant orthopaedic surgeon Christopher Gee, said: “It’s a huge delight to see that we’ve reached the 1,000th patient milestone and this is an accomplishment of which we should all be very proud.
“This has been a real team effort, from providing more preoperative imaging in radiography to allow us to plan the cases, to the Patient Coordination Centre organising the appointments, the theatre teams learning new equipment all the way to the surgeons carrying out the procedures.
“Having surgery is a huge moment in a patient’s life and we want to give them the best possible chance of a good outcome. A key factor in this is making sure the implants are put in as accurately as possible, ensuring they last as long as possible.
“With this increased accuracy and improved outcomes associated with robotic surgery, the hope is that the joint only needs to be replaced once in a patient’s lifetime.

“While there is of course always the potential of needing further surgery in the future, with this pioneering technology becoming more common and popular among patients, our aim is that this translates to long term and wide spread improved quality of life for patients across Scotland.”
Mako
The Mako robot enables the surgeon to implant every joint replacement in the optimal position for each individual patient based on their specific anatomy, while at the same time, reducing bone resection and soft tissue injury. The robot is able to build a virtual 3D model of the patient’s anatomy based on a pre-operative CT scan, this is then validated by live intra-operative measurements. The surgeon is able to fine-tune the position of each component so that it works best for each patient. The robotic arm is utilised to make precise bone cuts as per the surgical plan. This conserves bone and minimises soft tissue damage. On the day in December the milestone was reached, John Wishart, 80, from Houston in Renfrewshire, had a partial knee replacement, carried out with the aid of a Stryker Mako robot. John said: “The pain over the past couple of years has been horrendous, to the point that around last Christmas time I could hardly sleep, so I should get to enjoy Christmas this year without that pain.
“I did a lot of exercise in the gym with a lot of cardio work to prepare for my operation and the physiotherapist has E
Technology
Issue 23.1 | HEALTH BUSINESS MAGAZINE 77
getmeanstheUsingrobotspatients better implant accuracy, reduced soft tissue damage andbloodreduced loss
Health, Care and Lounge Furniture

With our wide range of styles and colours we can help you create the right atmosphere for your care home without compromising on comfort or safety and all our upholstered furniture is available in a range of easy to clean and hygienic fabrics or faux leathers



Please browse to see our full range or contact our sales team to discuss your requirements further

Hamilton Patient & Visitor Chairs

Bestseller
Rosehill’s bestselling The Hamilton Patient & Visitor Chairs are a high quality and durable choice for your ward or waiting room. The chairs have a profiled seat for maximum comfort and an ergonomically designed back rest with a removable seat to help for easy cleaning. Optional extras include wheels, variable seat depth cushions to ensure the correct posture for multi-patient use, armpads and filled in sides. Order

All healthcare chair orders placed before 24th Feb 2023* *Quote AUTUMN22. Applicable for payment with order only.
online at rosehill.co.uk or
call our team on 0161 485 1717
We provide a variety of furnishings including lounge chairs, high back armchairs and more which are great for a wide range of users.
told me that has really helped me post-op, because I don’t need a frame and can get around on sticks at the moment.
“Now that I’ve had this procedure at the Golden Jubilee, I’m looking forward to a full recovery and getting back to the gym.”
Rosa and Da Vinci
The hospital has three robots for orthopaedic procedures – two Mako and one Rosa.
They also have two Da Vinci robots – one for lung and one for colorectal/other procedures.
The Da Vinci robot works by inserting rods into the body which are operated by a surgeon on a separate control pad, which moves the procedure on from conventional keyhole and traditionally invasive surgery. The wristed instruments of the robot have the ability to bend and rotate better than a human hand, with more accuracy as well, which means the surgeon can operate with a steady natural motion.
Patients who received robotic surgery, reported less pain and earlier return to normal activity, as well as a shorter hospital stay. The technology enables patients to recover more quickly, and reduces the chance of complications and nerve damage during the surgery.

The Da Vinci machine also has health benefits for the surgeons involved, as they are able to perform surgery sitting down instead of bending over an operating table. This can prevent back injuries and potentially extend their working life.

NHS Golden Jubilee medical director, Dr Mark MacGregor, said: “It is testament
to the hard work and dedication of all the teams involved that we have reached this milestone of treating 1,000 patients with cutting edge robotic technology.
“We now have 5 robots as part of our robotics programme here at NHS Golden Jubilee for orthopaedics, lung cancer, colorectal and other procedures.
“By collaborating with health boards from all across the NHS Scotland, this not only has huge benefits for patients all around the country, but is providing vital support to help tackle waiting lists both now and in the future.”
FURTHER INFORMATION
Read more here.
Technology
L
The technology enables patients to recover more quickly, and reduces the chance of complications and nerve damage during the surgery
EIssue 23.1 | HEALTH BUSINESS MAGAZINE 79
Can Spend Recovery Reviews generate
a much needed
financial windfall?
Twice2much discuss how Spend Recovery Reviews, based on a ‘share of recoveries’ only, can help ease current financial pressures
investigate anomalies; evidence to support initial findings.
STAGE 3 – Recovery/Reporting
have resulted from managers having approved the same invoice at different times in the approval and payment process.
Many organisations have either not heard of Spend Recovery Reviews or do not consider that the recoveries and associated cash generated is likely to be applicable to them. With so many financial pressures on every organisation as a result of the COVID pandemic and recent inflation and energy costs surges, there has never been a more appropriate time to consider EVERY avenue for income generation.
As the cost of a review is based on a ‘share of recoveries’ with no upfront costs and limited/no internal resource requirements, undertaking a review of this type should bear serious and urgent consideration.
Twice2much specialises in ‘Spend Recovery Services’ working with finance directors, accounts payable managers and heads of audit to provide a comprehensive review of accounts payable spend.
We provide the time, resource and expertise that many in-house teams cannot justify resourcing internally.
Twice2much are an approved supplier on the Crown Commercial Service Framework RM6226, Lot 15 - Spend Analytics and Recovery Services, enabling organisations to procure this service quickly and simply, as the due diligence has already been undertaken on the procuring organisation’s behalf. Our recoveries made on behalf of clients to date demonstrate beyond doubt how we can help any client…
What does a Spend Recovery Review involve?
Our reviews enable clients to benefit from a ‘bespoke’ detailed forensic review of their organisations’ accounts payable transactions.
There are three stages to a Twice2much Spend Recovery Review:
STAGE 1 - Identification/detection
Access to £100,000’s of technology, including ‘bespoke’ analytic software and resources; access to dedicated experienced professionals; multiple-layer interrogation of transactions with suppliers; specialist expertise in reviewing supplier transactions and identifying anomalies.
STAGE 2 - Verification/validation
Expert detailed analysis of transactions at individual supplier level to validate and
Twice2much provide the system, processes and resources to recover the errors found on our clients’ behalf; flexible but targeted reporting provides significant additional benefits to clients.

A comprehensive process
Our reviews do not just identify potential duplicates but cover the whole process from obtaining data, identification and verification and include recovery from suppliers. It even includes raising all paperwork to enable processing of recoveries and comprehensive reporting.
What resources are required internally?
All reviews are carried out off-system, off-site and out of sight with a focus on ensuring minimal requirement for internal resources.
The only internal resource requirements are for the extraction of data, review of initial results and processing of refunds or corrections. Assistance is provided by Twice2much for all elements.
Why can’t we do these reviews ourselves?
The truth is you can...
You can either create or buy analytical software to find potential overpayments you may have made.
However, both scenarios require cash and time resource cost with no guarantee of any benefit and at a time when resources can be better focussed on core business services. Our reviews involving significant established analytics and expertise operate on a ‘share of recoveries’ basis with zero upfront charges, thus incentivising us to find and recover more for you with minimal need for internal time and resource costs.
A common misconception
Many people mistakenly believe that if duplicates/overpayments are found by our reviews then accounts payable are at fault because they overpaid the supplier.
In my 30+ years of experience undertaking and managing reviews of this type, this could not be further from the truth, which I have explained to many finance directors and heads of finance and audit.
Rarely are payments made to a supplier without a manager’s approval and in nearly all cases, duplicates/overpayments identified
In these difficult times, it is essential that we think less about the blame game and more about the opportunities and cash generated that can help with the challenges we are all experiencing.
Who should be considering these reviews within your organisation?
Heads of audit, heads of fraud departments, heads of finance, and heads of accounts payable or procurement are the key individuals involved in considering and procuring these types of ‘specialised’ reviews. As ‘all’ Twice2much Spend Recovery reviews are undertaken on a ‘share of savings’ basis, they are in effect selffinancing, and therefore no budget or funding is required, limiting the need for a protracted procurement exercise.

How to procure a review
Crown Commercial Services ‘Framework’ RM6226, Lot 15 - Spend Analytics and Recovery Services can be used to procure the service either by direct award or by a limited tender exercise.
Public sector organisations can procure these services directly with accredited providers like Twice2much.
Benefits?
Recoveries from our reviews effectively represent an ‘unbudgeted financial windfall’ which can be used to directly address budgetary pressures, enable the provision of additional services and/or fund additional resource requirements.
Twice2much would be happy to provide more details or discuss how we can help you generate these benefits quickly and efficiently. L
FURTHER INFORMATION
www.twice2much.com
Advertisement Feature
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 80
Printing the medtech of the future

Researchers at the University of Nottingham have recently been awarded a £6 million grant from the Engineering and Physical Sciences Research Council (EPSRC) in order to develop a toolkit for 3D printing. HB spoke to Ricky Wildman, Professor in Chemical Engineering at The University of Nottingham
The toolkit is intended to act as an instruction manual to improve the pathway from research to development and clinical adoption. Up until now, medtech industries have faced barriers in adopting 3D printing, as the materials have not been available, product development is arduous and the route to market is too long. It is hoped the toolkit will give healthcare professionals access to the latest science more quickly.
The Centre for Additive Manufacturing (CfAM) is a multidisciplinary research group at The University of Nottingham and is the recipient of the grant from the EPSRC. The group is made up of 100 researchers, PhD students and staff including biochemists, physicists and mechanical engineers, and is based in a purpose-built laboratory.
Developing the toolkit
The grant will be used by researchers to create a toolkit platform by which the materials and processes needed to 3D print medical technology and devices can be delivered on demand. Ricky said: “Our group of academics, industry partners and clinicians, are working together to identify the main challenges stopping us from delivering our advanced products (our biopill, intestinal patch, biocatalytic reactors), which in turn will tell us what steps are needed as part of our toolkit. We will then put those steps together
– screening tools, computational systems and manufacturing modalities – into a coherent ‘toolkit’ that can be rolled out to business.”
Additive Manufacturing is the technology behind creating customisable 3D objects and it works by adding layer upon layer of materials such as plastic, metal, or concrete to create smart, customisable products. The technology will be used to create highly functional, smart products for (bio)pharma, cell therapy/regenerative medicine, and (bio) catalysis, products that had been impossible to create using traditional manufacturing.
Ricky explained: “Additive Manufacturing, also known as 3D printing, is a type of manufacturing where we build up the structure layer by layer or point by point, rather than traditional methods of manufacturing where structures are created by taking material away (e.g., milling) or by forming (e.g., injection moulding).
“It was originally invented in the 1980s, developed further in the 1990s and then became widely available in the 2000s+. In the healthcare world, its most prominent uses are in the manufacture of hearing aid shells, dental aligners, and joint replacements.
“With the development of our toolkit at CfAM, we are aiming to reach the next level of product, where we incorporate advanced function: oral tablets that can deliver biomacromolecules (peptides/oligonucleotides) across the intestinal lining, an intestinal patch that will deliver stem cells to treat chronic intestinal diseases such as Crohn’s, and E
Medical equipment
Issue 23.1 | HEALTH BUSINESS MAGAZINE 81
Additive isManufacturing the behindtechnology customisablecreating 3D objects and it works by adding layer upon layer of materials
Quality & innovation
ProLine & ProLine XT
Tracheostomy tubes with an excellent realtionship between inner and outer diameter
E Thin-walled design for generous air supply
Made of tissue-friendly polyurethane (PU)
Ultra-thin polyurethane low-pressure cuff which helps to prevent microaspiration (for cuffed versions)


Swivelling 15 mm connector on all inner cannulas
Secure bayonet catch
Available with speaking option
Available with subglottic suction function (suction line perfectly embedded into tube wall)


Available in standard and extended length

Halberstadt M edizintechnik GmbH Straße des 20. Juli 1 D - 38820 Halberstadt Tel. 0049 (0) 3941 - 668 6 Fax. 0049 (0) 3941 - 245 65 www.primed-halberstadt.de primed@primed-halberstadt.de
Your specialist for medical devices in the eld of tracheostomy & laryngectomy
biocatalytic reactors for the hyperefficient local manufacture of medicines.”
Tailored devices
The end goal is to create an instruction toolkit that will be able to identify how medtech can develop personalised, tailored medtech devices. Ricky says: “Our goal is to make it easy for industry to adopt additive manufacturing, and equip them with the information needed to manufacture personalised, tailored products that can meet patient need.”
Ricky explained how the toolkit will work: “With additive manufacturing, we envision personalised, bespoke products that are tailored to each individual patient’s needs. However, one of the challenges we face in realising this and getting additive manufacturing used in clinical settings, is that industry finds it difficult to adopt the technology. One of the reasons for this is that it requires a different way of thinking – we are used to manufacturing with traditional methods.
“At the Centre for Additive Manufacturing (CfAM), we plan to get around this problem by giving adopters the instruction manual for delivering their product idea – we are developing a toolkit that will make it easy
for someone to identify what materials, how to use them, and how to manufacture with them, all with healthcare products in mind.”
It is anticipated that the toolkit can bring benefits to the health service, by bringing products to market more quickly and easily. In order to see widespread uptake across hospitals, pharmacies and the wider NHS, researchers recognise that manufacturing products embedded with advanced functionality need the capability to quickly, predictably, and reliably ‘dial up’ performance, so they are able to meet sector specific needs and specific advanced functionalities.
Benefits to the health service
Ricky set out the benefits it could bring to the NHS: “At the Centre for Additive Manufacturing, we work hard to educate industry and clinicians on the benefits of additive manufacturing / 3D printing; personalisation, on demand manufacturing, point of care, distributive manufacturing.

The goal of the NHS is of, course, to provide care to meet each and every patient’s needs – additive manufacturing offers that opportunity in areas as diverse as surgical planning, prosthetics, drug delivery and regenerative medicine. It is a technology of the future, now, and adopting it has the potential to give many more choices for treatment in the clinical arena.”
Professor Mohammad Ilyas, consultant at NHS Nottingham also added: “This is very exciting work which, through building cellular models, will improve our understanding of how the gut functions. More importantly, if successful, it will lead to a paradigm shift in clinical management and launch the use of autologous tissue engineered therapeutics for the treatment of bowel disease”
FURTHER INFORMATION
https://www.nottingham.ac.uk/
Medical equipment
L
research/groups/cfam/
Issue 23.1 | HEALTH BUSINESS MAGAZINE 83
It is a technology of the future, now, and adopting it has the potential to give many more choices for treatment in the clinical arena
AUDIO VISUAL
Market leader for telehealth solutions
AVer is dedicated to offering top-of-the-line cameras with patient-centred design and cutting-edge Artificial Intelligence, as well as optics and image processing technologies for the applications of Telehealth, Telemedicine, Tele-ICU, and OR Live Surgery Broadcast.
With over 20 years of research, development and manufacturing excellence, AVer is a proud recipient of numerous international design, innovation, application, and service awards centered on exceptional product usability, reliability and customer satisfaction, sustaining our market leadership position as a reflection of our drive to craft quality products and services. Our easy-to-use, affordable and meaningful technology
solutions coupled with our unparalleled customer support and best warranty programs, enables you to accelerate learning in the classroom and increase competitive advantage for your business. Our product portfolio is deeply rooted in exceptional customer-centric product research and design, providing you intelligent solutions with excellent value. Spanning four separate continents with 15 international offices serving over 100 countries through 700 employees worldwide, our farreaching international presence and extensive network of reliable distribution channels continue to empower us to serve our customers on a global scale with unsurpassed service and dedicated support. L
FURTHER INFORMATION
www.avereurope.com

Supporting new dads TECHNOLOGY
Working alongside the NHS, DadPad has developed a package of physical and digital resources that have been specifically written for men, to give them the knowledge and practical skills necessary to support themselves, their partner, and baby, as they transition to fatherhood.

At the same time, the healthcare professionals working with new dads will have the opportunity to build a full picture of the family dynamic, equipping them to give that new family unit the utmost in personalised support.
DadPad areas in the UK use a mixture of our ‘essential guide’ DadPad and the ‘baby basics’ Quick Read hardcopy guidebooks to engage, empower and aid assessment of each dad’s knowledge, skills and preparedness for fatherhood, alongside the DadPad app,
which provides an accessible, personalised, safe space for dad to explore information and interact with peers and health professionals alike. With this ‘fatherhood-at-yourfingertips’ app, each dad will be empowered to take ownership of his parenting journey. At the very heart of our offer is the opportunity to learn, develop and implement strategies for new fathers, so that Integrated Care Systems can provide a ‘whole family’ approach in supporting new families to parenthood. L
FURTHER INFORMATION
www.thedadpad.co.uk
ADVERTISERS INDEX The publishers accept no responsibility for errors or omissions in this free service 4c Strategies 18 Ammerhurst Replacement Keys 18 Anderson Quigley 46 Apollo UK 4 Asckey Data Services 76 Avaya 74 Aver Information Europe 12, 84 Big Dug 26 B Medical Systems IBC Cherry Products 24 Clinisys UK 64, 71 Cyber Secure Solutions 56 DadPad 84 EDM Healthcare Consulting 68, 71 Fordingbridge PLC 26 GE Healthcare IFC, 30 Giganet 52 ISS Mediclean 8 Knapman Roocroft 20 Lapcabby 54 max20 14 Murray Equipment Co 48 NG Security (UK) 58 Philips Monitors 6 Powell System Engineering 36 Powerstar 38 Primed Halberstadt Medizintechnik GmbH 82 Radar Healthcare 62 Rosehill Furnishings 78 Rubrik UK 66, 71 Secure IT 10 Sellox 16 Sign Direct 24 The Health Informatics Service 72 Twice2much 80 Upcycled Medical 42 Veolia ES (UK) 40 Yewdale Corporation 28 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 84



DEDICATED TO IMPROVING OCCUPATIONAL HEALTH & SAFETY STANDARDS Find out more www.healthandsafetyevent.com 25-27 April 2023, NEC Birmingham UK Lead Media Partner: Co-located with: